Explore Any Narratives
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
On a Tuesday afternoon in late March 2024, in a lab at the Cancer Centre at Illinois, Hua Wang watched a data stream confirm a stubborn problem in immuno-oncology was cracking open. The challenge was dendritic cells—the sentinels of the immune system—and their frustrating reluctance to process mRNA-encoded tumor antigens efficiently. The solution, published in *ecancermedicalscience*, wasn't a new chemical compound. It was a sponge. A macroporous hydrogel designed not for passive diffusion, but for active recruitment. It worked. This specific moment of validation, documented in a research paper, is a direct thread leading to 2026, a year now pinpointed by industry leaders like BioNTech as a "catalyst-rich" period for a medical revolution that began with a pandemic shot.
The narrative of mRNA technology is undergoing a violent and productive rewrite. It is shedding its identity as a mere vaccine platform for infectious diseases and being recast as a modular, rapid-response system for human repair. The calendar year 2026 is emerging not as a distant future, but as a concrete horizon for a cluster of clinical and technological readouts that will define the next decade of medicine. We are tracking a triple convergence: the expansion of mRNA into cancer and genetic diseases, the refinement of delivery through methods like microneedles, and the compression of development timelines by artificial intelligence. The journey from a COVID-19 vaccine to a personalized cancer immunotherapy is shorter than most assume, and it runs directly through 2026.
The profound lesson of the COVID-19 vaccines was logistical, not just biological. We learned that the same core platform—lipid nanoparticles carrying messenger RNA—could be rapidly reprogrammed. Swap out the genetic code for the SARS-CoV-2 spike protein for the code for a melanoma antigen or a missing metabolic enzyme, and the factory line theoretically remains the same. This is the modular promise. By 2026, this promise is expected to materialize in late-stage clinical pipelines. The applications are breathtakingly broad: cancer immunotherapies, protein replacement for rare genetic disorders like Crigler-Najjar syndrome, regenerative medicine for tissue repair, and even as a delivery vehicle for CRISPR gene-editing tools.
But the path from a vaccine that teaches the body to recognize a foreign virus to a therapy that reprograms it to fix an internal error is fraught with new engineering challenges. Vaccines need a strong, transient signal to alert the immune system. Therapeutics often require precise, controlled, and sometimes sustained protein expression. "The shift from prophylactic vaccines to therapeutics necessitates a fundamental rethinking of delivery and dosing," explains a senior scientist from a leading mRNA therapeutics firm, who spoke on background due to competitive sensitivities. "It's no longer just about generating an immune response. It's about providing a corrective function with minimal off-target effects, which is a far more delicate operation."
This is where research like Hua Wang's hydrogel breakthrough becomes critical, especially for cancer. A major reason therapeutic cancer vaccines have historically struggled is that dendritic cells, which must present tumor antigens to killer T-cells, are inefficient at gathering and processing those antigens from conventional vaccines. Think of it as a postal system where most letters get lost. Wang's team engineered a biomaterial scaffold that actively recruits these crucial dendritic cells to the vaccination site, dramatically increasing the chance they will grab the mRNA instructions and present the right target.
According to the published research, "this active recruitment strategy resulted in markedly higher mRNA-dendritic cell encounter rates compared to conventional methods, leading to enhanced T-cell activation and a stronger antitumor response in preclinical models."
The platform doesn't just wait for immune cells to wander by; it calls them in for a direct briefing. This kind of adjuvant technology—enhancing the *delivery system* rather than the payload itself—is a key trend for achieving efficacy in complex diseases. It transforms the vaccine from a broadcast message into a targeted, high-priority memo.
The first-generation mRNA workhorse is a linear strand. Next-generation constructs are already in the pipeline, designed to be more potent, longer-lasting, and stealthier. Two variants are particularly significant for the 2026 outlook.
Self-amplifying RNA (saRNA) contains genes not only for the target antigen but also for a viral replicase. Once inside a cell, it creates copies of itself, leading to much greater protein production from a far smaller dose. This could enable single-shot vaccines for diseases that currently require multiple boosts and reduce manufacturing costs per dose. Circular RNA (circRNA) lacks the free ends that make linear RNA vulnerable to rapid degradation by cellular enzymes. It’s a closed loop, granting it extraordinary stability and the potential for more durable protein expression, which is vital for therapeutic applications. It also tends to fly under the radar of innate immune sensors, reducing inflammatory side effects.
Delivery is evolving in parallel. While lipid nanoparticles (LNPs) remain the dominant vehicle, research is intensifying on alternatives like lipoplexes and polyplexes for different tissue targets. Inhaled mRNA nanoparticles for pulmonary diseases are in active development. And then there are microneedles.
Microneedle patches—arrays of microscopic needles that painlessly penetrate the top layers of skin to deliver a payload—have been a promising concept for years. They offer potential advantages: no cold chain requirement (a game-changer for global health), elimination of needle phobia and sharps waste, and possible self-administration. For mRNA, the skin is a target-rich environment, teeming with immune cells ideal for vaccination.
Yet, as of early 2025, the specific 2026 breakthrough trajectory for microneedles appears less about radical new needle design and more about their successful integration with the fragile mRNA molecule. The challenge is stabilizing the mRNA on the patch during storage and ensuring efficient release into the skin. The research focus has prioritized making the mRNA payload work within this established delivery method. A successful mRNA microneedle product by 2026 would represent a major logistical victory, but it hinges on formulation science, not micromechanical innovation.
"The true innovation isn't the needle array itself," says a biomedical engineer specializing in drug delivery. "It's the formulation of the mRNA payload into a stable, dry-state matrix that can be reconstituted by skin interstitial fluid and then efficiently translated. That's the hidden chemistry determining success or failure."
While headlines imagine AI designing drugs from scratch, its near-term, transformative role in the mRNA space is as a hyper-efficient optimization engine. Designing an mRNA sequence isn't just about the code for the protein. It's about tweaking the untranslated regions, the nucleoside modifications, and the codon usage to maximize protein yield, stability, and immunogenicity while minimizing unwanted immune reactions. This is a multivariate optimization problem of staggering complexity.
Artificial intelligence, particularly machine learning models trained on vast datasets of sequence and outcome data, can iterate through these possibilities at a speed impossible for human researchers. According to industry analyses, this can slash early-stage mRNA design and optimization timelines by up to 70%. This doesn't just make things faster; it makes better candidates more likely to be found. An AI can test millions of virtual constructs in silico before a single test tube is used, predicting which will have the optimal properties.
This acceleration directly feeds the 2026 pipeline. Candidates that might have taken two years to optimize and enter preclinical testing can now be ready in months. It is the silent, digital force compressing the entire development timeline, making the rapid-response modular platform truly rapid.
The stage is set. The foundational science is transitioning into applied medicine. The funding mechanisms, like the CELLSCRIPT™ 2026 mRNA Research Advancement Awards (offering ten grants of $10,000 product value, with winners announced by January 31, 2026), are priming academic pumps. But this forward momentum exists in a political and regulatory landscape that is far from stable. The path to 2026 is not just one of scientific breakthroughs, but of navigating evidence, policy, and public trust. The next part of this story examines the converging timelines, the concrete players, and the substantial headwinds that could accelerate or stall the vaccine revolution.
Science operates on a different calendar than politics. In the meticulous world of clinical trials, 2026 is a fixed coordinate, a year when multiple late-stage studies will deliver definitive answers. In the volatile arena of public health funding, 2026 is a cliff edge. The tension between these two realities—between the linear progression of research and the cyclical chaos of policy—will determine whether the promise of this medical moment is fulfilled or fractured. We are not merely waiting for data; we are watching a collision.
The most audacious application of mRNA technology may be its assault on HIV. The IAVI G004 Phase 1 trial, which began vaccinations in 2024, is a masterclass in immunological chess. It uses Moderna's mRNA platform not to directly induce antibodies against the mercurial HIV virus, but to execute a "germline-targeting" strategy. The goal is to coax the immune system, through a series of precisely engineered mRNA shots delivered via lipid nanoparticles, to produce the vanishingly rare broadly neutralizing antibodies that can block a wide spectrum of HIV strains.
Think of it as a multi-year training regimen for the immune system. The first shots prime specific, naive B-cells. Subsequent booster shots, with slightly modified mRNA instructions, guide those cells to mature and refine their antibody production. The entire 2026 timeline hinges on the data from this sequential approach. Early results have noted safety signals like skin reactions, a reminder that powerful immune modulation carries real, if manageable, risks. The ultimate test, planned for later this decade, is a "treatment interruption" study: can this mRNA regimen control HIV replication in infected individuals without daily antiretroviral therapy?
"The germline-targeting approach is a paradigm shift," explains a virologist involved in the trial. "We're not asking the immune system to hit a moving target with one perfect shot. We're giving it the blueprints and the time to build a master key."
This represents a fundamental expansion of the mRNA concept. It is no longer a simple message saying "make this viral protein." It is a sophisticated, multi-part instruction manual for engineering a bespoke immune weapon. Success here would validate mRNA as a platform for complex immune engineering far beyond simple prophylaxis.
While HIV represents a global health moonshot, the mRNA war on cancer is already being fought on multiple, personalized fronts. Prostate cancer vaccines like CV9103 and CV9104 have blazed a trail, combining mRNA-encoded tumor-associated antigens with checkpoint inhibitors. The logic is brutal and elegant: use the mRNA to paint a target on the cancer cells, then remove the immune system's brakes so it can attack. A January 2026 review in NPJ Vaccines underscores the ongoing challenges—antigen selection, the immunosuppressive tumor microenvironment—but frames them as engineering problems, not dead ends.
The potential payoff is not just measured in tumor shrinkage. It is quantified in national economies and in tens of thousands of living, breathing people. A sobering report from the Center for Infectious Disease Modeling and Analysis (CIDMA) at the Yale School of Public Health, led by Professor Alison Galvani, put a staggering number on the opportunity cost of inaction.
"mRNA vaccine platforms represent an extraordinary convergence of clinical promise and societal value. Our results show that sustained investment could dramatically reduce cancer mortality and avert medical costs," said Alison Galvani, director of CIDMA and Professor of Epidemiology at Yale School of Public Health.
The numbers are not subtle. The Yale analysis projects that effective mRNA therapeutic vaccines for just four aggressive cancers—pancreatic, renal cell carcinoma, non-small cell lung cancer, and metastatic melanoma—could prevent approximately 49,000 deaths annually in the United States alone. The economic impact is even more eye-watering: over $75 billion in direct and indirect costs averted every single year. This isn't just a medical journal abstract; it's a fiscal and moral argument for a massive, sustained research mobilization.
But who is paying for the mobilization? Here the narrative fractures. While BioNTech talks of a "catalyst-rich" 2026 and academic awards like the CELLSCRIPT™ mRNA Research Advancement Awards (with ten winners receiving $10,000 in product value to be announced by January 31, 2026) provide crucial seed funding, the federal pipeline in the United States has sprung a catastrophic leak.
In 2023, the U.S. Department of Health and Human Services canceled an $800 million federal funding initiative for next-generation mRNA COVID-19 vaccine research. The ripple effects of that decision now threaten to swamp the entire field. The National Foundation for Infectious Diseases (NFID) has explicitly warned that this and other policy shifts have "eroded trust" in the Advisory Committee on Immunization Practices (ACIP) and left the nation vulnerable.
"The decision to cancel that funding wasn't just a budget line item," argues a former NIH program director who requested anonymity. "It was a signal to the entire biotech ecosystem. It said that the strategic urgency of the pandemic is over, and mRNA is back to being just another research area fighting for scraps. That signal has a chilling effect on early-stage investment and talent retention."
The NFID frames 2026 as a year where "evidence-based policy matters more than ever," specifically highlighting the risk to preparedness for threats like avian influenza. The subtext is clear: the infrastructure built for COVID-19—the rapid clinical trial networks, the manufacturing partnerships, the regulatory pathways—is decaying. The very platform that could deliver a pandemic-stopping bird flu vaccine in months is being undermined by political complacency.
Is this the inevitable boom-and-bust cycle of biomedical funding, or a unique failure of political vision? The contrast is jarring. On one hand, you have meticulously planned trials aiming to deliver landmark data in 2026. On the other, you have a policy environment actively dismantling the foundation that makes such trials possible. The Yale report doesn't mince words, warning of "devastating health and economic consequences" from the funding cuts.
Amidst the high-stakes drama of HIV trials and cancer cures, a quieter revolution in logistics is taking shape. Experts consistently point to 2026 as a pivotal year for microneedle array patches. Their value proposition is less about biological breakthrough and more about systemic enablement. They promise thermostability—removing the brutal -80°C cold chain requirement—and painless, minimally trained administration.
The real breakthrough, however, may be geopolitical. Gavi, the Vaccine Alliance, emphasizes that microneedle patches, often discussed alongside mRNA, are key to building "regional production ecosystems." The goal is not just a better delivery device, but a redistribution of power.
"The combination of mRNA's flexible platform and microneedle patches' logistical simplicity enables regional manufacturing sovereignty," notes a vaccine access expert from Gavi. "It reduces aid dependency. A clinic in sub-Saharan Africa could hold a year's supply of multiple vaccine antigens in a small, solar-powered fridge, or even without refrigeration at all. That changes everything."
This is the less glamorous, more profound horizon for 2026. It's not just about what the vaccine does in the body, but about who controls its journey to the patient. Can a technology born in Western biotech hubs truly democratize global health? The microneedle patch, coupled with mRNA, represents a test case. Success means moving from a model of charity to one of local capability.
Yet, skepticism is warranted. The history of global health is littered with "miracle" technologies that failed to scale due to cost, complexity, or intellectual property barriers. Will mRNA-filled microneedle patches be any different, or will they simply become another premium product for wealthy health systems? The 2026 timeline will reveal whether the companies driving this technology are prioritizing scalable, equitable access or protected profit margins.
Here is the contrarian observation: for all the talk of AI-driven trials revolutionizing the field by 2026, the current evidence is strikingly thin. The enrichment data for this article found no verifiable breakthroughs, specific studies, or expert quotes directly linking AI to the design or execution of major vaccine clinical trials in this timeframe. The promise is ubiquitous in industry white papers—AI will optimize patient recruitment, predict endpoints, analyze imaging data. But where are the named trials? The published results?
The most concrete application remains in the pre-clinical space: using machine learning to optimize mRNA sequence design for stability and protein expression, shaving months off development. This is vital, but it is not the same as an "AI-driven trial." The grandiose vision of AI selecting patient cohorts in real-time or dynamically adapting trial protocols feels, for 2026 at least, more like marketing hype than imminent reality. The hard graft of clinical research—patient consent, regulatory filings, blinding, data monitoring—remains a profoundly human and bureaucratic endeavor.
Perhaps the true AI story of 2026 will be one of absence. The focus, rightly, is on the biological and logistical challenges: making the vaccines work, making them stable, and getting them to people. The algorithm can wait. The immunology cannot.
So what are we left with as we look toward this pivotal year? A series of concrete experiments—in HIV, in cancer, in delivery, in manufacturing—running headlong into a fog of political and financial uncertainty. The science has a schedule. Does the will to support it? The final part of this analysis will judge the players, weigh the critiques, and look beyond the 2026 horizon to see what endures.
This is not merely a story about a few clinical trials. The year 2026 represents a fundamental stress test for an entire model of medical progress. The converging timelines for mRNA vaccines, microneedle patches, and even the overhyped promise of AI, are probing the limits of our systems: our regulatory agility, our commitment to equitable access, and our willingness to fund science that saves lives and money. The outcome will signal whether the 21st-century biomedical ecosystem—forged in the emergency of COVID-19—can transition into a sustainable engine for chronic and complex diseases. The legacy will be measured not in press releases, but in whether pancreatic cancer survival rates bend, whether HIV functional cures become plausible, and whether a child in a remote clinic receives a shelf-stable vaccine from a patch.
The cultural impact is subtler but just as profound. We are witnessing the normalization of genetic medicine. The public's encounter with mRNA began with a pandemic shot framed as a necessary, novel emergency tool. By 2026, the conversation shifts to its use as a programmable therapeutic for cancer, a personalizable treatment. This moves the technology from the realm of public health mandate into the intimate space of chronic disease management. It transforms mRNA from a foreign concept into a standard tool in the oncologist's armamentarium. That shift in public perception—from fear of the new to expectation of the effective—is a prerequisite for the next wave of genetic therapies.
"What we are seeing is the maturation of a platform from a pandemic response vehicle into the backbone of a new therapeutic modality," observes a venture capitalist specializing in biotechnology. "The companies that navigate 2026 successfully won't just have positive data; they will have validated a business model for personalized, off-the-shelf genetic medicines. That's what the market is waiting to see."
The historical parallel is not the polio vaccine, but the monoclonal antibody. Once a rare, complex, and astronomically expensive technology, it was refined, industrialized, and is now a standard treatment for dozens of conditions from cancer to autoimmune disease. 2026 is the year mRNA seeks to prove it can follow that same path from miraculous novelty to medical mainstay.
For all the justified optimism, a clear-eyed view demands skepticism. The first critique is one of overpromise. The biotech and pharmaceutical industries, fueled by investor capital, have a notorious habit of extrapolating early-phase success into guaranteed blockbuster drugs. Not every mRNA cancer vaccine will be a CV9104. The germline-targeting HIV approach is elegant but remains a high-risk, high-reward gamble; Phase 1 safety data is a far cry from functional cure data. The microneedle patches face not just technical formulation hurdles, but the brutal economics of manufacturing at scale. The narrative of 2026 as a "catalyst-rich" year could easily give way to 2027 as a year of sobering readouts and failed primary endpoints.
A more profound criticism centers on equity. The Yale report's staggering figures—49,000 lives and $75 billion potentially saved annually—are calculations based on U.S. data. The implicit assumption is that these therapies, once proven, will be available within the wealthy healthcare systems that funded their development. What is the plan for renal cell carcinoma patients in Lagos or Hanoi? The mRNA platform, born in a global pandemic with an explicit goal of worldwide vaccination, now risks retreating into the lucrative silo of oncology, where treatments routinely carry price tags in the hundreds of thousands of dollars.
The cold chain problem may be solved technically by microneedle patches, but the "cold chain of inequity"—the systemic barriers of cost, patents, and infrastructure—remains fully operational. Will the companies leading this charge, like Moderna and BioNTech, commit to the tiered pricing and technology transfer agreements necessary for global benefit? Or will 2026's breakthroughs simply widen the medical divide between the Global North and South? The ethical burden here is immense, and the track record of the pharmaceutical industry offers little reassurance.
Finally, there is the distraction of shiny objects. The focus on AI as a buzzworthy accelerant can pull attention and resources from the mundane, unglamorous, and absolutely critical work of scaling up lipid nanoparticle production, stabilizing formulations, and training regulatory agencies on how to evaluate these complex products. Chasing the algorithm while the factory floor is underfunded is a recipe for failure.
The immediate future is etched in calendars and clinical trial registries. The announcement of the CELLSCRIPT™ award winners by January 31, 2026, will spotlight the academic research poised to fill the pipeline in the latter half of the decade. Later in 2026, expect interim data readouts from the IAVI G004 HIV trial, offering the first real glimpse of whether the germline-targeting strategy is eliciting the desired immune responses. BioNTech has explicitly marked 2026 for key milestones in its oncology pipeline, likely involving its proprietary FixVac platform and iNeST personalized cancer vaccine candidates. These are not vague hopes; they are scheduled events that will generate concrete, binary data.
My prediction, based on the trajectory and the obstacles, is one of bifurcation. By the end of 2026, the field will have split into clear winners and stalled projects. We will see one or two mRNA cancer therapeutic vaccines demonstrate unequivocal, practice-changing survival benefits in specific, biomarker-defined cancers, likely melanoma or lung cancer. These will be fast-tracked for approval and become the new standard of care, accompanied by the inevitable $200,000-per-year price tag debates. Simultaneously, the logistical promise of microneedles will hit a snag—not a scientific one, but a manufacturing scalability issue that pushes widespread adoption another five years down the road.
The policy story will grow darker. The $800 million funding cut will be seen in retrospect as the first symptom of a broader retreat from public investment in biomedical preparedness. The next pandemic scare—be it avian influenza or Disease X—will find the U.S. apparatus rusted and slow to respond, triggering a frantic and wasteful scramble to rebuild what was deliberately dismantled.
And the patient? For a select few, 2026 will be the year a personalized mRNA vaccine, designed from their tumor's genetic sequence, becomes a covered treatment option. For millions of others, it will be another year of waiting, hoping the science outruns the politics, the economics, and the inertia.
Back in that Illinois lab, Hua Wang’s hydrogel sponge sits at a crossroads. It is a brilliant solution to a discrete problem—the dendritic cell bottleneck. Its fate, and the fate of the thousands of similar breakthroughs in labs worldwide, now depends on forces far beyond the bench: funding committees, regulatory reviewers, corporate boardrooms, and the fragile consensus that saving lives is a priority worth paying for. The science has given us a tool of almost magical flexibility. The year 2026 will reveal whether we have the wisdom, and the will, to use it.
Your personal space to curate, organize, and share knowledge with the world.
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
Connect with others who share your interests. Create and participate in themed boards about any topic you have in mind.
Contribute your knowledge and insights. Create engaging content and participate in meaningful discussions across multiple languages.
Already have an account? Sign in here

AI transforms healthcare in 2026, detecting hidden tumors, predicting diseases before symptoms, and personalizing treatm...
View Board
Major 2025 trials reveal no effective treatments for long COVID brain fog, forcing a shift from cognitive training to im...
View Board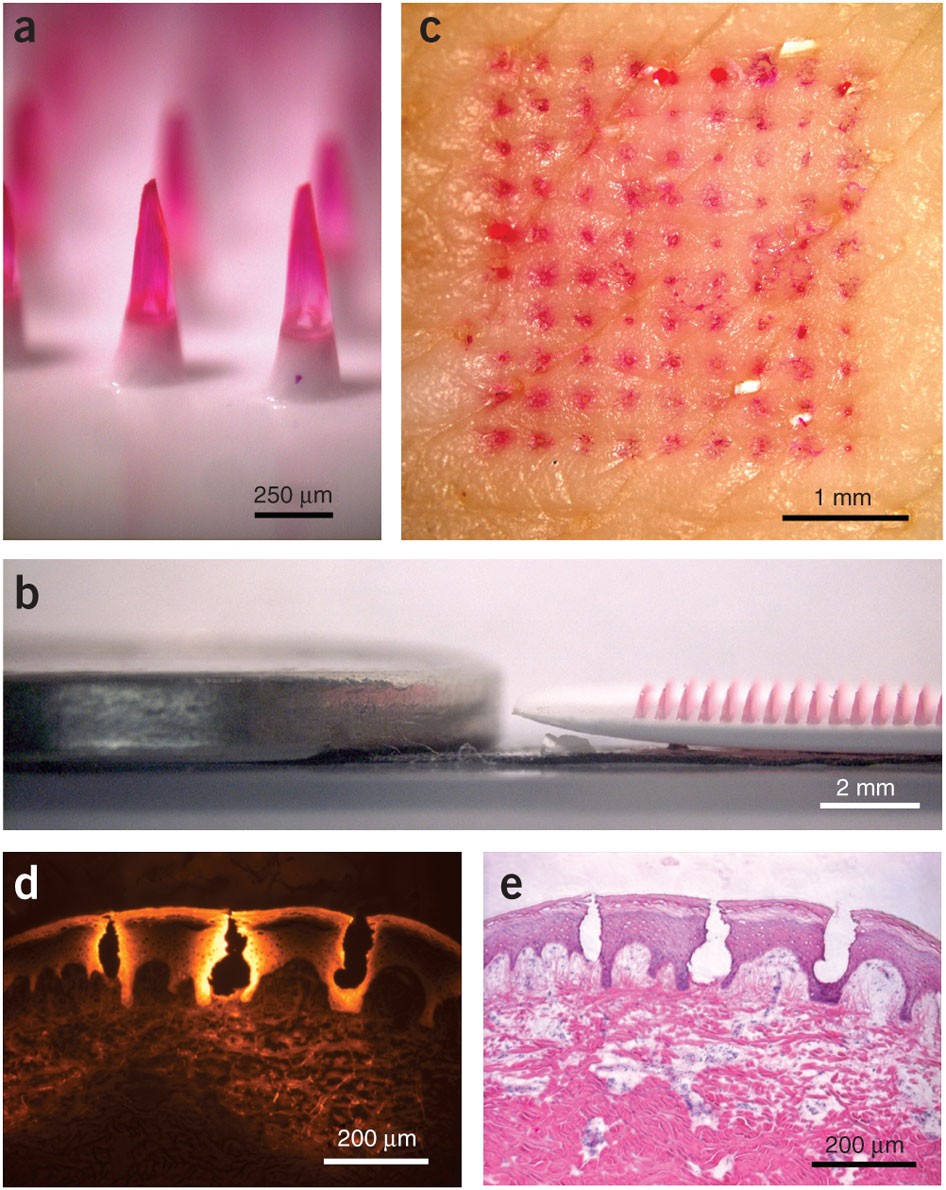
Microneedle patches deliver painless, effective vaccines via skin, revolutionizing global healthcare with self-administr...
View Board
AI revolutionizes medical physics, crafting precise radiation plans in minutes, transforming diagnostics, and reshaping ...
View Board
Discover how Sir Ronald Ross revolutionized malaria understanding! Learn about his groundbreaking discovery of mosquito ...
View Board
Discover how AI is revolutionizing the fight against antibiotic-resistant superbugs. Learn about AI-driven drug discover...
View Board
Scientists reverse blood stem cell aging with lysosomal inhibitors and RhoA blockers, restoring regenerative capacity an...
View Board
MIT chemists synthesize verticillin A after 55 years, unlocking a potential weapon against fatal pediatric brain tumors ...
View Board
Discover Karl Landsteiner's groundbreaking work on blood groups (ABO & Rh), revolutionizing transfusions. Learn about hi...
View Board
Pancreatic cancer's sugar-coated shield uncovered: Researchers reveal how tumors exploit sialic acid to deceive immune c...
View Board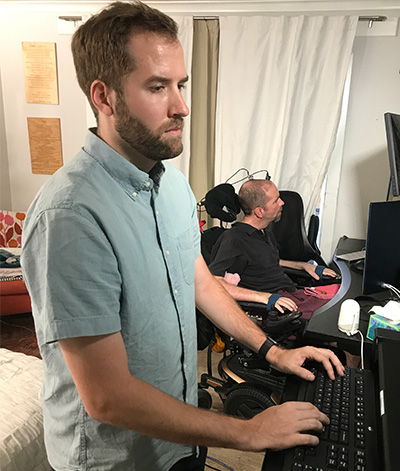
Brain-computer interface breakthroughs create thought-controlled prosthetics, restoring motor control & realistic touch....
View Board
ZDoggMD transforms medical burnout into viral rap satire, exposing systemic flaws while building direct‑care models that...
View Board
Cancer research reaches new heights as ISS microgravity enables breakthroughs like FDA-approved pembrolizumab injections...
View Board
The open AI accelerator exchange in 2025 breaks NVIDIA's CUDA dominance, enabling seamless model deployment across diver...
View Board
Autonomous AI agents quietly reshape work in 2026, slashing claim processing times by 38% overnight, shifting roles from...
View Board
Depthfirst's $40M Series A fuels AI-native defense against autonomous AI threats, reshaping enterprise security with con...
View Board
Scientists capture influenza virus invading a human cell in real-time using groundbreaking ViViD-AFM microscopy, reveali...
View Board
Microsoft's Copilot+ PC debuts a new computing era with dedicated NPUs delivering 40+ TOPS, enabling instant, private AI...
View Board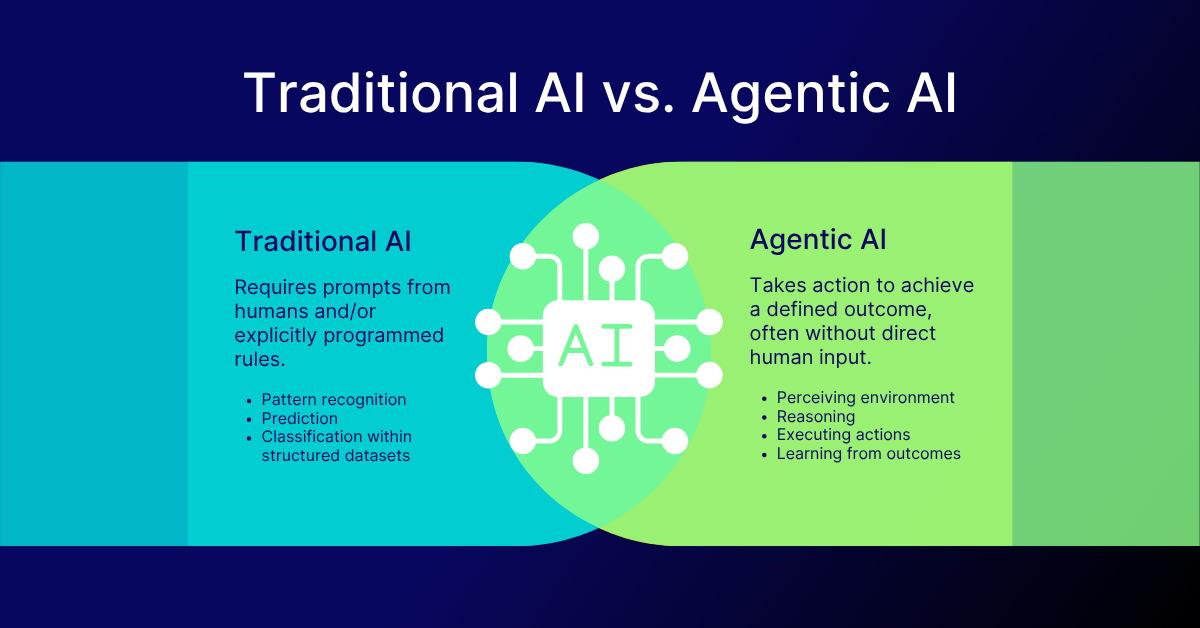
AI-driven networks redefine telecom in 2026, shifting from automation to autonomy with agentic AI predicting failures, o...
View Board
Linh Tran’s radical chip design slashes AI power use by 67%, challenging NVIDIA’s dominance as data centers face a therm...
View Board
Comments