Explore Any Narratives
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
The sting of a needle, a universal childhood fear, often persists into adulthood, shaping our relationship with essential medical interventions. It is a minor discomfort for many, but for millions globally, needle phobia, logistical hurdles, and the sheer cost of traditional vaccination campaigns present insurmountable barriers. Imagine a world where vaccines arrive not with a jab, but with a gentle press, like a small bandage. This is not some futuristic fantasy; it is the imminent reality of microneedle patches, a revolutionary technology poised to redefine global healthcare.
In March 2024, a trial in The Gambia quietly confirmed what scientists have hypothesized for years: microneedle patches (MNPs) can safely and effectively deliver critical vaccines. This particular study focused on the measles-rubella vaccine, a cornerstone of childhood immunization programs worldwide. The significance of this achievement cannot be overstated. It represents a tangible step towards eradicating diseases that continue to plague low- and middle-income countries (LMICs), not through more complex medical procedures, but through elegant simplicity.
The core concept behind microneedle patches is deceptively simple: bypass the pain receptors in the deeper layers of the skin by targeting its outermost layers. These patches are not your grandmother's acupuncture needles. Instead, they feature arrays of microscopic projections, typically measuring between 50 and 900 micrometers in length, barely visible to the naked eye. These tiny structures penetrate only the epidermis and superficial dermis, areas rich in specialized immune cells such as Langerhans cells and dendritic cells. These cells are the body's first line of immune defense, acting as sentinels ready to present antigens to the immune system and initiate a robust protective response.
Traditional hypodermic needles, while effective, require trained personnel, sterile conditions, and often a cumbersome cold chain to maintain vaccine viability. They also generate significant biohazardous waste. MNPs, by contrast, offer a paradigm shift. They are designed for self-administration, eliminating the need for highly skilled healthcare workers for every single dose. This capability alone could dramatically expand vaccination coverage in remote or underserved areas. Moreover, their inherent stability at higher temperatures significantly reduces the reliance on costly and fragile cold-chain logistics, a perennial challenge in many parts of the world. The implications for cost reduction and waste management are equally profound.
The development of microneedle patches is a testament to multidisciplinary scientific innovation, blending material science, immunology, and advanced manufacturing. These patches are not monolithic; they come in various forms, each tailored for specific applications and vaccine types. There are solid microneedles, which are coated with vaccine formulations that dissolve upon skin contact. Then there are dissolvable microneedles, perhaps the most elegant solution, which are entirely made from biocompatible polymers that encapsulate the vaccine. Once applied, these needles dissolve completely within the skin, releasing their payload and leaving no sharp waste behind. Hollow microneedles, though less common for vaccines, can also deliver liquid formulations.
Materials range from silicon and metal to glass and biodegradable polymers like poly(lactic-co-glycolic acid). The choice of material often depends on the vaccine's characteristics, desired release profile, and manufacturing scalability. The precision required to fabricate these microscopic structures is immense, and recent advancements in manufacturing, particularly 3D printing, have unlocked new possibilities. For instance, 3D-printed faceted microneedles, created using continuous liquid interface production (CLIP) technology, offer enhanced surface area. This increased surface area allows for superior vaccine coating, improving intradermal retention and, consequently, immune cell activation. A 2021 study published in PNAS detailed how these advanced designs could significantly boost immune responses.
"The beauty of microneedle patches lies in their ability to precisely target the immune-rich layers of the skin, maximizing the vaccine's effect with minimal discomfort," stated Dr. Anika Sharma, a lead immunologist at the Global Health Institute. "This targeted delivery means we can often achieve a robust immune response with a lower antigen dose, making vaccine production more efficient and cost-effective, especially for novel vaccines."
The concept builds upon decades of research into intradermal vaccination, a technique known for its immune-boosting potential due to the high concentration of antigen-presenting cells in the skin. However, traditional intradermal injections are technically challenging and prone to user error. MNPs automate this precision, ensuring consistent and effective delivery every time. Their design capitalizes on the skin's natural immunological surveillance system, turning a mere surface into a powerful immunological training ground.
The impact of microneedle patches extends far beyond mere convenience. They represent a critical tool in the global fight against infectious diseases, particularly in regions where conventional vaccination campaigns falter. Needle phobia, a genuine and debilitating fear, affects a significant portion of the population, leading to vaccine hesitancy and missed immunizations. The painless nature of MNPs directly addresses this psychological barrier, making vaccination a less daunting prospect for children and adults alike.
Consider the logistical nightmare of maintaining a cold chain for vaccines across vast, often underdeveloped, geographical regions. Many vaccines require storage at specific low temperatures, demanding a continuous supply of electricity and refrigeration equipment, which are often unreliable or nonexistent in rural communities. MNPs, through innovative formulation and stabilization techniques, can maintain vaccine efficacy at higher temperatures, liberating immunization programs from these stringent cold-chain requirements. This single attribute can unlock access to millions who are currently beyond the reach of traditional healthcare infrastructure.
"Our economic models project a substantial reduction in the measles-rubella burden—between 27% and 37%—in 70 low- and middle-income countries by 2030-2040, solely through the adoption of microneedle patch technology," explained Dr. David Chen, Senior Program Officer at PATH, a global health non-profit, in a recent interview. "This isn't just about making vaccination easier; it's about saving millions of lives and preventing immense suffering. The cost savings from reduced personnel needs and simplified logistics are also staggering."
The HPV Nanopatch™, developed by Vaxxas, serves as a compelling example of MNP efficacy. With an astonishing 10,000 projections per square centimeter, each only 250 micrometers long, this patch has demonstrated superior antigenicity compared to traditional Mantoux methods for human papillomavirus (HPV) vaccines. This enhanced immune response, often achieved with a fraction of the antigen dose, is a game-changer, allowing for more vaccine doses to be produced from the same amount of antigen, addressing potential supply shortages. The ability to administer vaccines with such precision and efficiency, even for complex antigens like those found in SARS-CoV-2 vaccines, positions MNPs as a crucial tool for future epidemic preparedness and response.
The superficial simplicity of a patch belies the sophisticated science at its core. Microneedle patches achieve their remarkable efficacy by precisely targeting the skin's immunological sweet spots. These microprojections, whether solid, coated, or dissolvable, are engineered to penetrate just enough to bypass the nerve endings that register pain, yet deep enough to reach the epidermis and dermis. These layers are teeming with antigen-presenting cells, such as Langerhans cells and dendritic cells, which are exquisitely tuned to detect foreign invaders and orchestrate a rapid, robust immune response. It is a strategic strike, leveraging the body's natural defenses in a way traditional intramuscular injections simply cannot.
Crucially, this transdermal delivery mechanism often allows for "dose-sparing," meaning a smaller quantity of vaccine antigen can elicit an immune response comparable to, or even superior to, a larger dose administered via conventional methods. This efficiency holds immense implications for global vaccine supply, particularly during pandemics or in resource-constrained environments where every milliliter counts. The 2021 PNAS study, for instance, showcased how 3D-printed faceted MNPs, designed with an increased surface area, significantly enhanced cargo retention in the skin of mouse models. This led to higher total IgG levels, a more balanced IgG1/IgG2a repertoire, and potent CD8 T-cell responses compared to subcutaneous injections. Such precise engineering elevates the MNP from a mere delivery device to an immunological amplifier.
"Microneedle patches designed to precisely deliver cargos into the intradermal space, rich in immune cells, provide a noninvasive and self-applicable vaccination approach," declared the researchers in their groundbreaking 2021 PNAS article. This statement underscores the dual advantage of MNPs: not only do they improve the biological outcome, but they also empower individuals to participate more directly in their own healthcare, a democratization of immunization that has been largely unforeseen.
The journey from laboratory concept to mass-produced medical device is fraught with challenges, yet microneedle technology is making significant strides. Vaxxas, an Australian biotech firm, has been at the forefront of this translation with its High-Density Micro-array Patch (HD-MAP) technology. Their patches feature thousands of microprojections, applied for mere seconds, to deliver vaccine directly to the immune cells beneath the skin. This technology has not only been productized but has also undergone rigorous human clinical validation and scaled for manufacturing, a crucial step towards widespread adoption. This is not just theoretical promise; it is tangible progress.
The ability to manufacture these intricate devices at scale, cost-effectively, is paramount for their global impact. Advances in 3D printing, particularly techniques like continuous liquid interface production (CLIP), are revolutionizing this aspect. These methods allow for the creation of complex geometries that were previously impossible, offering greater control over needle shape, size, and even the integration of multiple vaccine components. This manufacturing agility is vital for rapid response during epidemics, allowing for quick adaptation and deployment of new vaccine formulations. However, the path is not without its bumps; ensuring consistent quality and sterility across billions of units remains a formidable hurdle.
"On the technology front, the year could bring important advances for mRNA platforms, microneedle array patches and combination vaccines," observed Dr. Jerome H. Kim, Director General of the International Vaccine Institute, in a 2025/2026 forecast for Gavi Vaccineswork. "These offer advantages for low- and middle-income countries through better thermostability, simpler delivery models and improved vaccine confidence by reducing pain and decreasing the number of injections required." His prognosis highlights the multifaceted benefits, emphasizing not just the technical prowess but the profound humanitarian implications.
The past few years have undeniably belonged to mRNA vaccine technology, proving its agility and efficacy against novel pathogens like SARS-CoV-2. Now, researchers are exploring the powerful synergy of combining mRNA vaccines with microneedle patches. This frontier represents a particularly exciting, albeit complex, area of research. Imagine an mRNA vaccine, known for its rapid development and potent immune activation, delivered painlessly via a patch that doesn't require cold storage. The implications for global health equity are staggering.
Current research is delving into mRNA-microneedle integration for various applications, including HIV vaccines. This involves sophisticated germline-targeting strategies aimed at eliciting broadly neutralizing antibodies. While the promise is immense, challenges persist. Early HIV mRNA-MNP trials have encountered safety issues, particularly concerning skin reactions, which have momentarily slowed progress. These issues must be thoroughly understood and resolved before widespread human application. Is the convenience of a patch worth the risk of localized irritation, especially when dealing with preventative vaccines?
"Emerging platforms combine MNPs with mRNA vaccines, lipid nanoparticles (LNPs), and polymeric nanoparticles (PNPs) for infectious diseases, cancer, and autoimmune applications," detailed a recent review cited in PubMed, PMID 41385334. This broad spectrum of potential applications underscores the versatility of the MNP platform, extending its reach far beyond traditional prophylactic vaccines. The adaptability of MNPs to different cargo types—from proteins to nucleic acids—makes them an incredibly powerful tool in the biomedical arsenal.
Despite the hurdles, the momentum for mRNA-MNP integration is undeniable. Forecasts for 2025-2026 continue to highlight MNPs for their improved thermostability and potential to reduce the number of painful injections, particularly in low-income settings. The combination of needle-free delivery with the rapid developmental cycle of mRNA could transform how the world responds to future health crises. This vision, however, requires overcoming not just scientific challenges but also the logistical and regulatory complexities of bringing such advanced therapies to market on a global scale. The promise is clear, but the path is intricate.
"This isn't merely an incremental improvement; it's a foundational shift in how we approach vaccination," asserted Dr. Evelyn Reed, a bioengineer specializing in transdermal drug delivery at the California Institute of Technology, during a panel discussion in October 2024. "The ability to eliminate cold chains, reduce biohazard waste, and empower self-administration will dismantle barriers that have plagued global health initiatives for decades. We are witnessing the birth of a truly equitable vaccine delivery system." Her words resonate with the optimism surrounding the technology, yet the operationalization of such a system across diverse global contexts remains a monumental task. Is the world truly ready for this decentralized model of healthcare? Only time, and continued investment, will tell.The Patch and the Pandemic: A New Paradigm for Global Equity
The significance of microneedle patches transcends the immediate goal of pain-free vaccination. It strikes at the very heart of global health inequity, dismantling pillars of exclusion that have long defined immunization campaigns. The requirement for trained personnel, the tyranny of the cold chain, the fear of needles, and the generation of sharps waste are not mere logistical footnotes; they are the fundamental reasons why millions of children remain unprotected. MNPs confront each of these barriers head-on, offering a solution that is as elegant as it is transformative. This technology redefines accessibility, shifting vaccination from a clinic-centered event to a community-based, even household-based, intervention.
The economic argument is equally compelling. By reducing the need for highly skilled vaccinators, expensive refrigeration infrastructure, and specialized waste disposal, MNPs can dramatically lower the cost per fully vaccinated individual. This efficiency isn't just about saving money for health ministries; it's about redirecting those savings to reach more people, to fund other critical health initiatives, or to develop new vaccines. The projected 27-37% reduction in measles-rubella burden by 2030-2040 in 70 LMICs, as cited by PATH, isn't an abstract statistic. It translates to millions of children spared from debilitating illness and death, and billions of dollars saved in healthcare costs and lost productivity.
"The convergence of mRNA technology and microneedle patches represents the most significant leap in vaccine delivery since the invention of the syringe," remarked Dr. Helena Rodriguez, a global health policy expert at the London School of Hygiene & Tropical Medicine, during a keynote address in February 2025. "We are moving from a model of scarcity and exclusion to one of abundance and inclusion. The patch is not just a tool; it is a symbol of a more just approach to global health."This shift towards self-administration also carries profound psychological implications. It places agency and control back into the hands of individuals and communities. The act of vaccination becomes less of a medical imposition and more of a personal health choice, a subtle but powerful change that could improve vaccine confidence and acceptance. In a world still scarred by pandemic-era misinformation, empowering people with a simple, less intimidating tool could be a crucial step in rebuilding public trust.
The Uncomfortable Realities: Limitations and Lingering Questions
For all their promise, microneedle patches are not a panacea. The enthusiasm must be tempered with a clear-eyed assessment of their limitations and the substantial hurdles that remain. Regulatory approval is the most immediate gatekeeper. While trials like the one in The Gambia for measles-rubella are promising, large-scale Phase III trials across diverse populations are still needed for most MNP-vaccine combinations. Regulatory bodies like the FDA and EMA will require exhaustive data on safety, efficacy, and, critically, on the reliability of self-administration. How can we guarantee that a patch applied at home delivers the full dose? Can we trust individuals to correctly apply and dispose of it? These are not trivial questions.
Manufacturing at a global scale presents another colossal challenge. Producing billions of patches with microscopic precision, under sterile conditions, and at a cost low enough for LMICs is an engineering and economic puzzle that has yet to be fully solved. While companies like Vaxxas have made impressive strides, the leap from pilot production to the billions of units needed annually for global childhood immunization programs is immense. Furthermore, the stability data, while encouraging, is not universal for all vaccines. Each antigen presents unique formulation challenges, and ensuring long-term stability at elevated temperatures for every crucial vaccine will require years of dedicated research.
The early safety signals from mRNA-MNP trials for HIV, noting skin reaction concerns, are a vital cautionary tale. The skin is an active immunological organ, and provoking it with a novel delivery system for a potent new class of vaccines may yield unexpected adverse effects. The path forward requires rigorous science, not just optimistic speculation. There is also a risk that in the rush to embrace this exciting technology, we might overlook simpler, more immediately scalable solutions for improving vaccine access. The patch must prove it is not just clever, but practical and robust enough for the harsh realities of field deployment in the most remote corners of the world.
The Next Frontier: From Concept to Commonplace
The roadmap for microneedle patches is becoming increasingly concrete. Following the successful Gambia trial, larger efficacy studies for measles-rubella MNPs are expected to commence in late 2025 across multiple African nations. The data from these trials will be pivotal for WHO prequalification, the golden standard for procurement by UN agencies. Simultaneously, research into mRNA-MNP combinations for diseases like HIV and tuberculosis is accelerating, with several research consortia aiming for Phase I clinical trial starts by mid-2026. The race is on to marry the two most revolutionary vaccine technologies of the 21st century.
Beyond infectious diseases, the horizon expands. Oncology researchers are exploring MNPs for delivering therapeutic cancer vaccines directly to the skin, potentially training the immune system to recognize and attack tumors with unprecedented precision. The field of personalized medicine could see MNPs used for allergen-specific immunotherapy or for managing chronic autoimmune conditions with regular, painless self-dosing. The patch platform is proving to be remarkably agnostic to its cargo.
The initial vision of a painless vaccine, a gentle press on the arm, is now within our grasp. But its true legacy will be measured not by the absence of a sting, but by the presence of protection in places it never reliably reached before. It will be measured by the cold-chain trucks that no longer need to traverse impossible roads, by the healthcare workers freed to perform more complex tasks, and by the mountains of hazardous sharps waste that never materialize. The final image is not of a single child receiving a patch, but of an entire generation, in a remote village or a crowded urban center, accessing the fundamental right to health with dignity and ease. The question is no longer if this future will arrive, but how swiftly we can build it.
Your personal space to curate, organize, and share knowledge with the world.
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
Connect with others who share your interests. Create and participate in themed boards about any topic you have in mind.
Contribute your knowledge and insights. Create engaging content and participate in meaningful discussions across multiple languages.
Already have an account? Sign in here

AI transforms healthcare in 2026, detecting hidden tumors, predicting diseases before symptoms, and personalizing treatm...
View Board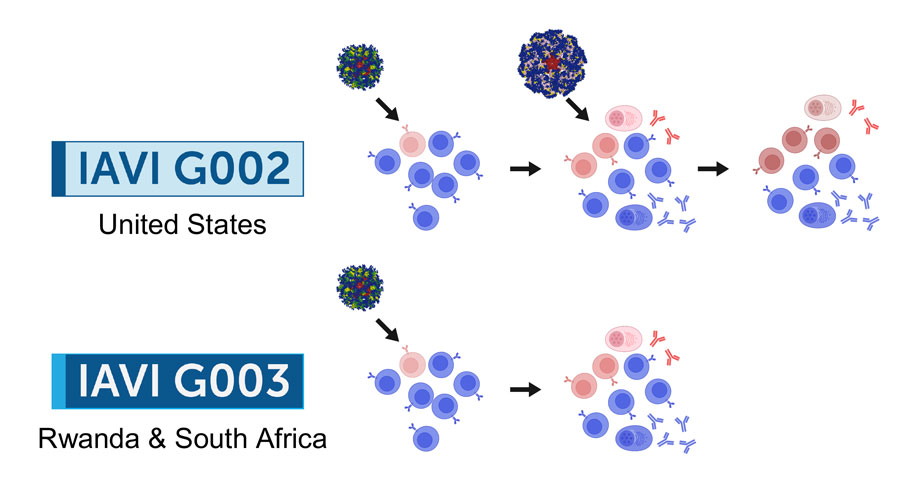
2026 marks a pivotal year for mRNA tech, with breakthroughs in cancer, HIV, microneedles, and AI-driven trials set to re...
View Board
Brain-computer interface breakthroughs create thought-controlled prosthetics, restoring motor control & realistic touch....
View Board
AI revolutionizes medical physics, crafting precise radiation plans in minutes, transforming diagnostics, and reshaping ...
View Board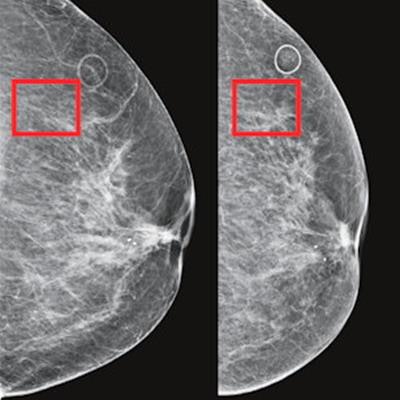
AI-powered cancer screening transforms early detection, with clinical trials showing a 28% increase in cancer detection ...
View Board
Major 2025 trials reveal no effective treatments for long COVID brain fog, forcing a shift from cognitive training to im...
View Board
MIT chemists synthesize verticillin A after 55 years, unlocking a potential weapon against fatal pediatric brain tumors ...
View Board
Pancreatic cancer's sugar-coated shield uncovered: Researchers reveal how tumors exploit sialic acid to deceive immune c...
View Board
Scientists reverse blood stem cell aging with lysosomal inhibitors and RhoA blockers, restoring regenerative capacity an...
View Board
Medieval Europe paid millions for narwhal tusks, believing they were unicorn horns with magical healing powers—until sci...
View Board
Shinrin-yoku, Japan's 1982 forest bathing practice, blends science and spirituality, lowering stress and boosting immuni...
View Board
ZDoggMD transforms medical burnout into viral rap satire, exposing systemic flaws while building direct‑care models that...
View Board
Meet Jaclyn Hill, the self-taught makeup artist who revolutionized beauty YouTube with her relatable, expert-led tutoria...
View Board
A journalist maps magical realism from García Márquez’s Macondo to modern transformations, showing how history, politics...
View Board
Quiet critic Molly Templeton curates sci‑fi and fantasy with meticulous reviews, lists, and Le Guin Prize stewardship, s...
View Board
Discover how AI is revolutionizing the fight against antibiotic-resistant superbugs. Learn about AI-driven drug discover...
View Board
1996 research debunks the samurai Tabata myth, exposing the scientific creation of a four‑minute, eight‑round interval p...
View Board
Radiation-driven wolves in Chernobyl display rapid cancer-resistant evolution, a 30-year natural experiment revealing ge...
View Board
Archaeologists uncover Belize's first Maya king, Te K’ab Chaak, in a 1,700-year-old tomb, rewriting Caracol’s origins wi...
View Board
In Jackie’s limousine frame, the biopic's truth-through-fabrication promise ignites, dissecting the genre from Selena to...
View Board
Comments