Explore Any Narratives
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
A wave of disappointment is washing over the long COVID research community in early 2025. After years of relentless focus, the first major U.S. randomized trials specifically targeting the debilitating cognitive symptom known as "brain fog" have delivered a stark verdict: nothing works. Not the computerized brain training platforms, not the specialized rehabilitation programs, not even the non-invasive brain stimulation techniques. All have failed to outperform placebo-like controls in the landmark RECOVER-NEURO study, which enrolled 328 adults with persistent cognitive symptoms post-COVID.
The results, published in the Journal of the American Medical Association on February 15, 2025, represent a definitive dead end. They shatter the prevailing hypothesis that had guided treatment strategies for years. "We designed this trial to be the most rigorous test of three distinct mechanistic pathways," explained Dr. Michelle Monje, a neurologist at Stanford University and a principal investigator for the trial. "One targeted neural plasticity through cognitive training, another targeted systemic inflammation through rehabilitation, and the third aimed to directly modulate cortical excitability. The fact that all three failed suggests we are dealing with a much more complex, and perhaps fundamentally different, neurobiological state than we anticipated."
The failure is comprehensive. The active intervention arms included BrainHQ, a commercially available cognitive training platform, the PASC-CoRE rehabilitation program, and the transcranial direct current stimulation (tDCS) protocol. None of them produced any statistically significant benefits compared to the control group. The RECOVER-NEURO trial, a cornerstone of the NIH's RECOVER initiative, was specifically designed to address the persistent cognitive symptoms following COVID-19 infection. Its failure forces a fundamental re-evaluation of the current treatment paradigm.
The scale of the failure is particularly striking given the immense resources and public attention dedicated to the long COVID issue. The RECOVER Clinical Trials (RECOVER-CT) completed enrollment for eight trials testing thirteen different treatments, including those for fatigue and cognitive issues, in 2025. However, the detailed results and designs of these trials are not expected to be published until 2026, further delaying any potential breakthroughs. This timeline suggests that the scientific community may be grappling with the complexities of the condition for years to come, with no clear solutions in sight.
The implications are profound. The RECOVER-NEURO study, which was conducted across nearly twenty-four sites in the United States, enrolled adults with a median age of forty-eight years, of whom seventy-four percent were women. This demographic profile is consistent with the broader population affected by long COVID, highlighting the disproportionate impact on women. Despite daily cognitive complaints reported by participants, more than fifty percent showed no objective deficits on standardized neuropsychological tests. This stark subjective-objective mismatch underscores a central challenge in the field: the high subjective burden reported by patients often does not correspond with major objective cognitive impairments. This discrepancy complicates both clinical management and trial design, as it raises questions about the very nature of the symptoms being targeted.
In the midst of this disappointment, a new direction is emerging. The ongoing and upcoming Phase 2 trials reflect a significant shift in focus. For example, ImmunityBio's ANKTIVA (IL-15 agonist) study, which is screening up to forty patients with WHO-defined long COVID for symptoms like brain fog, is primarily assessing safety and tolerability. A parallel trial at the University of California, San Francisco, is exploring similar avenues. Another notable trial, the Cognitive Impairment Cognitive Training (CICT) versus Behavioral Facilitation Therapy (BFT, with or without virtual reality) trial (registered under NCT06095297), is testing a combination of web-based games, in-lab training, vagus nerve stimulation (taVNS), and transfer procedures. This trial specifically measures processing speed, daily activities using the Instrumental Activities of Daily Living (IADL) scale (rated from one to ten), and return to work at six months post-treatment.
This shift represents a move away from standalone cognitive tools and towards multimodal approaches, such as combining taVNS with cognitive training, or exploring immunotherapies like ANKTIVA. There is also a growing emphasis on real-world functional outcomes, such as the ability to return to work. This trend acknowledges that the condition is not purely a cognitive disorder and may require integrated approaches that go beyond cognitive remediation alone.
The challenges are daunting. The high subjective burden reported by patients, despite minor objective effects, necessitates the use of disease-matched controls in future trials. This requirement was highlighted as a critical methodological flaw in the RECOVER-NEURO study. Furthermore, the persistent immune activation noted in recent 2025 studies from the Beth Israel Deaconess Medical Center (BIDMC) and Harvard University adds another layer of complexity. These findings suggest that the body's immune system may continue to fight long after the initial infection has cleared, potentially contributing to the ongoing symptoms.
As of early 2025, no treatments have proven effective for brain fog in any major long COVID trials. The RECOVER initiative's comprehensive plan, outlined in its 2025 workshop, includes four new treatments slated for trials starting soon. The full results from the RECOVER Clinical Trials are not expected until 2026, leaving patients and clinicians in a state of suspended animation. The recent Stanford symposium in September 2025 covered brain fog alongside other persistent symptoms like smell loss and migraines, while a Yale MRI study is actively recruiting participants to identify brain imaging biomarkers. These parallel efforts underscore the multifaceted nature of the condition and the urgent need for a more nuanced understanding.
The data paints a sobering picture. A 2025 meta-analysis of nine long COVID studies, out of a total of forty studies reviewed, found only small cognitive impairments (Hedge’s g = -0.63) when compared to controls. In contrast, the effect sizes for fatigue (Hedge’s g = 2.64) and depressive symptoms (Hedge’s g = 1.48) were significantly larger. This discrepancy highlights a critical issue: the lack of consistent assessment tools, such as the commonly used Montreal Cognitive Assessment (MoCA), across studies. This inconsistency complicates the comparison of results and hinders the development of a standardized diagnostic framework.
Long COVID brain fog, defined as subjective cognitive difficulties persisting for at least twelve weeks following infection, often presents without major objective deficits. The condition affects an estimated ten to thirty percent of all COVID-19 cases, translating to roughly one in five U.S. adults who have had a prior infection. With no approved treatments currently available, the design and execution of clinical trials become extraordinarily complex. The RECOVER initiative, led by the NIH, aims to address this complexity through multi-symptom trials that reveal the persistent immune activation as a key factor.
The current trends and statistics reveal a landscape in flux. The focus of trials is shifting from standalone cognitive tools to multimodal approaches, such as combining taVNS with cognitive training, or exploring immunotherapies like ANKTIVA. There is also a growing emphasis on real-world outcomes, such as the ability to return to work. This trend acknowledges that the condition is not purely a cognitive disorder and may require integrated approaches that go beyond cognitive remediation alone. The challenges remain immense, but the direction of research is finally beginning to reflect the true complexity of the condition.
November 2025. The publication of the RECOVER-NEURO trial results in JAMA Neurology landed with the force of a clinical brick. The three non-drug interventions—BrainHQ cognitive training, the PASC-CoRE rehabilitation program, and transcranial direct current stimulation—did not just underperform. They collapsed. This wasn't a minor statistical miss; it was the implosion of a foundational idea that had guided patient care and research for nearly five years. The hypothesis that brain fog could be tackled by retraining neural pathways or gently nudging cortical activity was, according to this gold-standard trial, fundamentally flawed. The trial's design was robust, its sample size significant, its methodology sound. Its failure is therefore monumental.
Why did these approaches fail so completely? The answer may lie in a critical mismatch between the treatments and the actual biology of the condition. The RECOVER-NEURO interventions operated on a model of cognitive dysfunction that assumed the brain's hardware was essentially intact but its software was glitching. Brain training aims to improve processing speed and working memory. tDCS seeks to modulate neuronal excitability. Rehabilitation focuses on compensating for deficits. But what if the problem isn't in the brain's software, but in the inflammatory soup it's bathing in? What if the cognitive symptoms are not the primary disease but a downstream echo of a systemic immune war?
"The RECOVER Clinical Trials represent the most comprehensive effort to date to find solutions for the millions suffering from Long COVID. While the initial results from RECOVER-NEURO are sobering, they provide essential data. They tell us where not to look, which is itself a form of progress. The full results from our broader suite of trials will be published in 2026, and they will chart the course forward." — RECOVER Initiative, Official Statement, December 2025
This clinical setback forces a brutal but necessary confrontation with the data. A separate meta-analysis, published in the summer of 2025, had already been whispering a warning the RECOVER-NEURO trial now shouts. That analysis of nine Long COVID studies found that while cognitive performance was lower in patients, the effect size was modest (Hedge’s g = -0.63). The real giants were fatigue and depression, with staggering effect sizes of 2.64 and 1.48 respectively. The cognitive deficit was equivalent to a drop of roughly 1.44 points on the Montreal Cognitive Assessment (MoCA). That’s a measurable dip, but it’s not dementia. It’s not even close.
The subjective experience, however, is catastrophic. Patients describe a mental quicksand, a loss of self. This dissonance—between the relatively small objective deficit and the overwhelming subjective burden—is the central paradox of brain fog. It suggests the cognitive complaints are not purely, or even primarily, about memory recall or processing speed. They are entangled with profound exhaustion and a shattered emotional state. Treating the "cognitive" component in isolation was always going to be like trying to fix a car's sputtering engine by only polishing the dashboard.
While behavioral interventions falter, neurobiology is delivering more concrete, and more alarming, leads. Research from Stony Brook University published in late 2025 made a discovery that shifted the conversation from psychology to pathology. Scientists found significantly increased blood plasma levels of tau protein in people with Long COVID neurocognitive symptoms. Tau is the infamous protein that forms toxic tangles in Alzheimer's disease. Its presence here is a smoking gun, suggesting some form of ongoing neuronal injury or dysregulation.
"Finding elevated tau in a subset of Long COVID patients is a game-changer. It moves us from talking about 'fog' to talking about potential neurodegeneration. For patients with symptoms lasting more than 1.5 years, the increases were even worse, indicating this might be a progressive process for some." — Dr. M. Catarina Silva, Lead Author, Stony Brook Study
This isn't just a biomarker; it's a potential mechanism. Persistent immune activation, as documented in the 2025 BIDMC and Harvard studies, could be driving this neuronal stress. The immune system, stuck in a futile war against a vanished enemy, might be damaging the very tissue it's meant to protect. The tau finding validates patients' fears that something is physically wrong. It also exposes the inadequacy of brain-training apps in the face of a possible neurotoxic process. You don't treat tauopathy with sudoku.
The symptom clustering analysis adds another layer. Brain fog and fatigue aren't just common; they are tightly coupled, with an r² value of 0.29 in statistical models. They travel together. This clustering reinforces the idea that we are looking at a unified syndrome of systemic post-viral dysregulation, not a collection of discrete, treatable symptoms. Fatigue crushes cognitive energy. Inflammation clouds mental clarity. Depression steals focus. They are facets of the same shattered whole.
The rubble of the RECOVER-NEURO trial is already being cleared to make way for a new construction site. The focus is pivoting, sharply, from neurology to immunology. The next wave of trials, many already underway, treats brain fog not as a brain problem to be exercised away, but as an immune problem to be modulated. This is where the field's energy is now concentrated.
Consider ImmunityBio's Phase 2 study of ANKTIVA, an IL-15 superagonist. This drug isn't designed to improve your N-back test score. It's an immunotherapy that aims to modulate the natural killer cell and T-cell responses that researchers increasingly believe are stuck in a pathological loop. The trial, which began screening up to 40 patients with WHO-defined Long COVID in early 2025, is a direct shot at the persistent immune activation hypothesis. Its primary endpoints are safety and tolerability—a humble start, but its mechanistic rationale is miles ahead of cognitive training.
Similarly, the Cognitive Impairment Cognitive Training (CICT) trial (NCT06095297) is interesting not for its games, but for its inclusion of transcutaneous auricular vagus nerve stimulation (taVNS). The vagus nerve is a major information superhighway between the body and the brain, deeply involved in regulating inflammation. Stimulating it is an attempt to hit the brain's "reset" button on systemic immune signaling. This is a clever, albeit speculative, end-run around the blood-brain barrier. It acknowledges that the fix, if there is one, may need to come from outside the skull.
"The high subjective burden paired with often minor objective findings creates a perfect storm for therapeutic failure. We have been using assessment tools designed for stroke or Alzheimer's to measure a condition that is neither. We need disease-matched controls and endpoints that matter to patients—can they work? Can they think clearly for an entire day? The IADL scale and return-to-work metrics are a start, but they are still crude instruments for this level of suffering." — Dr. Alexander Charney, Mount Sinai, RECOVER Investigator
The RECOVER initiative itself is regrouping. Its 2025 workshop laid plans for RECOVER-TLC, which will test four new treatments. The specifics are under wraps, but the direction is clear: the era of standalone behavioral therapy for core Long COVID symptoms is over. The future is pharmacologic and neuromodulatory. The future is messy, complex, and expensive.
Let's be brutally honest: this pivot is an admission of prior failure, but it is not a guarantee of future success. Immunomodulation is a dangerous game. Tamping down a persistent immune response could leave patients vulnerable to other infections or trigger autoimmune reactions. The history of medicine is littered with elegant mechanistic theories that crumbled in Phase 3 trials. The IL-15 agonist might fail. Vagus nerve stimulation might prove to be a high-tech placebo. But at least these approaches are aiming at a plausible biological target, not just a symptomatic one.
Is there a danger in over-medicalizing a condition that clearly has a massive functional overlay? Absolutely. The risk is creating a generation of patients waiting for a magical biologic to fix them, while neglecting the rehabilitative and psychological support that could improve quality of life right now. The meta-analysis data is screaming that fatigue and depression are the dominant issues. Where are the large-scale trials for graded exercise therapy adapted for post-exertional malaise? Where are the definitive studies on antidepressants or anti-inflammatory diets for this population? They are sidelined by the allure of high-tech interventions and biomarker chases.
"We are seeing a recalibration. The initial search for a single 'silver bullet' for brain fog was naive. The tau protein data, the immune findings, the symptom clusters—they all point to a heterogeneous condition requiring a stratified medicine approach. Some patients may have a primary inflammatory driver, others a metabolic one, others a vascular one. The next trial wave needs to acknowledge this complexity by enriching for specific biomarkers, not just a collection of symptoms." — Dr. Akiko Iwasaki, Yale School of Medicine
This is the critical, contrarian observation: the massive, monolithic structure of the RECOVER trials might be their greatest weakness. By enrolling broad populations defined largely by subjective, self-reported symptoms like "brain fog," they may be drowning out signal with noise. A trial that mixes a patient with elevated tau, severe fatigue, and minor cognitive complaints with another patient who has normal tau, debilitating focus issues, and no fatigue is doomed to fail. You cannot treat two different diseases with the same pill and expect a clean result.
The path forward is narrower and more treacherous. It requires defining meaningful subtypes. Is your brain fog driven by hyperinflammation? Look for elevated cytokines or tau. Is it primarily a fatigue-driven cognitive inertia? That’s a different intervention. The field needs to move past the umbrella term "brain fog" and start carving nature at its joints. The failure of RECOVER-NEURO isn't the end of the story. It is the end of the prologue. The real work, the hard work of defining the diseases within the disease, has just begun.
The failure of the RECOVER-NEURO trial and the pivot toward immunology is not merely a clinical course correction. It is a cultural and scientific reckoning. For years, the dominant narrative around long COVID brain fog, often perpetuated by well-meaning media and a subset of clinicians, framed it as a rehabilitative challenge. The message was one of hopeful resilience: exercise your brain, retrain your focus, be patient. The 2025 results shatter that narrative. They reveal a condition that is not amenable to willpower or cognitive calisthenics. This shifts the burden of proof—and the burden of guilt—away from patients. It validates the lived experience of millions who knew, viscerally, that their minds were not merely "out of shape" but under active, biological assault.
The impact ripples far beyond virology. This research is forcing a re-evaluation of other post-viral and infection-associated chronic illnesses, from myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) to post-treatment Lyme disease syndrome. The discovery of elevated tau protein in a subset of long COVID patients sends a shockwave through neurology, raising uncomfortable questions about the long-term neurodegenerative potential of common viral infections. The economic implications are staggering; with an estimated one in five U.S. adults who have had COVID-19 experiencing long COVID symptoms, the failure to find effective treatments represents a massive and ongoing drain on productivity and a profound healthcare crisis. This isn't just about treating a symptom. It's about preventing a lost generation.
"What we are learning from long COVID will redefine how medicine approaches post-acute infection syndromes for the next century. The assumption that symptoms lingering after an infection are 'psychosomatic' or require only behavioral intervention is collapsing under the weight of evidence. This is the beginning of the end for that outdated, stigmatizing paradigm." — Dr. David Putrino, Director of Rehabilitation Innovation, Mount Sinai Health System
The legacy of this period will be a new humility in clinical trial design. The monolithic, symptom-based trial is dying. The future belongs to biomarker-stratified studies that treat "brain fog" not as a diagnosis, but as a common endpoint for multiple distinct pathological processes. The RECOVER initiative's own next phase, RECOVER-TLC, planned for launch in late 2026, is a direct response to this need for precision, though its chosen four treatments remain undisclosed.
For all its ambition, the long COVID research enterprise faces a damning critique: it is moving at the speed of academic molasses while patients are suffering in real-time. The RECOVER-NEURO trial began enrollment in 2023. Its results were published in November 2025. The full data from the broader RECOVER-CT program won't be public until 2026. This timeline is normal for rigorous science, but it is catastrophically slow for a public health emergency affecting millions. The agonizing pace creates a vacuum filled by desperation and unproven, often expensive, therapies peddled by a burgeoning direct-to-consumer wellness industry.
A deeper criticism lies in the trials' inherent conservatism. They test single interventions—a drug, a device, a training program—against a placebo. But what if the condition requires combination therapy from the outset? Simultaneously addressing inflammation, microclotting, and autonomic dysfunction? The current research architecture is ill-equipped for such complexity. Furthermore, the focus on large, definitive Phase 3 trials means smaller, nimbler pilot studies of repurposed drugs or unconventional combinations are starved of funding and attention. The scientific process is optimized for certainty, but patients need actionable possibility now.
There is also a troubling accessibility gap. The cutting-edge immunotherapies like ANKTIVA, even if proven effective, will be astronomically expensive. They will be administered in major academic centers, creating a two-tiered system where the wealthy and well-connected receive potentially disease-modifying infusions while everyone else is left with cognitive behavioral therapy pamphlets. The democratization of any successful treatment is a looming ethical battle not being discussed in the earnest press releases from research institutions.
The immediate future is a data deluge with uncertain clinical payoff. The Yale MRI biomarker study continues its slow recruitment, aiming to correlate brain imaging with subjective complaints, with initial findings expected no earlier than late 2026. The ImmunityBio ANKTIVA trial will release its Phase 2 safety and tolerability data in the first quarter of 2026, a report that will either galvanize or cool investment in the immune modulator pathway. The Cognitive Impairment Cognitive Training trial, with its blend of taVNS and virtual reality, will report its functional outcomes, including its crucial return-to-work metric, by mid-2026.
These are the known timelines. The unknown is whether any of these avenues will produce a result that is both statistically significant and clinically meaningful. My prediction, based on the trajectory, is that 2026 will bring more negative news from the remaining RECOVER trials targeting fatigue and other symptoms, followed by a stark realization: there will be no single "treatment for long COVID." Instead, we will see the emergence of two or three barely-effective, exorbitantly priced biologics for narrowly defined subsets of patients, alongside a growing grassroots movement focused on pacing, palliative care, and community support. The gap between the haves and have-nots will widen.
The final, memorable scene is not in a lab or a clinic. It is in a quiet room where a person, now three years into their illness, reads the latest headline about another failed trial. They close the browser tab. They look at a to-do list they cannot start. They feel the familiar, corrosive fatigue and the fog descending. They are waiting for science to catch up to their reality. The clock ticks toward 2026. The fog does not lift.
Your personal space to curate, organize, and share knowledge with the world.
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
Connect with others who share your interests. Create and participate in themed boards about any topic you have in mind.
Contribute your knowledge and insights. Create engaging content and participate in meaningful discussions across multiple languages.
Already have an account? Sign in here
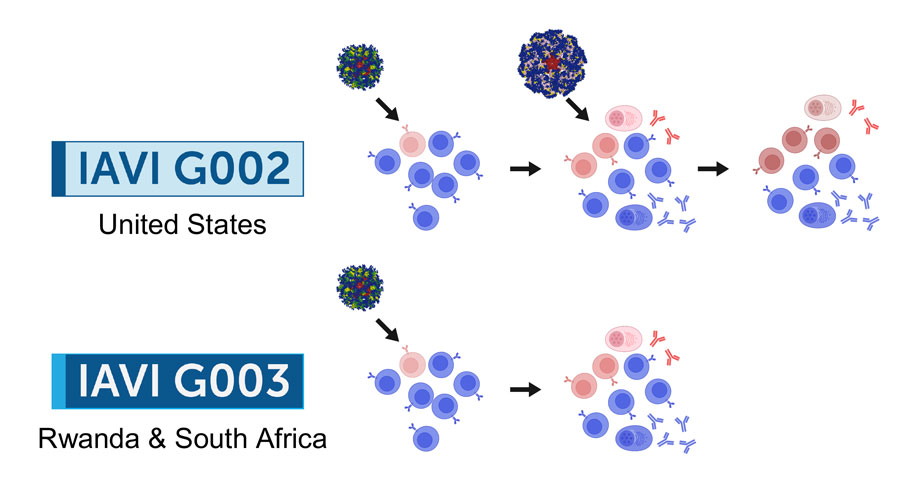
2026 marks a pivotal year for mRNA tech, with breakthroughs in cancer, HIV, microneedles, and AI-driven trials set to re...
View Board
AI transforms healthcare in 2026, detecting hidden tumors, predicting diseases before symptoms, and personalizing treatm...
View Board
AI revolutionizes medical physics, crafting precise radiation plans in minutes, transforming diagnostics, and reshaping ...
View Board
Discover Karl Landsteiner's groundbreaking work on blood groups (ABO & Rh), revolutionizing transfusions. Learn about hi...
View Board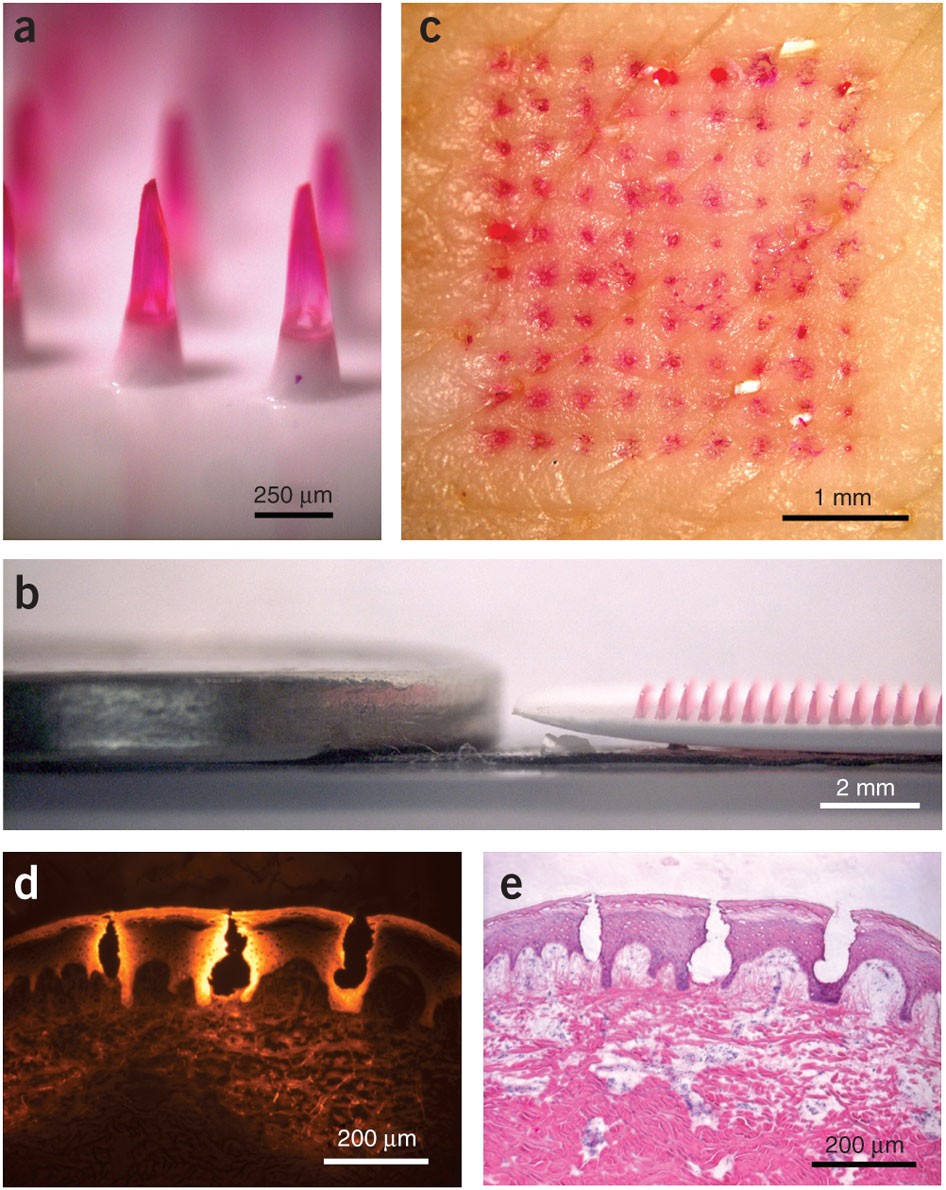
Microneedle patches deliver painless, effective vaccines via skin, revolutionizing global healthcare with self-administr...
View Board
Scientists reverse blood stem cell aging with lysosomal inhibitors and RhoA blockers, restoring regenerative capacity an...
View Board
Entdecken Sie das Leben von Robin Warren, dem medizinischen Pionier, der mit der Entdeckung von Helicobacter pylori die ...
View Board
Explore Hannah Witton's journey: from sex education pioneer to disability advocate and creator mentor. Learn about her i...
View Board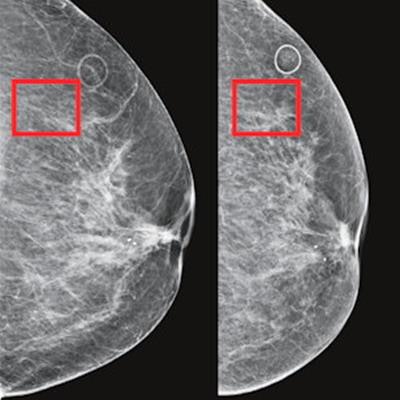
AI-powered cancer screening transforms early detection, with clinical trials showing a 28% increase in cancer detection ...
View Board
Explore Paul Broca's groundbreaking contributions to neuroanatomy and language research. Discover Broca's area, aphasia ...
View Board
Learn about Ally's Law (Restroom Access Act) and how it ensures restroom access for individuals with medical conditions ...
View Board
Discover how AI is revolutionizing the fight against antibiotic-resistant superbugs. Learn about AI-driven drug discover...
View Board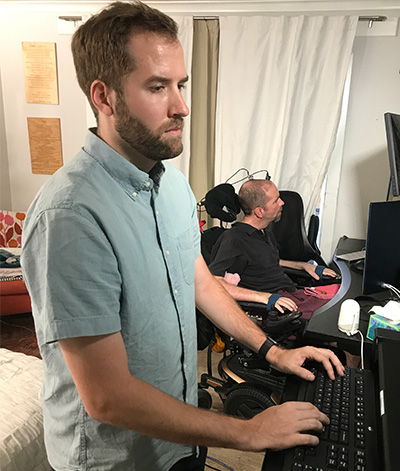
Brain-computer interface breakthroughs create thought-controlled prosthetics, restoring motor control & realistic touch....
View Board
Radiation-driven wolves in Chernobyl display rapid cancer-resistant evolution, a 30-year natural experiment revealing ge...
View Board
Dive into the fascinating world of the Merrell Twins! Discover their journey from YouTube stars to actresses and musicia...
View Board
MIT chemists synthesize verticillin A after 55 years, unlocking a potential weapon against fatal pediatric brain tumors ...
View Board
Cancer research reaches new heights as ISS microgravity enables breakthroughs like FDA-approved pembrolizumab injections...
View Board
Discover how Sir Ronald Ross revolutionized malaria understanding! Learn about his groundbreaking discovery of mosquito ...
View Board
Pancreatic cancer's sugar-coated shield uncovered: Researchers reveal how tumors exploit sialic acid to deceive immune c...
View Board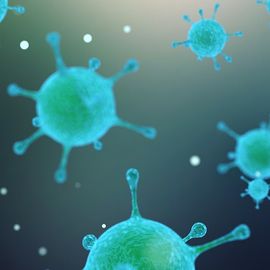
Scientists capture influenza virus invading a human cell in real-time using groundbreaking ViViD-AFM microscopy, reveali...
View Board
Comments