Explore Any Narratives
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
In the annals of medical history, few discoveries have had as profound an impact as Alexander Fleming's discovery of penicillin in 1928. This Scottish physician and microbiologist inadvertently sparked the antibiotic revolution, forever changing the landscape of modern medicine. His groundbreaking work not only introduced the world's first broadly effective antibiotic but also laid the foundation for the development of countless life-saving drugs. This article delves into the life, discoveries, and enduring legacy of Alexander Fleming, the man who transformed our ability to combat infectious diseases.
Born on August 6, 1881, in Lochfield, Scotland, Alexander Fleming grew up in a rural setting that would later influence his scientific curiosity. After completing his education at St. Mary's Hospital Medical School in London, Fleming embarked on a career in microbiology, driven by a desire to understand and combat bacterial infections.
Fleming's academic journey began at the University of London, where he studied medicine. His early exposure to the works of Louis Pasteur and Robert Koch ignited his passion for bacteriology. These pioneers in microbiology inspired Fleming to explore the intricate world of bacteria and their role in human health.
During World War I, Fleming served as a captain in the Royal Army Medical Corps. His experiences on the battlefield, where he witnessed the devastating effects of bacterial infections on wounded soldiers, deepened his resolve to find effective treatments. Post-war, he returned to St. Mary's Hospital, where he continued his research on antibacterial substances.
Before his monumental discovery of penicillin, Fleming made another significant contribution to microbiology with the identification of lysozyme in 1922. This enzyme, found in tears, saliva, and mucus, exhibited weak antibacterial properties against certain non-pathogenic bacteria.
Although lysozyme's antibacterial effects were limited, its discovery was crucial for several reasons:
Fleming's meticulous observations during his experiments with lysozyme highlighted his keen eye for detail. He noted that the enzyme could dissolve certain bacteria, albeit not the more harmful pathogens. This work underscored the potential for discovering more potent antibacterial agents, a pursuit that would soon lead him to penicillin.
The story of penicillin's discovery is one of scientific serendipity. In 1928, while studying Staphylococcus aureus at St. Mary's Hospital, Fleming noticed something unusual in one of his Petri dishes. A mold, later identified as Penicillium notatum, had contaminated the dish and inhibited the growth of bacteria around it.
Fleming's laboratory was known for its somewhat disorganized state, a characteristic that ironically played a role in his discovery. An uncovered Petri dish near an open window became contaminated with mold spores. Instead of discarding the dish, Fleming observed that the bacteria near the mold were being destroyed. This observation led him to isolate the antibacterial substance, which he named penicillin on March 7, 1929.
Despite the promising nature of his discovery, Fleming's initial publication in 1929 garnered little attention. The scientific community was skeptical, and the instability of penicillin posed significant challenges for its practical application. It would take over a decade for the full potential of penicillin to be realized, thanks to the efforts of Howard Florey and Ernst Chain.
While Alexander Fleming is credited with the discovery of penicillin, the development of the antibiotic into a viable medical treatment involved the collaborative efforts of several key figures. Among them, Howard Florey and Ernst Chain played pivotal roles in purifying penicillin and demonstrating its efficacy.
Howard Florey, an Australian pharmacologist, led the team at the University of Oxford that successfully purified penicillin. His relentless efforts in the late 1930s and early 1940s transformed Fleming's "mold juice" into a stable, usable antibiotic. Florey's work was instrumental in scaling up production and conducting the first clinical trials.
Ernst Chain, a German-born biochemist, collaborated closely with Florey. His expertise in biochemistry was crucial in isolating and concentrating penicillin. Chain's contributions ensured that the antibiotic could be produced in quantities sufficient for medical use, paving the way for its widespread adoption.
In 1945, Alexander Fleming, Howard Florey, and Ernst Chain were jointly awarded the Nobel Prize in Physiology or Medicine for their groundbreaking work on penicillin. This recognition underscored the collaborative nature of scientific discovery and the profound impact of their contributions to medicine.
The advent of World War II provided a critical impetus for the mass production of penicillin. The urgent need for effective treatments for infected wounds and diseases among soldiers accelerated the development and distribution of the antibiotic.
The first human trial of penicillin took place in 1941, with a policeman named Albert Alexander. Although the initial results were promising, supply shortages limited the treatment's effectiveness. However, subsequent trials demonstrated penicillin's remarkable ability to combat a range of bacterial infections, including streptococcal, staphylococcal, and gonococcal infections.
By 1942, the United States had established pilot plants for the mass production of penicillin. Companies like Merck played a crucial role in scaling up production, ensuring that the antibiotic was available in sufficient quantities for military use. Penicillin became a vital tool in treating wounded soldiers, significantly reducing mortality rates from infections.
The success of penicillin during the war set the stage for its post-war adoption in public health. The antibiotic's effectiveness against diseases such as syphilis, pneumonia, and meningitis revolutionized medical practice. Penicillin's impact extended beyond the battlefield, transforming the treatment of bacterial infections worldwide.
The discovery of penicillin marked the beginning of the antibiotic era, a period characterized by the development and use of antibiotics to combat bacterial infections. Fleming's work laid the foundation for modern antibiotic therapy, saving countless lives and shaping the course of medical history.
Penicillin's success inspired the discovery and development of numerous other antibiotics. Drugs like streptomycin, tetracycline, and erythromycin followed, each contributing to the arsenal of treatments available to combat bacterial infections. The antibiotic era has been marked by continuous innovation, driven by the principles established by Fleming's discovery.
Despite the transformative impact of antibiotics, their use has not been without challenges. Alexander Fleming himself warned of the potential for antibiotic resistance as early as 1942. His concerns have proven prescient, as the rise of multidrug-resistant bacteria poses a significant threat to global health. The ongoing battle against antibiotic resistance underscores the need for continued research and innovation in the field of microbiology.
Today, Alexander Fleming is remembered as a pioneer in the field of microbiology. His discovery of penicillin has earned him a place among the most influential figures in medical history. Institutions and organizations worldwide continue to honor his legacy, recognizing the profound impact of his work on human health and well-being.
In the next part of this article, we will delve deeper into the scientific details of penicillin's discovery, its mechanism of action, and the ongoing efforts to combat antibiotic resistance. Stay tuned for an exploration of the intricate world of antibiotics and the enduring legacy of Alexander Fleming.
The discovery of penicillin by Alexander Fleming was a pivotal moment in medical history, but understanding its mechanism of action and the subsequent development process is equally fascinating. This section explores the scientific intricacies of penicillin, from its antibacterial properties to the challenges faced in its mass production.
Penicillin operates as a bactericidal agent, meaning it kills bacteria rather than merely inhibiting their growth. Its primary mechanism involves interfering with the synthesis of the bacterial cell wall. Specifically, penicillin targets the enzyme transpeptidase, which is crucial for cross-linking the peptide chains in the bacterial cell wall.
When penicillin binds to transpeptidase, it prevents the formation of a strong and rigid cell wall. This weakening leads to the bacteria becoming susceptible to osmotic pressure, ultimately causing the cell to lyse (burst) and die. This mode of action is particularly effective against Gram-positive bacteria, which have a thick cell wall composed primarily of peptidoglycan.
Despite its promising antibacterial properties, the early production of penicillin faced numerous challenges. Fleming's initial "mold juice" was highly unstable and difficult to purify. The key obstacles included:
These challenges necessitated innovative solutions, which were ultimately provided by Howard Florey and Ernst Chain at the University of Oxford.
The journey of penicillin from a laboratory curiosity to a widely available antibiotic is a testament to the power of scientific collaboration and innovation. This section delves into the critical steps that transformed penicillin into a medical marvel.
In the late 1930s, Howard Florey and Ernst Chain took up the challenge of purifying and stabilizing penicillin. Their work at the University of Oxford marked a turning point in the antibiotic's development. By 1940, they had successfully produced a purified form of penicillin that was stable enough for clinical trials.
The Oxford team's breakthrough involved several key innovations:
The first human trial of penicillin took place on February 12, 1941, with a patient named Albert Alexander. Alexander, a policeman, was suffering from severe infections caused by Staphylococcus aureus. The trial demonstrated penicillin's remarkable efficacy, as Alexander showed significant improvement shortly after receiving the treatment.
However, the initial success was tempered by the limited supply of penicillin. Despite the Oxford team's efforts, they could not produce enough penicillin to sustain Alexander's treatment, and he ultimately relapsed. This experience underscored the urgent need for large-scale production of the antibiotic.
The onset of World War II provided the necessary impetus for the mass production of penicillin. The United States, recognizing the antibiotic's potential to save lives on the battlefield, invested heavily in scaling up production. Key developments during this period included:
By 1944, penicillin was being produced in large quantities, with hundreds of liters available weekly. This mass production effort was instrumental in treating wounded soldiers and reducing mortality rates from bacterial infections.
The introduction of penicillin revolutionized the field of medicine, transforming the treatment of bacterial infections and saving countless lives. This section explores the profound impact of penicillin on modern medical practice and public health.
Before the advent of penicillin, bacterial infections were a leading cause of death worldwide. Diseases such as pneumonia, syphilis, and meningitis often proved fatal due to the lack of effective treatments. Penicillin changed this landscape dramatically, providing a powerful tool to combat a wide range of bacterial infections.
Some of the key infections treated by penicillin include:
The impact of penicillin extended beyond the treatment of systemic infections. The antibiotic played a crucial role in surgical practice and wound care, significantly reducing the risk of post-operative infections. Before penicillin, surgical procedures carried a high risk of complications due to bacterial contamination. With the advent of penicillin, surgeons could perform operations with greater confidence, knowing that infections could be effectively managed.
During World War II, penicillin was extensively used to treat wounded soldiers, preventing infections that would have otherwise been fatal. This application not only saved lives but also demonstrated the antibiotic's versatility and efficacy in a range of medical settings.
The success of penicillin inspired a wave of research into other antibiotics. Scientists around the world began exploring the potential of natural and synthetic compounds to combat bacterial infections. This research led to the discovery of numerous antibiotics, each with unique properties and applications.
Some of the notable antibiotics developed in the wake of penicillin include:
The discovery of these antibiotics expanded the arsenal of treatments available to medical professionals, further enhancing their ability to combat bacterial infections.
Despite the transformative impact of penicillin, Alexander Fleming was acutely aware of the potential for antibiotic resistance. As early as 1942, he warned that the overuse and misuse of antibiotics could lead to the development of resistant bacterial strains. This section explores Fleming's prescient warnings and the ongoing challenge of antibiotic resistance.
In his Nobel Prize acceptance speech, Fleming cautioned about the dangers of antibiotic resistance:
"It is not difficult to make microbes resistant to penicillin in the laboratory by exposing them to concentrations not sufficient to kill them, and the same thing has occasionally happened in the body."
Fleming's observations were based on his experiments, where he noted that bacteria exposed to sub-lethal doses of penicillin could develop resistance. This phenomenon, known as antibiotic resistance, occurs when bacteria evolve mechanisms to survive the effects of antibiotics.
The first cases of penicillin-resistant bacteria were documented in the early 1940s, shortly after the antibiotic's introduction. One of the most notable examples is Staphylococcus aureus, a common pathogen that quickly developed resistance to penicillin. Today, methicillin-resistant Staphylococcus aureus (MRSA) is a significant public health concern, causing infections that are difficult to treat with standard antibiotics.
The rise of antibiotic resistance is driven by several factors, including:
Today, antibiotic resistance is recognized as a global health crisis. The World Health Organization (WHO) has warned that without urgent action, we could enter a post-antibiotic era where common infections become untreatable. The implications of this crisis are profound, affecting medical procedures, public health, and global economies.
Key statistics highlighting the severity of the issue include:
Addressing this crisis requires a multifaceted approach, including the development of new antibiotics, improved stewardship of existing antibiotics, and global cooperation to combat the spread of resistant bacteria.
The legacy of Alexander Fleming extends far beyond his discovery of penicillin. His work laid the foundation for modern antibiotic therapy and inspired generations of scientists to explore the potential of antimicrobial agents. This section reflects on Fleming's enduring impact and the future of antibiotic research.
Fleming's contributions to microbiology are vast and varied. In addition to his discovery of penicillin, he made significant advancements in the understanding of bacterial infections and the body's immune response. His work on lysozyme provided insights into the body's natural defense mechanisms, while his research on antibacterial agents paved the way for the development of numerous life-saving drugs.
Fleming's approach to scientific inquiry, characterized by curiosity and keen observation, serves as a model for researchers today. His ability to recognize the potential in seemingly mundane observations, such as a contaminated Petri dish, highlights the importance of curiosity-driven research.
The ongoing challenge of antibiotic resistance underscores the need for continued innovation in the field of antimicrobial research. Scientists are exploring several avenues to address this crisis, including:
The future of antibiotic research holds promise, with advancements in technology and a deeper understanding of bacterial biology driving innovation. However, the lessons of the past, embodied in Fleming's warnings about resistance, must guide these efforts to ensure the continued effectiveness of antibiotics.
In the final part of this article, we will explore the broader implications of Fleming's discovery, its impact on society, and the ongoing efforts to honor his legacy. Stay tuned for a comprehensive conclusion to our exploration of Alexander Fleming and the antibiotic revolution.
The discovery of penicillin by Alexander Fleming not only revolutionized medicine but also had profound societal implications. This section explores how the antibiotic era transformed public health, extended life expectancy, and reshaped medical practices worldwide.
Before the antibiotic era, infectious diseases were the leading cause of death globally. Conditions like pneumonia, tuberculosis, and sepsis claimed millions of lives annually. The introduction of penicillin dramatically altered this landscape:
These changes had far-reaching economic and social consequences, allowing populations to grow healthier and more productive.
The availability of effective antibiotics transformed medical practices in numerous ways:
The antibiotic era fundamentally changed how doctors approached patient care, shifting from reactive treatment of infections to preventive measures and more aggressive medical interventions.
Beyond his scientific discoveries, Alexander Fleming's approach to research and his personal philosophy continue to inspire scientists and medical professionals today. This section examines his lasting influence on the scientific community and medical education.
Fleming's discovery of penicillin exemplifies several key principles that remain fundamental to scientific research:
These principles continue to guide scientific inquiry and innovation in the 21st century.
Fleming's story has become a cornerstone in medical education, inspiring countless students to pursue careers in microbiology and pharmaceutical research. His life and work demonstrate:
Many modern researchers cite Fleming as a key influence in their decision to study infectious diseases and antibiotic development.
The global recognition of Alexander Fleming's contributions has led to numerous commemorations and institutions dedicated to preserving his legacy. This section explores how his work continues to be honored worldwide.
Several institutions around the world celebrate Fleming's achievements:
These museums serve as educational resources, helping the public understand the significance of antibiotic discovery and the ongoing challenges in infectious disease treatment.
Fleming's name has become synonymous with scientific excellence in microbiology:
These honors ensure that Fleming's legacy continues to inspire new generations of scientists and medical professionals.
The story of penicillin offers valuable lessons for addressing contemporary challenges in medicine and public health. This section examines how Fleming's experiences can inform our approach to current and future health crises.
Fleming's early warnings about antibiotic resistance provide crucial insights for combating this modern crisis:
These principles are particularly relevant as we face the growing threat of antimicrobial resistance, which the WHO has identified as one of the top 10 global public health threats.
The penicillin story demonstrates the potential for innovative solutions to emerge from unexpected sources. Modern approaches to antimicrobial development include:
These innovative approaches, inspired by the spirit of Fleming's discovery, offer hope in the fight against antibiotic-resistant infections.
The discovery of penicillin by Alexander Fleming in 1928 stands as one of the most significant milestones in medical history. This accidental yet revolutionary finding transformed the treatment of bacterial infections, saved countless lives, and laid the foundation for modern antibiotic therapy. As we reflect on Fleming's contributions, several key takeaways emerge:
As we face the challenges of antibiotic resistance and emerging infectious diseases, the story of Alexander Fleming and penicillin serves as both a source of inspiration and a cautionary tale. It reminds us of the transformative power of scientific discovery while underscoring the importance of responsible innovation and global cooperation in addressing health crises. The antibiotic revolution sparked by Fleming's discovery continues to shape modern medicine, and his legacy endures as a testament to the profound impact that a single scientific breakthrough can have on humanity.
In an era where the threat of antibiotic-resistant bacteria looms large, the lessons from Fleming's discovery are more relevant than ever. By embracing the spirit of curiosity, collaboration, and responsible innovation that characterized his work, we can honor his legacy while forging new paths in the ongoing battle against infectious diseases. The story of Alexander Fleming and penicillin is not just a chapter in medical history—it is a continuing narrative that challenges and inspires us to push the boundaries of scientific discovery for the betterment of global health.
Your personal space to curate, organize, and share knowledge with the world.
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
Connect with others who share your interests. Create and participate in themed boards about any topic you have in mind.
Contribute your knowledge and insights. Create engaging content and participate in meaningful discussions across multiple languages.
Already have an account? Sign in here

Discover the fascinating legacy of Félix d'Herelle, the self-taught pioneer behind bacteriophage therapy. This captivati...
View Board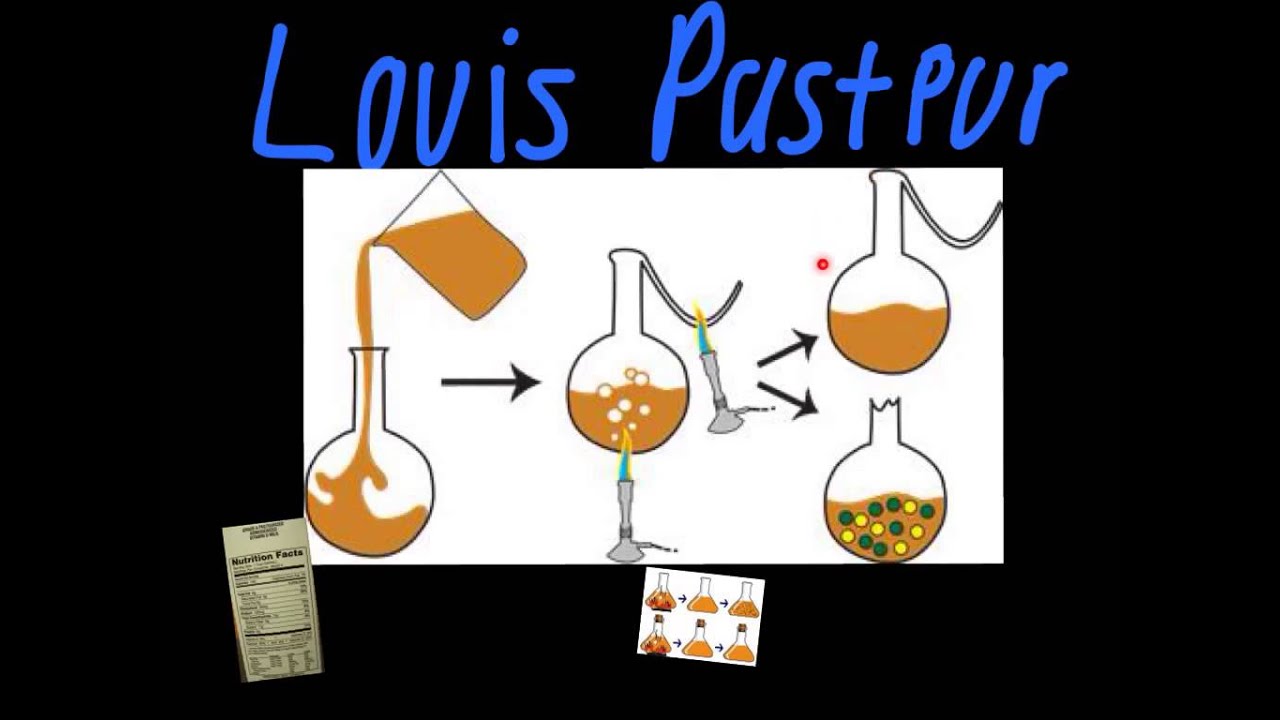
Louis Pasteur, the father of modern microbiology, revolutionized science with germ theory, pasteurization, and vaccines....
View Board
Discover how Louis Pasteur revolutionized medicine with germ theory, vaccines, and pasteurization. Explore his enduring ...
View Board
Discover the groundbreaking journey of Barry Marshall, a trailblazer in gastroenterology whose bold hypotheses and revol...
View Board
Discover how AI is revolutionizing the fight against antibiotic resistance by accelerating drug discovery, predicting ou...
View Board
Explore the life and legacy of Karl Landsteiner, the visionary who revolutionized medical science with the discovery of ...
View Board
Discover the groundbreaking journey of Ronald Ross, the pioneering scientist whose revolutionary understanding of malari...
View Board
"Explore microbiology's impact on health, industry, and the environment. Discover groundbreaking findings like penicilli...
View Board
"Explore Manuel García's vocal science legacy & laryngoscope invention. Discover how his innovations shaped modern voice...
View Board
"Manuel Elkin Patarroyo, a pioneering immunologist, developed a malaria vaccine and advocates for global health, inspiri...
View Board
Discover Félix d'Hérelle, the self-taught genius who revolutionized science with bacteriophages. Explore his groundbreak...
View Board
Explore the inspiring journey of Gerty Cori, the first woman Nobel laureate in Physiology or Medicine, who defied societ...
View Board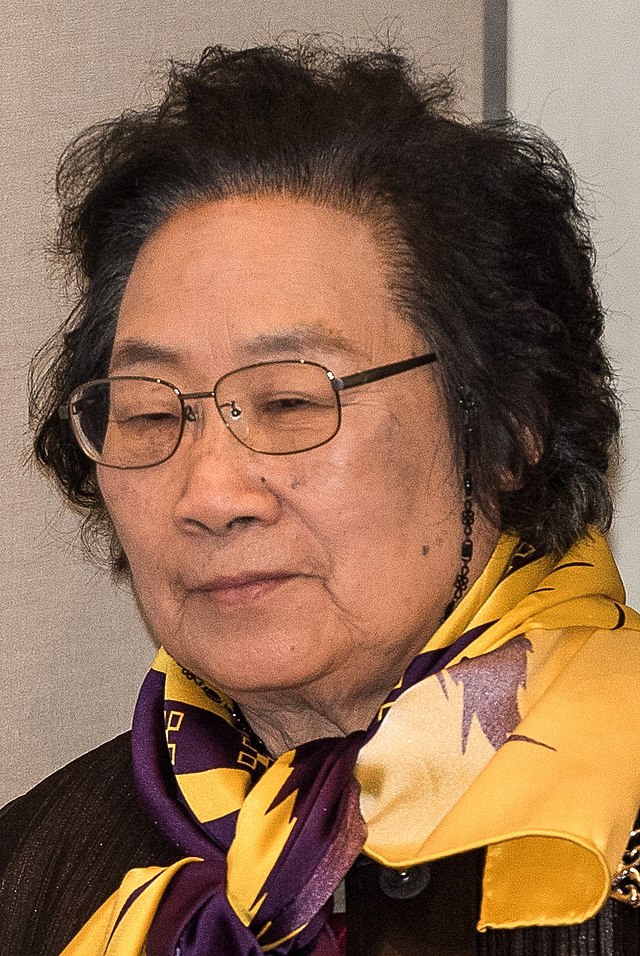
Discover the compelling journey of Tu Youyou, the legendary scientist who revolutionized malaria treatment by integratin...
View Board
"Discover Gabriele Falloppio, the 16th-century anatomist who transformed reproductive medicine. Learn about his life, di...
View Board
Discover how Jonas Salk's polio vaccine eradicated fear and transformed global health. Learn about its impact, challenge...
View Board
**Meta Description:** Discover how Francisco Mojica, the Spanish microbiologist behind CRISPR’s groundbreaking discove...
View Board
Discover how Frederick Banting's groundbreaking insulin discovery revolutionized diabetes treatment, saving millions. Ex...
View Board
"Discover Luigi Galvani's frog leg experiments that sparked modern neurophysiology. Learn how his work shaped neuroscien...
View Board
Fritz Haber: A Chemist Whose Work Changed the World The Rise of a Scientist Fritz Haber was born on December 9, 1868, i...
View Board
Узнайте, как революционный микроскоп ViViD-AFM раскрывает тайны проникновения вируса гриппа в клетки в реальном времени....
View Board
Comments