Explore Any Narratives
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
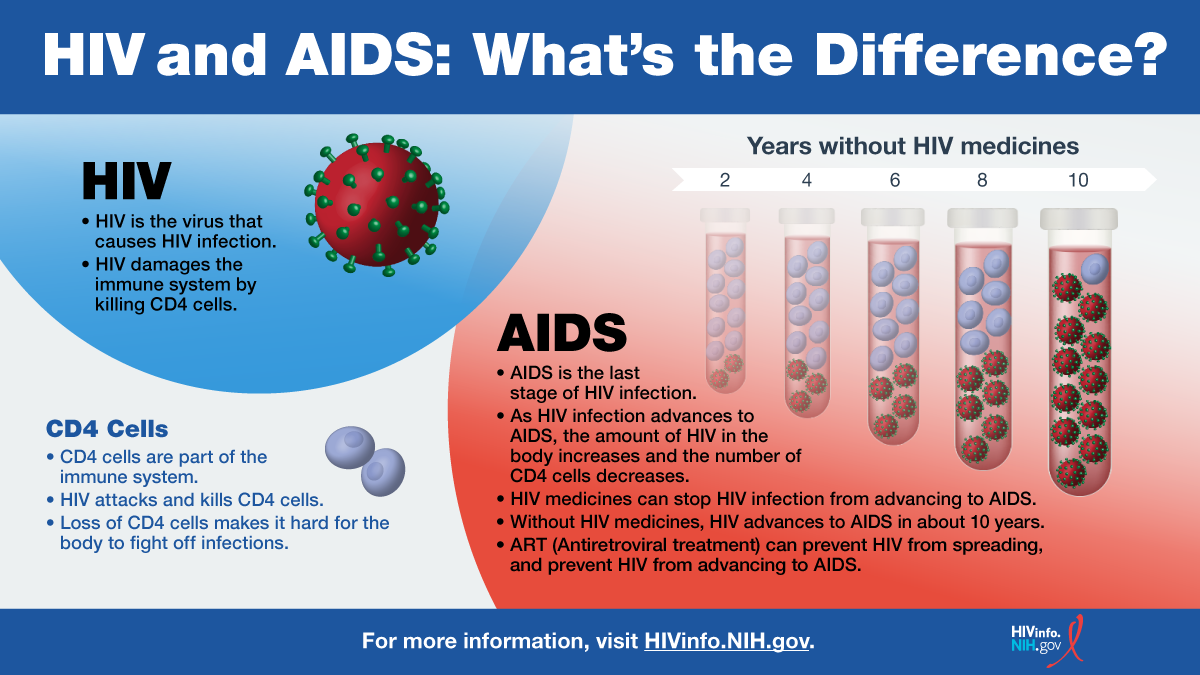
HIV (Human Immunodeficiency Virus) is a global health challenge that has affected millions of lives since its discovery in the 1980s. This virus attacks the immune system, specifically the CD4 cells (T cells), which are crucial for fighting infections. If left untreated, HIV can lead to AIDS (Acquired Immunodeficiency Syndrome), the final stage of HIV infection where the immune system is severely damaged.
Thanks to advancements in medical science, particularly the development of antiretroviral therapy (ART), people living with HIV can now manage the virus effectively and live long, healthy lives. However, the global impact of HIV remains significant, with millions of new infections and deaths reported annually.
As of 2024, the global prevalence of HIV stands at 40.8 million people living with the virus. This includes 2.42 million children aged 0-19 and 1.4 million children aged 0-14. These statistics highlight the widespread nature of the virus and its impact on diverse populations, including vulnerable groups such as children and adolescents.
The distribution of HIV is not uniform across the globe. Certain regions, particularly sub-Saharan Africa, bear a disproportionate burden of the epidemic. This region accounts for a significant portion of new infections and deaths, underscoring the need for targeted interventions and resources.
In 2024, there were 1.3 million new HIV infections globally, averaging about 3,500 new infections per day. While this represents a 61% decrease from the peak in 1996 (3.4 million) and a 40% decrease from 2010 (2.2 million), it falls short of the 2025 target of fewer than 370,000 new infections.
The decline in new infections is a testament to the effectiveness of prevention strategies, including condom use, testing, and pre-exposure prophylaxis (PrEP). However, the stagnation in recent years indicates that sustained efforts and innovative approaches are necessary to achieve global targets.
Certain populations are at higher risk of HIV infection. These include men who have sex with men (MSM), people who inject drugs, sex workers, and transgender women. In 2024, these key populations and their partners accounted for more than 50% of new global infections.
In the United States, MSM accounted for 67% of new HIV infections and 87% of infections among males. This highlights the importance of tailored prevention and treatment programs for these high-risk groups.
Despite significant progress in treatment and prevention, AIDS-related deaths remain a critical concern. In 2024, there were 630,000 AIDS-related deaths globally, including approximately 250 children per day. These statistics underscore the urgent need for expanded access to antiretroviral therapy (ART) and comprehensive care.
The majority of AIDS-related deaths occur in sub-Saharan Africa, which accounts for 61% of global deaths. This region faces unique challenges, including limited healthcare infrastructure, stigma, and socioeconomic barriers that hinder access to treatment and prevention services.
Access to antiretroviral therapy (ART) has transformed the landscape of HIV treatment. As of 2024, 31.6 million people globally are on ART, representing about 77% of those living with HIV. This widespread access to treatment has significantly improved the quality of life for people living with HIV and reduced the risk of transmission.
However, disparities in treatment access persist. While some regions, such as Eastern and Southern Africa, have made substantial progress with 84% of people living with HIV on ART, other regions, like Latin America, face challenges in scaling up treatment and prevention efforts. For instance, PrEP access in Latin America is currently at 250,000, far below the target of 2 million.
The global community has set ambitious targets to end the HIV epidemic by 2030. The 95-95-95 targets aim to ensure that by 2025, 95% of people living with HIV are diagnosed, 95% of those diagnosed are on treatment, and 95% of those on treatment achieve viral suppression.
While progress has been made, achieving these targets remains uneven. Disparities in healthcare access, funding gaps, and socioeconomic factors continue to pose significant challenges. Addressing these inequalities is crucial for making sustained progress toward ending the HIV epidemic.
The HIV epidemic has evolved significantly since its discovery in the 1980s. The peak of new infections occurred in 1996, with 3.4 million new cases. Since then, global efforts in prevention, testing, and treatment have led to a substantial reduction in new infections and deaths.
Key milestones in the fight against HIV include the development of antiretroviral therapy (ART) in the mid-1990s, which revolutionized HIV treatment, and the introduction of pre-exposure prophylaxis (PrEP) in the 2010s, which provided a highly effective prevention tool for individuals at high risk of infection.
The impact of HIV varies significantly by region. Sub-Saharan Africa remains the most affected, with 21.1 million people living with HIV and 490,000 new infections in 2024. This region also bears 52% of the global HIV burden.
In contrast, regions like Latin America have seen a 13% increase in new infections since 2010. This rise highlights the need for renewed efforts in prevention, testing, and treatment access in these areas.
Despite the progress made in the fight against HIV, significant challenges remain. Funding gaps, healthcare disparities, and socioeconomic barriers continue to hinder efforts to end the epidemic. Additionally, emerging issues such as climate change, conflict, and displacement pose new threats to HIV prevention and treatment programs.
Looking ahead, the global community must prioritize equitable access to healthcare, innovative prevention strategies, and sustained funding to achieve the 2030 targets. By addressing these challenges, we can make significant strides toward ending the HIV epidemic and improving the lives of millions affected by the virus.
Understanding how HIV is transmitted is crucial for effective prevention. The virus spreads primarily through unprotected sexual contact, sharing needles, and mother-to-child transmission during pregnancy, childbirth, or breastfeeding. Less commonly, HIV can be transmitted through blood transfusions or occupational exposure in healthcare settings.
Prevention strategies have evolved significantly over the years. Key approaches include:
HIV testing is a cornerstone of prevention efforts. Early diagnosis allows individuals to start treatment promptly, improving health outcomes and reducing transmission risk. The U.S. Centers for Disease Control and Prevention (CDC) recommends that everyone aged 13-64 get tested at least once, with more frequent testing for those at higher risk.
Innovations in testing, such as rapid tests and self-testing kits, have made it easier for people to know their status. These advancements are particularly important in reaching underserved populations and reducing stigma associated with testing.
The impact of HIV varies across different populations, with certain groups facing higher risks due to biological, behavioral, and socioeconomic factors. Understanding these disparities is essential for developing targeted interventions.
In 2024, women and girls accounted for 45% of new global HIV infections. In sub-Saharan Africa, adolescent girls and young women (aged 15-24) are particularly vulnerable, with over 210,000 new infections in this group alone. This translates to approximately 570 new infections per day.
Factors contributing to this disparity include gender inequality, limited access to education, and biological susceptibility to HIV infection. Programs aimed at empowering women and girls, such as cash transfer initiatives and school-based HIV education, have shown promise in reducing infection rates.
Men who have sex with men (MSM) are disproportionately affected by HIV. In the United States, MSM accounted for 67% of new HIV infections in 2022, with this figure rising to 87% among males. Globally, MSM are 28 times more likely to acquire HIV compared to the general population.
Stigma, discrimination, and criminalization of same-sex relationships in many countries exacerbate the risk for MSM. Comprehensive prevention strategies, including PrEP, regular testing, and community-based support, are critical for addressing this disparity.
People who inject drugs (PWID) face a heightened risk of HIV due to needle-sharing practices. In some regions, HIV prevalence among PWID can exceed 20%. Harm reduction strategies, such as needle exchange programs and opioid substitution therapy, have proven effective in reducing HIV transmission in this population.
Despite their effectiveness, these programs often face legal and societal barriers, limiting their implementation. Advocacy for evidence-based policies and increased funding is essential to expand access to these life-saving interventions.
Children represent a vulnerable population in the HIV epidemic. In 2024, there were 2.42 million children aged 0-19 and 1.4 million children aged 0-14 living with HIV globally. Without intervention, the risk of mother-to-child transmission can be as high as 45%, but with proper treatment, this risk can be reduced to less than 1%.
Preventing mother-to-child transmission (PMTCT) is a critical component of HIV prevention efforts. The World Health Organization (WHO) recommends a comprehensive approach that includes:
In 2024, 85% of pregnant women living with HIV received ART, a significant improvement from previous years. However, gaps remain, particularly in regions with limited healthcare access.
Children living with HIV face unique challenges in accessing treatment. Pediatric ART formulations are often less available than adult formulations, and diagnostic tools for infants can be limited in resource-poor settings. Additionally, adherence to treatment can be difficult for children, requiring strong support from caregivers and healthcare providers.
Efforts to improve pediatric HIV care include the development of child-friendly formulations, point-of-care diagnostic tools, and community-based support programs. These initiatives aim to ensure that children living with HIV can access the care they need to thrive.
The global response to HIV has been shaped by international organizations, governments, and community-based initiatives. Key players include UNAIDS, the World Health Organization (WHO), and The Global Fund to Fight AIDS, Tuberculosis and Malaria. These organizations work to coordinate efforts, set global targets, and mobilize resources.
UNAIDS plays a pivotal role in the global HIV response by setting strategic goals and monitoring progress. The organization's 95-95-95 targets have guided national and international efforts to scale up testing, treatment, and viral suppression. UNAIDS also advocates for human rights-based approaches and addresses structural barriers that hinder HIV prevention and treatment.
In its 2025 Global AIDS Update, UNAIDS highlighted the urgent need for increased funding and political commitment to sustain progress. The report warned of potential reversals in gains due to funding shortfalls and global crises such as conflict and climate change.
The Global Fund has been instrumental in financing HIV programs worldwide. Since its inception, the fund has invested over $50 billion in HIV prevention, treatment, and care. These investments have contributed to significant reductions in new infections and deaths, particularly in high-burden regions.
Despite its successes, The Global Fund faces ongoing challenges, including donor fatigue and competing global health priorities. Sustained funding is essential to maintain progress and address emerging threats, such as drug resistance and health system weaknesses.
Funding remains a critical challenge in the global HIV response. In 2024, UNAIDS estimated a $8.1 billion funding gap for HIV programs in low- and middle-income countries. This shortfall threatens to reverse progress, particularly in areas such as pediatric HIV care and prevention programs for key populations.
Efficient resource allocation is equally important. Ensuring that funds reach the most affected communities and are used effectively requires strong governance, transparency, and community engagement. Innovative financing mechanisms, such as social impact bonds and public-private partnerships, are being explored to bridge the funding gap.
Research and innovation continue to drive progress in HIV prevention, treatment, and care. Recent advancements offer hope for more effective interventions and, ultimately, a cure.
One of the most promising developments is the introduction of long-acting antiretrovirals. These formulations, such as cabotegravir and rilpivirine, are administered as injections every one to two months, reducing the burden of daily pill-taking. Long-acting PrEP has shown high efficacy in clinical trials and is now being rolled out in several countries.
Long-acting treatments have the potential to improve adherence and retention in care, particularly for populations facing barriers to daily medication. However, challenges such as cost and distribution logistics must be addressed to ensure widespread access.
The search for an HIV vaccine and a cure remains a top priority for researchers. While significant challenges exist due to the virus's ability to mutate and evade the immune system, several promising approaches are under investigation:
While a cure remains elusive, recent cases of long-term remission, such as the "Berlin Patient" and "London Patient", provide proof of concept that a cure is possible. These cases involved stem cell transplants from donors with a rare genetic mutation that confers HIV resistance.
Digital health technologies are transforming HIV care by improving access to services and enhancing patient engagement. Innovations include:
These technologies have the potential to overcome barriers to care, such as stigma, distance, and healthcare workforce shortages. However, ensuring digital literacy and data privacy are critical for their successful implementation.
Stigma and discrimination remain significant barriers in the fight against HIV. Fear of judgment and social exclusion often prevent individuals from seeking testing, treatment, and support services. Addressing these issues is crucial for achieving global HIV targets and improving the quality of life for people living with HIV.
Stigma can manifest in various forms, including social rejection, employment discrimination, and healthcare disparities. Studies show that individuals who experience HIV-related stigma are less likely to adhere to antiretroviral therapy (ART) and more likely to suffer from mental health issues such as depression and anxiety.
In many communities, misconceptions about HIV transmission persist, fueling fear and discrimination. For example, some people still believe that HIV can be spread through casual contact, such as hugging or sharing food. Education and awareness campaigns are essential to dispel these myths and promote evidence-based understanding of HIV.
Efforts to reduce HIV-related stigma include:
Organizations such as UNAIDS and the International AIDS Society have developed guidelines and toolkits to help communities and governments address stigma effectively. These resources emphasize the importance of human rights and inclusivity in HIV responses.
Community-based organizations (CBOs) play a vital role in the global HIV response. These organizations are often led by or closely connected to the communities they serve, allowing them to provide culturally appropriate and tailored services that meet the unique needs of their populations.
CBOs offer a wide range of services, including:
These organizations are particularly effective in reaching marginalized populations, such as sex workers, people who inject drugs, and LGBTQ+ individuals, who may face barriers in accessing traditional healthcare services.
Numerous CBOs have demonstrated remarkable success in HIV prevention and care. For example, the Treatment Action Campaign (TAC) in South Africa has been instrumental in advocating for access to ART and improving HIV policies. Similarly, the GMHC (Gay Men's Health Crisis) in the United States has provided comprehensive support services to thousands of individuals affected by HIV.
Research has shown that communities with strong CBO involvement experience higher rates of HIV testing, better treatment adherence, and improved health outcomes. These organizations often serve as a bridge between healthcare systems and the communities they serve, ensuring that services are accessible, acceptable, and effective.
International policies and frameworks provide a roadmap for the global HIV response. These guidelines help countries develop national strategies, allocate resources, and monitor progress toward ending the HIV epidemic.
The United Nations Sustainable Development Goals (SDGs), adopted in 2015, include a specific target to end the HIV epidemic by 2030. SDG 3.3 aims to "end the epidemics of AIDS, tuberculosis, malaria, and neglected tropical diseases" by ensuring universal access to prevention, treatment, and care.
Progress toward this goal is measured through indicators such as the number of new HIV infections, AIDS-related deaths, and access to ART. Achieving SDG 3.3 requires a multi-sectoral approach, involving healthcare, education, social protection, and human rights initiatives.
The UNAIDS 95-95-95 targets represent a bold ambition to accelerate progress in the HIV response. By 2025, the goals are:
As of 2024, global progress toward these targets has been uneven. While some countries have achieved or exceeded the 95-95-95 benchmarks, others lag due to limited resources, health system weaknesses, and social barriers. Continued investment and innovation are needed to close these gaps.
As the global community strives to end the HIV epidemic, several emerging challenges and future directions must be considered. Addressing these issues will require collaboration, innovation, and sustained commitment from all stakeholders.
Key challenges include:
To overcome these challenges, the following strategies are essential:
The global HIV epidemic has evolved significantly since its emergence in the 1980s. While antiretroviral therapy and prevention strategies have transformed HIV from a fatal diagnosis to a manageable chronic condition, the fight is far from over. With 40.8 million people living with HIV worldwide and 1.3 million new infections in 2024 alone, sustained effort and innovation are crucial.
Key takeaways from this article include:
Ending the HIV epidemic by 2030 is an ambitious but achievable goal. It requires a collective commitment from governments, healthcare providers, researchers, communities, and individuals. By addressing structural barriers, expanding access to care, and fostering inclusivity, we can create a world where HIV no longer poses a threat to public health. Together, we can turn the tide against HIV and ensure a healthier, more equitable future for all.
"The fight against HIV is not just about medical treatments and prevention strategies; it is about dignity, human rights, and social justice. Every person deserves access to the care and support they need to live a healthy and fulfilling life."


Your personal space to curate, organize, and share knowledge with the world.
Discover and contribute to detailed historical accounts and cultural stories. Share your knowledge and engage with enthusiasts worldwide.
Connect with others who share your interests. Create and participate in themed boards about any topic you have in mind.
Contribute your knowledge and insights. Create engaging content and participate in meaningful discussions across multiple languages.
Already have an account? Sign in here

Discover how Jonas Salk's polio vaccine eradicated fear and transformed global health. Learn about its impact, challenge...
View Board
Discover how AI is revolutionizing the fight against antibiotic resistance by accelerating drug discovery, predicting ou...
View BoardDiscover the inspiring journey of Mikhail Varshavski, also known as "Doctor Mike," the internet's favorite doctor who bl...
View Board
Discover the groundbreaking journey of Ronald Ross, the pioneering scientist whose revolutionary understanding of malari...
View Board
"Manuel Elkin Patarroyo, a pioneering immunologist, developed a malaria vaccine and advocates for global health, inspiri...
View Board**Meta Description:** Discover Hippocrates, the Father of Medicine, whose ethical principles and groundbreaking theori...
View Board
Explore the life and legacy of Karl Landsteiner, the visionary who revolutionized medical science with the discovery of ...
View Board
Discover how Ally's Law ensures restroom access for those with Crohn's, IBD, and other urgent medical needs. Learn its i...
View Board
Узнайте, как революционный микроскоп ViViD-AFM раскрывает тайны проникновения вируса гриппа в клетки в реальном времени....
View Board
"Discover how Fleming's 1928 penicillin discovery revolutionized medicine, saving millions. Learn about the antibiotic e...
View Board
Explore the inspiring journey of Jonathan Tomines, widely known as "The Toe Bro," who has revolutionized podiatry with h...
View Board
Discover the transformative journey of Zubin Damania, or ZDoggMD, a trailblazing physician intertwining humor and advoca...
View Board
Louis Pasteur, the father of modern microbiology, revolutionized science with germ theory, pasteurization, and vaccines....
View Board
Discover how the Human Leukocyte Antigen (HLA) system shapes immune responses, influences disease susceptibility, and re...
View Board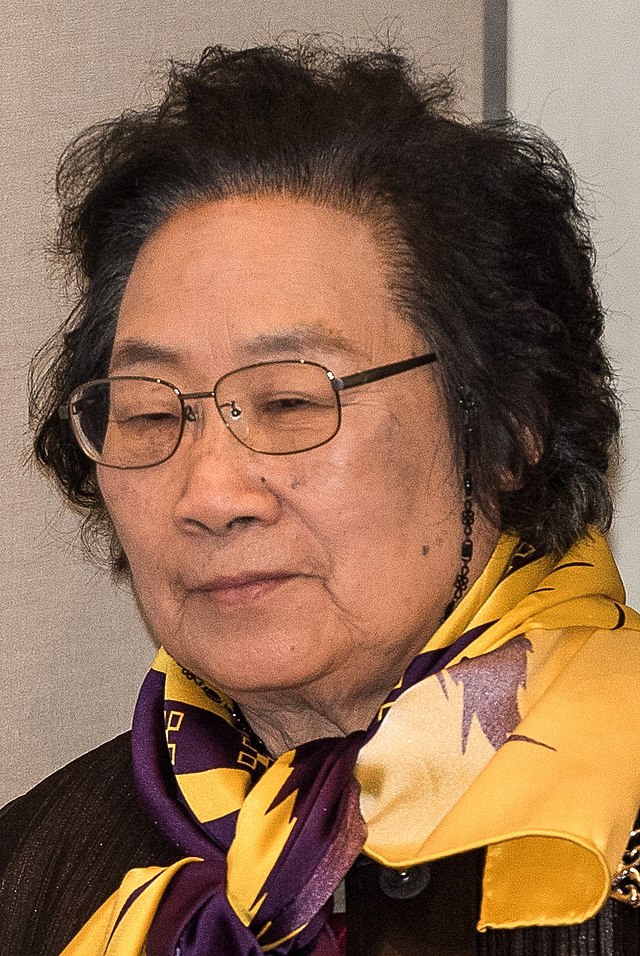
Discover the compelling journey of Tu Youyou, the legendary scientist who revolutionized malaria treatment by integratin...
View Board
Discover the fascinating legacy of Félix d'Herelle, the self-taught pioneer behind bacteriophage therapy. This captivati...
View Board
Explore the groundbreaking contributions of Jean Dausset, the luminary in immunogenetics whose discovery of the Human Le...
View Board
Discover how Louis Pasteur revolutionized medicine with germ theory, vaccines, and pasteurization. Explore his enduring ...
View Board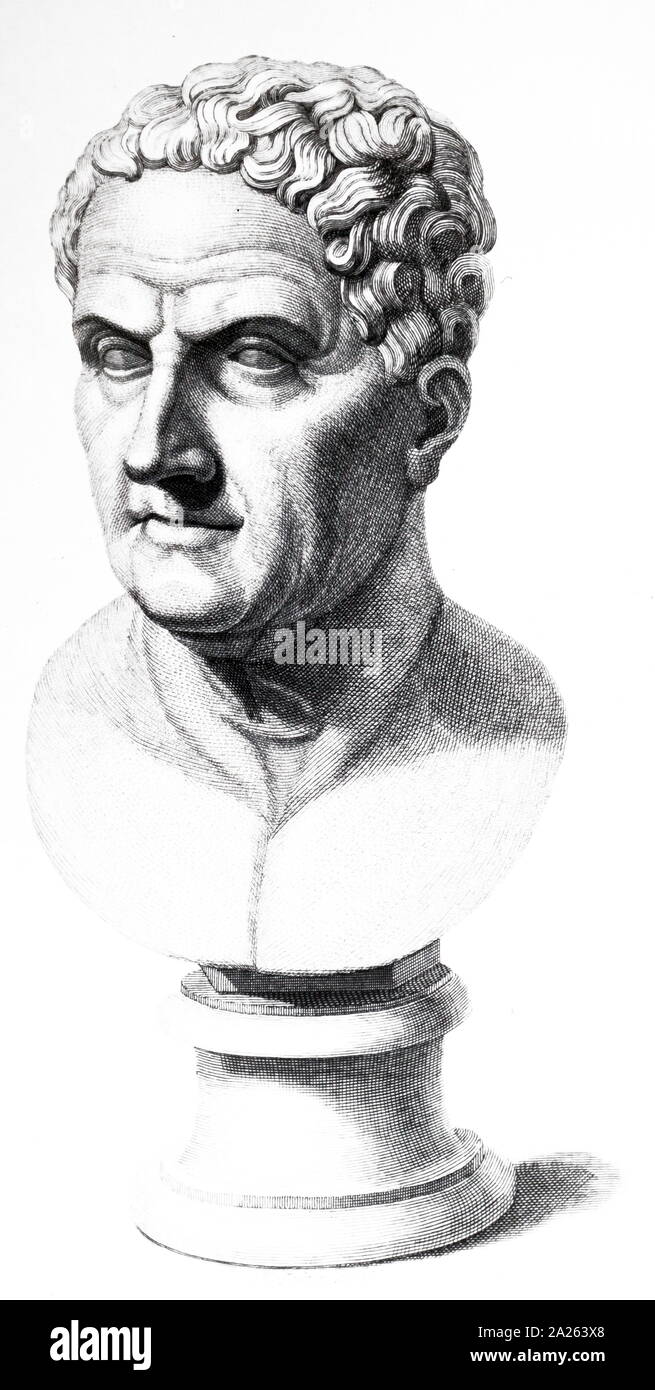
> **Meta Description:** Explore the life and legacy of Galen, the father of medicine, whose groundbreaking work in anato...
View Board
Discover Félix d'Hérelle, the self-taught genius who revolutionized science with bacteriophages. Explore his groundbreak...
View Board
Comments