MIT Breaks 55-Year Barrier: Synthesizing a Fungal Molecule for Brain Tumors
The molecule sat in the scientific literature for over half a century, a tantalizing ghost. Isolated from a fungus in 1970, verticillin A was known to be a potent killer of cancer cells. Chemists understood its promise against some of the most aggressive tumors. They also understood its profound, almost arrogant, complexity. Ten rings, eight stereocenters, and a breathtaking fragility made it a Mount Everest of synthetic chemistry: visible, desirable, and impossibly out of reach. For 55 years, no one could build it from scratch in a lab. The compound remained a scientific curiosity, its therapeutic potential locked away by its own intricate architecture.
That changed on a quiet morning in December 2025. In a lab at the Massachusetts Institute of Technology, a team led by Professor Mohammad Movassaghi had just completed a 16-step chemical gauntlet. They had created, for the first time in history, synthetic verticillin A. This was not merely an academic trophy. It was the master key to a vault. The vault contained a potential new weapon against one of medicine’s cruelest adversaries: diffuse midline glioma (DMG), a rare and fatal pediatric brain cancer.
“Nature is the ultimate chemist, but she doesn’t produce these molecules on our schedule or in the quantities we need,” says Movassaghi. “For decades, verticillin A was a blueprint without a construction method. Our synthesis is that method. It transforms a scientific artifact into a tangible starting point for medicine.”
This breakthrough, formally announced on December 3, 2025, in the Journal of the American Chemical Society, represents a seismic shift in a niche but critical field. It blends the old and the new: a forgotten natural product resurrected by cutting-edge synthetic technique, now aimed at a cancer whose biology was only recently decoded. The story is not just about making a difficult molecule. It’s about dismantling a fundamental bottleneck in drug discovery. When a promising compound cannot be synthesized, it can never be optimized, never be mass-produced, never be tested in a robust clinical pipeline. It remains a footnote. MIT’s work erases the footnote and starts a new chapter.
The Impossible Molecule and the Unforgiving Cancer
To grasp the significance of the synthesis, you must first appreciate the sheer brutality of the disease it targets. Diffuse midline glioma strikes children, often between the ages of 5 and 10. The tumor weaves itself into the delicate, critical structures of the brainstem, making surgical removal impossible. The median survival after diagnosis is 9 to 11 months. Radiation therapy offers a brief respite, a temporary slowing, but the disease is almost uniformly fatal. For decades, oncologists had little more than palliative care to offer.
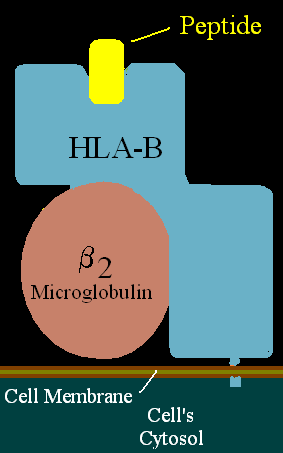
The molecular basis of DMG began to crystallize in the 2010s. A high percentage of these tumors carry a specific mutation, dubbed H3K27M, in a histone protein. Histones are the spools around which DNA is wound, and chemical tags on them—like the methylation mark at position K27—act as master switches, controlling whether genes are active or silent. The H3K27M mutation hijacks this system. It recruits a protein called EZHIP that mimics the mutation’s effects, effectively jamming the “off” switch for crucial tumor-suppressor genes. The result is epigenetic chaos: the cell’s normal instruction manual is scrambled, driving uncontrolled growth.
This knowledge revealed a new, glaring vulnerability. The problem was epigenetic, rooted in the misregulation of DNA and histone tags. Could you find a molecule that could reset the system? That’s where the long-dormant verticillin A re-enters the picture.
Verticillin A belongs to a notorious family called epipolythiodioxopiperazine (ETP) alkaloids. These fungal-derived compounds are known for their fierce biological activity and their fiendish chemical structures. They are dense, compact, and often possess a reactive bridge of sulfur atoms. For verticillin A, the devil was in two seemingly minor details: two extra oxygen atoms positioned on its complex framework. These atoms, essential for its anti-cancer activity, also made the molecule fall apart at the slightest provocation. Imagine a house of cards where two specific cards are made of tissue paper. The entire edifice collapses under the stress of most chemical manipulations. Every attempt to build it since 1970 had failed.
“The difference between an inactive analog and verticillin A is just two oxygens. But in synthetic chemistry, that’s the difference between a hill and a Himalayan peak,” explains Movassaghi. “Those oxygens create a polarity, a sensitivity that dictated our entire strategic approach. We couldn’t use traditional methods. We had to invent a new route that built the molecule’s core with surgical precision, protecting those delicate sites from the very beginning.”
A 16-Step Chemical Ballet
The MIT team’s synthesis, funded by the National Institutes of Health and pediatric cancer foundations, is a lesson in meticulous planning. Starting from a commercially available amino acid derivative called beta-hydroxytryptophan, they orchestrated a 16-step sequence. The climax was a dimerization reaction—taking two complex, ornate halves and stitching them together with perfect symmetry and correct three-dimensional orientation. Getting this step wrong would produce a useless mirror-image molecule or a scrambled mess.
They succeeded. The final, elegant proof was a set of data: nuclear magnetic resonance spectra, mass spectrometry readings, and optical rotation data that matched, point for point, the natural compound isolated 55 years prior. The synthetic molecule was not an approximation. It was an exact replica. The mountain was climbed.
But the summit was just a vantage point. With the ability to synthesize the core structure, the team could now do what was previously unimaginable: they could modify it. They could create “analogs”—chemical cousins—designed to be more stable, more potent, or more selective. This is the true engine of modern drug discovery.
In collaboration with Jun Qi’s lab at Dana-Farber Cancer Institute and Harvard Medical School, they did exactly that. They created a series of verticillin A derivatives. One key modification was N-sulfonylation—attaching a sulfur-based group to a nitrogen atom. This simple change acted like a suit of armor, dramatically improving the molecule’s stability without killing its cancer-fighting power.
Then came the critical tests. The researchers exposed plates of cancer cells to these new compounds. The results were stark and selective. The verticillin derivatives potently killed DMG cell lines that expressed high levels of the EZHIP protein—the very driver of the tumor’s epigenetic dysregulation. Meanwhile, they largely spared normal human cells. This selectivity is the holy grail of chemotherapy; the difference between a treatment and poison.
Mechanistic studies revealed the molecules were working exactly as hoped, operating on the epigenetic level. They induced DNA hypermethylation (adding “off” switches to DNA), elevated levels of the corrective H3K27me3 histone mark, and ultimately triggered apoptosis—programmed cell death—in the tumor cells. The fungal molecule, engineered by human hands, was speaking the cancer’s own corrupted language to tell it to die.
The synthesis of verticillin A is not a cure. It is a definitive, hard-won beginning. It transforms a pharmaceutical phantasm into a physical substance that can be weighed, measured, tested, and improved. It shifts the question from “Can we ever make this?” to “What can we make from this?” For a field desperate for new directions, especially in pediatric neuro-oncology, that shift is everything. It opens a door that had been welded shut for generations. What lies on the other side is a long road of preclinical and clinical testing, but it is, for the first time, a road that can actually be traveled.
Chemical Judo and the Two-Oxygen Problem
The real story of verticillin A's synthesis isn't in the final molecule. It's in a single, catastrophic design flaw discovered over decades of failure. The compound differs from a simpler, more stable analog called (+)-11,11'-dideoxyverticillin A by just two oxygen atoms. This fact seems trivial. In the logic of organic synthesis, it's everything. Those two atoms change the entire molecular personality.
"Those two oxygen atoms dramatically narrow the conditions under which reactions can occur. They make the molecule so much more fragile, so much more sensitive to almost any chemical operation you attempt." — Mohammad Movassaghi, MIT Professor of Chemistry
Think of building two structurally identical skyscrapers. One uses standard steel beams. The other uses a specialized, super-strong alloy that, unfortunately, warps if the temperature in the construction yard fluctuates by a single degree. The blueprint is the same. The construction process becomes a nightmare of controlled environments and impossible precision. This was the verticillin problem. Every published attempt to synthesize it prior to December 2025 failed because conventional chemical "tools" – acids, bases, common catalysts – would either destroy the sensitive oxygens or scramble the geometry around them.
The MIT team's breakthrough was an act of chemical judo. Instead of fighting the molecule's instability, they designed a 16-step sequence that respected it from the very first move. The conventional wisdom, drawn from the synthesis of the simpler analog, was to form certain critical bonds, particularly the carbon-sulfur linkages that form the molecule’s reactive disulfide bridge, late in the process. This was standard practice: build the skeleton, then add the delicate features. For verticillin A, standard practice was a guaranteed dead end.
"We realized the timing of the events is absolutely critical. You can't just follow the old roadmap and expect to arrive at a different, more delicate destination. We had to completely redesign the synthetic sequence, introducing and protecting key functionality much earlier to avoid those catastrophic late-stage failures." — Movassaghi, on the strategic redesign
The synthesis began with beta-hydroxytryptophan, an amino acid derivative. From that starting block, they performed a high-wire act, adding alcohols, ketones, and amides in a precise order, all while maintaining the absolute stereochemical configuration of what would become eight stereocenters. One wrong spatial turn at any step would derail the entire effort, yielding a biologically useless mirror image. The culmination was a dimerization reaction—fusing two highly complex, identically crafted halves together with perfect symmetry. The publication of this route in the Journal of the American Chemical Society on December 3, 2025, wasn't just a paper. It was a new playbook for tackling a whole class of "undruggable" natural products.
Stability Through Design: The Analogs Take Over
Here is the first contrarian observation about this breakthrough: the natural verticillin A molecule itself is probably not the future drug. It is the prototype, the foundational patent from which improved models are built. The moment the MIT chemists had their hands on reliable quantities of the pure compound, they immediately began breaking its own rules. They engineered derivatives. And in a beautiful twist of scientific irony, these human-designed analogs outperformed the natural product forged by millions of years of fungal evolution.
The most critical modification is called N-sulfonylation. By attaching a sulfonyl group to a nitrogen atom in the verticillin core, the chemists did something remarkable. They armored it. The molecule retained—and in some cases enhanced—its cancer-killing power while gaining a resilience that the fragile natural product utterly lacked. This is where scalable drug production truly begins. A molecule that decomposes on a lab bench can never become a medicine; a stabilized analog can be formulated, bottled, tested in animals, and, eventually, administered to a patient.
Collaboration turned the chemical achievement into a biological one. Movassaghi’s team shipped their new compounds to Jun Qi’s laboratory at Dana-Farber Cancer Institute and Harvard Medical School. The task was to throw them at the grim reality of diffuse midline glioma. The researchers didn't test on generic "cancer cells." They used carefully characterized DMG cell lines, some with high expression of the EZHIP protein, the epigenetic mastermind of the tumor, and others without.
The results, detailed in the same landmark publication, were starkly selective. The verticillin derivatives, particularly the N-sulfonylated versions, showed potent activity against the EZHIP-high DMG cells. They induced a cascade of epigenetic correction: DNA hypermethylation, a restoration of the crucial H3K27me3 histone mark, and finally, apoptosis. The tumor cells, whose survival depended on epigenetic chaos, were methodically shut down by a molecule that reversed the chaos. Normal cells were largely spared. This is the definition of a targeted therapeutic effect.
"The natural molecule itself is not the strongest, but making it allowed us to design and study better versions. We are not slaves to what the fungus made; we are now its engineers." — Mohammad Movassaghi, on the power of synthetic derivatives
The Brutal Calculus of Pediatric Neuro-Oncology
To understand why this work matters, you must sit with the numbers that define diffuse midline glioma. It strikes roughly 100 to 200 children in the United States each year. The median survival is 9 to 11 months from diagnosis. For over a decade, the standard of care has been radiation therapy, a treatment that can briefly stall the tumor’s growth but offers no cure. The clinical trial landscape is a graveyard of failed approaches. Why?
Most chemotherapies are useless. The blood-brain barrier, a protective shield, keeps them out. DMG’s location in the brainstem rules out meaningful surgery. The rapid progression leaves almost no time for iterative treatment. This creates a pharmaceutical development Catch-22: the patient population is tragically small, which discourages massive investment from large pharmaceutical companies, yet the biological complexity of the tumor demands expensive, high-risk, bespoke research. Diseases with larger markets attract more dollars and more shots on goal. DMG gets charity runs and academic grit.
This context transforms the verticillin synthesis from a cool chemical trick into a strategic asset. It creates an entirely new, target-validated chemical scaffold for a disease with virtually no good options. The EZHIP protein is a compelling target, but before December 2025, there were no small molecules known to selectively counteract its effects and subsequently kill the tumor cells. Now there is a structural template—a chemical "shape"—that does exactly that.
"Finding a compound that shows this level of selectivity for EZHIP-high DMG cells is exceptionally rare. It gives us a precise tool to probe the biology of this devastating tumor and, more importantly, a validated starting point for therapy development where almost none existed." — Jun Qi, Dana-Farber Cancer Institute
But here is the necessary skepticism, the critical eye a journalist must maintain. The path from a selective cell culture result to an approved drug is a gauntlet famed for its corpse-count. 16-step syntheses are economically daunting for large-scale production. Can the route be shortened? Can it be made cost-effective? The molecule must next prove it can cross the blood-brain barrier in an animal model, something no cell culture experiment can predict. It must show efficacy in a mouse model of DMG without debilitating toxicity. Then come pharmacokinetics, formulation, toxicology studies, and finally, Phase I clinical trials. The history of oncology is littered with compounds that shone in a petri dish and vanished in a mouse, or a human.
So, is the hype justified? Partially. The genuine achievement is the demolition of a fundamental roadblock: supply. For 55 years, any study of verticillin A’s medicinal potential was constrained by the minuscule, unreliable amounts painstakingly extracted from fungi. Now, the supply is limited only by the skill of organic chemists and the budget of a lab. This enables the kind of systematic optimization that defines modern drug discovery. It allows researchers to ask, and answer, questions that were previously off-limits: What part of the molecule is essential for crossing the blood-brain barrier? Can we tweak it to last longer in the bloodstream? Can we make it even more selective?
The synthesis is a foundational victory. It provides the field of pediatric neuro-oncology with a new piece on the chessboard, a piece with a unique and validated move set. The hard truth, however, is that the game is still overwhelmingly in the cancer’s favor. The real test is whether the scientific community can leverage this foundation quickly enough to matter for the children diagnosed next year, or the year after. The clock, as always with DMG, is the most unrelenting statistic of all.
A Blueprint for a Forgotten Pharmacy
The total synthesis of verticillin A reaches far beyond a single molecule or a single disease. Its true significance is methodological and philosophical. It proves that a class of molecules once deemed "undruggable" due to synthetic intractability is now within reach. This resurrects an entire library of forgotten natural products—compounds discovered in the 60s, 70s, and 80s, cataloged for promising activity, and then abandoned on the shelf because no one could make them. The fungal and bacterial kingdoms have been performing combinatorial chemistry for eons, producing structures of staggering complexity. For decades, we could only window-shop. The MIT work provides a set of lockpicks.
This shifts the paradigm in early drug discovery. The old model was one of scarcity: isolate milligrams from a natural source, run limited tests, and if the molecule was too hard to synthesize, abandon it. The new model, demonstrated here, is one of abundance and engineering. Synthesis provides not just the molecule, but the intellectual property and the means to improve upon nature’s design. It turns a dead-end observation into a starting line.
"This isn't just about one cancer drug. It's about validating a strategy. We are sending a message that no complex natural product is off-limits anymore. If there's compelling biology, we can build it, and then we can build it better. This should revive interest in hundreds of overlooked compounds sitting in old notebooks." — A pharmaceutical chemist specializing in natural products, who requested anonymity to speak freely
The impact is already rippling through specialized chemistry circles. Graduate students are dissecting the 16-step sequence, not just to memorize it, but to understand its strategic logic—the early-stage protections, the tailored dimerization. This synthesis will be taught in advanced courses as a case study in precision and planning. For the pediatric neuro-oncology community, it provides a rare jolt of genuine, mechanism-based optimism. Researchers now have a novel chemical probe to dissect EZHIP biology and a tangible candidate scaffold. In a field starved for viable clinical candidates, that’s more than a paper; it's a new weapon in the armory.
The Hard Road Ahead: A Realist's Critique
To report this story without skepticism would be professional malpractice. The chasm between a synthetically accessible, cell-active compound and an FDA-approved drug is vast, littered with brilliant failures. Let's articulate the specific, formidable hurdles that verticillin-based therapies must clear.
First, the blood-brain barrier. This is the sentinel that protects our brains and routinely denies entry to promising neuro-therapeutics. DMG resides behind it. The verticillin derivatives showed activity against DMG cells in a dish, where there is no barrier. Did they work because they can naturally cross, or because they were applied directly? No data published as of March 2026 demonstrates brain penetrance in a living animal. This is the next, absolutely non-negotiable experiment. If the molecules cannot cross, the project essentially ends, or requires a radical redesign that could strip its activity.
Second, the synthesis itself. A 16-step linear sequence is a production nightmare. The overall yield—the amount of final product you get from your starting material—drops with every step. Producing grams for preclinical studies is feasible in an academic lab. Producing kilograms for clinical trials requires a scalable, cost-effective process that almost certainly needs to be completely re-engineered. This demands a level of industrial chemistry expertise and investment that academic labs seldom possess.
Third, toxicity. Selectivity in a cell culture is promising, but not definitive. The unique biology of a developing child’s brain and body must be considered. ETP alkaloids, with their reactive disulfide bridges, can be proverbial grenades. Will they cause off-target epigenetic effects in healthy tissues? Could they trigger unforeseen neurotoxicity? The upcoming in vivo studies in mice, expected to commence in the second quarter of 2026, will provide the first harsh answers.
The history of cancer drug development is a graveyard of molecules that failed at one of these three altars: delivery, manufacturability, or safety. The verticillin program has elegantly solved the supply problem. The much harder problems of distribution and biocompatibility remain entirely unanswered.
What Comes Next
The immediate timeline is clear and unforgiving. Through mid-2026, the collaboration between MIT and Dana-Farber will focus on in vivo pharmacology. They will be formulating the most promising N-sulfonylated derivatives for mouse studies, with initial pharmacokinetic data—how the drug is absorbed, distributed, metabolized, and excreted—expected by late summer. The critical study, using mouse models of DMG that incorporate the human H3K27M mutation and EZHIP expression, is slated to begin before the end of the year. These results will be the real litmus test.
Concurrently, medicinal chemists will be busy. The published synthesis is a blueprint for creating not dozens, but hundreds of new analogs. The goal will be to improve brain penetration and pharmacokinetic profiles. Every atom on the verticillin core is now a potential handle for modification. This analog campaign is where the real drug candidate will likely emerge, perhaps looking quite different from the natural parent molecule.
By early 2027, the path will be obvious. Either the data will show sufficient efficacy and safety in animals to justify seeking orphan drug designation and partnership with a biotech company for clinical development, or the project will hit an insurmountable wall of toxicity or poor delivery. There is no middle ground for a disease this aggressive.
Does this story end with a cure for DMG? The odds remain heartbreakingly long. But it ends one thing definitively: the 55-year limbo of a molecule whose promise was trapped by its own elegant complexity. The fungal compound from 1970 is no longer a ghost in the literature. It is a tangible, weighable powder in a vial. It is a starting point. In the desperate race against a clock measured in months, providing a new starting line is sometimes the only victory science can deliver before the real marathon begins.
The mountain, at least, has been climbed. Now they must build a road down the other side.
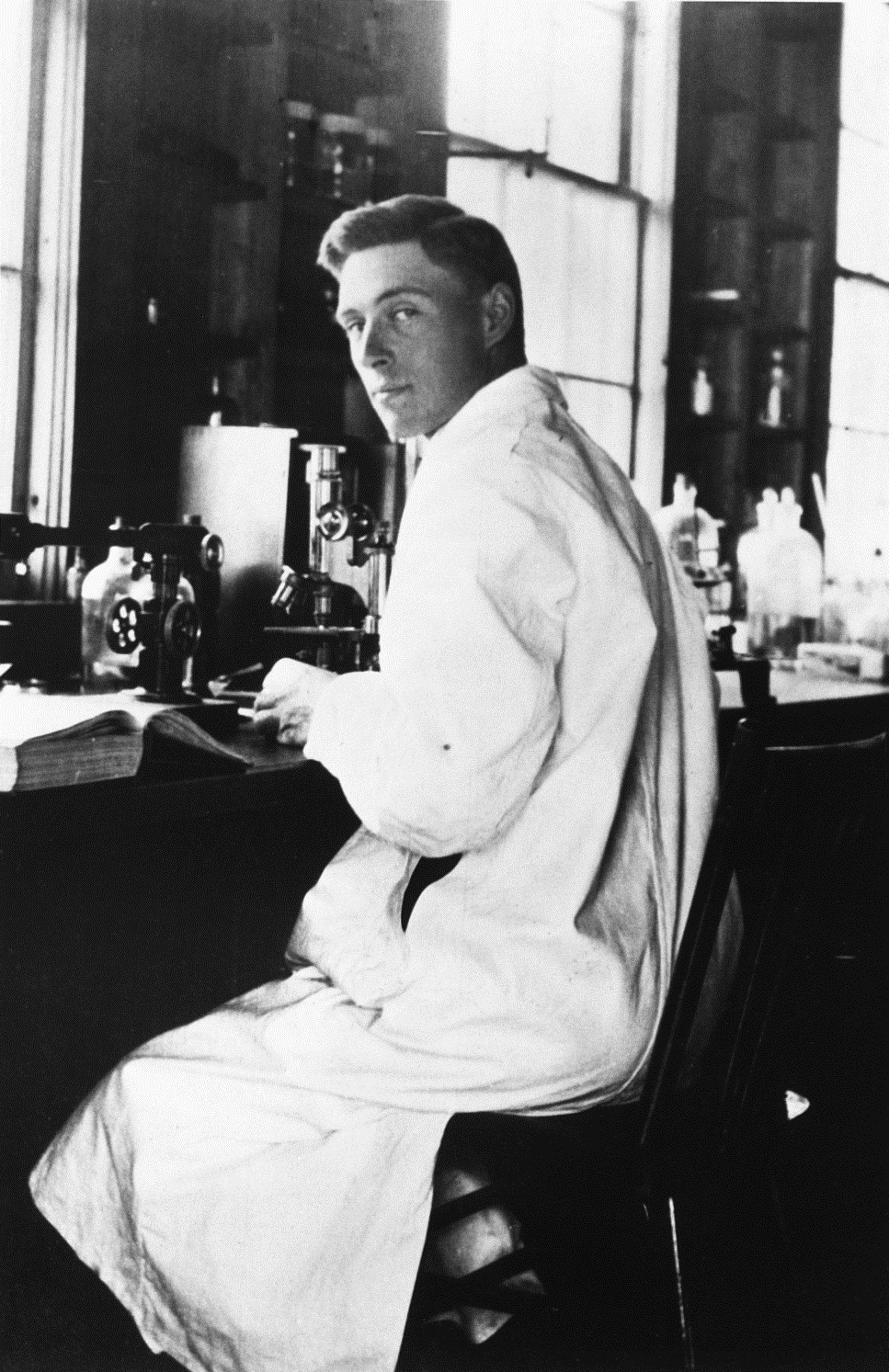
Robin Warren: Pionier der medizinischen Forschung
Der australische Pathologe John Robin Warren veränderte mit einer bahnbrechenden Entdeckung die Welt der Gastroenterologie für immer. Seine Arbeit, die zur Identifizierung des Bakteriums Helicobacter pylori führte, beendete ein medizinisches Dogma und revolutionierte die Behandlung von Magengeschwüren. Für diese Leistung erhielt er 2005, gemeinsam mit Barry J. Marshall, den Nobelpreis für Physiologie oder Medizin.
Warren, der am 23. Juli 2024 im Alter von 87 Jahren in Perth verstarb, gilt als einer der großen klinischen Beobachter des 20. Jahrhunderts. Seine Karriere, die sich über Jahrzehnte am Royal Perth Hospital erstreckte, steht beispielhaft für die Kraft der histologischen Forschung und des genauen Hinsehens. Dieser Artikel beleuchtet das Leben und das wegweisende Vermächtnis dieses medizinischen Pioniers.
Frühes Leben und medizinische Laufbahn
John Robin Warren wurde am 11. Juni 1937 in Adelaide, Australien, geboren. Sein Weg in die Medizin führte ihn an die University of Adelaide, wo er sein Studium 1961 erfolgreich abschloss. Die Wahl der Pathologie als Fachgebiet erwies sich als entscheidend für seine spätere Entdeckung.
Den Großteil seiner beruflichen Tätigkeit verbrachte Warren als leitender Pathologe am Royal Perth Hospital. Hier entwickelte er seine Expertise in der mikroskopischen Untersuchung von Gewebeproben. Seine akribische Arbeitsweise und sein Interesse an scheinbar unbedeutenden Details prägten seinen Forschungsstil und sollten schließlich zu einem Paradigmenwechsel führen.
Bis zu seinem Ruhestand im Jahr 1999 blieb Warren dieser Institution verbunden. Seine Arbeit war stets von einem tiefen Verständnis für die klinischen Implikationen der Pathologie geprägt. Dieser klinisch-pathologische Ansatz wurde zum Fundament seiner historischen Entdeckung.
Die historische Entdeckung von Helicobacter pylori
Ende der 1970er Jahre stieß Warren bei der Untersuchung von Magenbiopsien unter dem Mikroskop immer wieder auf ein ungewöhnliches Phänomen. In den Proben von Patienten mit Gastritis oder Magengeschwüren entdeckte er kurvige Bakterien, die sich in der Schleimhautschicht des Magens ansiedelten.
Ein Dogma gerät ins Wanken
Bis zu diesem Zeitpunkt war die vorherrschende medizinische Lehrmeinung, dass der menschliche Magen aufgrund der starken Säure steril sei. Die Ursachen für peptische Ulzera (Magen- und Zwölffingerdarmgeschwüre) wurden hauptsächlich in Faktoren wie Stress, Übersäuerung oder einer genetischen Veranlagung gesehen. Warrens Beobachtung stellte dieses langjährige Dogma fundamental in Frage.
Die Kombination aus histologischer Beobachtung, Kultivierungstechnik und späteren klinischen Studien führte zur breiten Akzeptanz der neuen Theorie.
Warrens Entdeckung war zunächst ein solitärer Befund. Die entscheidende Wende kam durch die Zusammenarbeit mit dem jungen Assistenzarzt Barry J. Marshall. Marshall gelang es, die von Warren beschriebenen Bakterien zu kultivieren, was den wissenschaftlichen Nachweis erheblich vorantrieb. Gemeinsam entwickelten sie die Hypothese, dass dieses Bakterium, später Helicobacter pylori genannt, die primäre Ursache für Gastritis und viele Geschwüre ist.
Der Weg zum Nobelpreis 2005
Die Widerstände gegen die neue Theorie waren anfangs immens. Um die Koch'schen Postulate zu erfüllen und einen kausalen Zusammenhang zu beweisen, unternahm Barry Marshall 1984 einen spektakulären Selbstversuch. Die darauf folgende Erkrankung und erfolgreiche Behandlung stärkte die Evidenz entscheidend.
In den folgenden Jahren untermauerten zahlreiche internationale Studien die Verbindung zwischen H. pylori und peptischen Ulzera. Die Entwicklung zuverlässiger diagnostischer Tests, wie des Urease-Atemtests, trug maßgeblich zur Verbreitung der neuen Erkenntnisse in der klinischen Praxis bei. Die bahnbrechende Arbeit von Warren und Marshall führte zu einem völlig neuen Therapieansatz.
Für die Entdeckung des Bakteriums Helicobacter pylori und seine Rolle bei der Entstehung von Gastritis und Magengeschwüren wurden J. Robin Warren und Barry J. Marshall im Jahr 2005 mit dem Nobelpreis für Physiologie oder Medizin ausgezeichnet. Das Nobelkomitee würdigte damit eine Entdeckung, die die Lebensqualität von Millionen Patienten weltweit verbesserte.
Klinische Folgen und ein neues Therapiezeitalter
Die Anerkennung der bakteriellen Ursache führte zu einem radikalen Wandel in der Behandlung von Magen- und Zwölffingerdarmgeschwüren. Anstelle von rein säurehemmenden Medikamenten oder chirurgischen Eingriffen trat nun eine Eradikationstherapie mit Antibiotika in Kombination mit Protonenpumpenhemmern.
- Reduktion von Rezidiven: Die antibiotische Behandlung von H. pylori führte zu einer dramatischen Verringerung der Wiederauftrittsrate von Geschwüren.
- Rückgang der Operationen: Weltweit ging die Zahl der notwendigen chirurgischen Eingriffe zur Ulkusbehandlung stark zurück.
- Neue Diagnostik: Einfache nicht-invasive Tests, wie der Atemtest, wurden Standard in der Diagnostik.
Warrens initiale histologische Beobachtung legte somit den Grundstein für eine der bedeutendsten Veränderungen in der klinischen Medizin des späten 20. Jahrhunderts. Aus einem chronischen, oft rezidivierenden Leiden wurde eine in der Regel heilbare Infektionskrankheit.
Das Vermächtnis eines klinischen Beobachters
Robin Warrens Vermächtnis geht weit über den Nobelpreis hinaus. Er verkörperte den Typus des neugierigen, detailversessenen Wissenschaftlers, der einer Beobachtung so lange nachgeht, bis sie erklärt ist. Seine Arbeit betonte stets die fundamentale Bedeutung der Pathologie als Brücke zwischen Grundlagenforschung und patientennaher Anwendung.
Sein Ansatz, "genau hinzusehen", wie es in Nachrufen oft heißt, führte nicht nur zu einer medizinischen Revolution, sondern auch zu einem Umdenken in der Ausbildung. Kliniker weltweit wurden für die Bedeutung mikroskopischer Diagnostik und eine enge Zusammenarbeit mit Pathologen sensibilisiert. Warren bewies, dass eine einzelne, sorgfältige Beobachtung ein ganzes medizinisches Fachgebiet auf den Kopf stellen kann.
Dieses Vermächtnis ist in jedem Labor und bei jeder Magenspiegelung präsent, bei der heute aktiv nach Helicobacter pylori gesucht wird. Warren hat gezeigt, dass wissenschaftlicher Fortschritt oft mit dem Hinterfragen von scheinbar feststehenden Tatsachen beginnt.
Rolle in der Krebsprävention und globale Auswirkungen
Die Entdeckung von Helicobacter pylori hatte nicht nur Auswirkungen auf die Behandlung von Geschwüren, sondern eröffnete auch völlig neue Perspektiven in der Krebsprävention. Epidemiologische Studien zeigten einen klaren Zusammenhang zwischen einer chronischen H. pylori-Infektion und einem erhöhten Risiko für bestimmte Magenkrebsarten, insbesondere das Magenkarzinom.
Neue Strategien in der Onkologie
Diese Erkenntnis führte zu einem strategischen Umdenken. Die Eradikation von H. pylori wird seither nicht mehr nur als Therapie für Geschwüre, sondern zunehmend auch als potenzielle präventive Maßnahme in Betracht gezogen. In Hochrisikopopulationen, wie in Regionen mit hoher Magenkrebsinzidenz, kann die frühzeitige Behandlung der Infektion das Krebsrisiko signifikant senken.
Internationale Leitlinien, beispielsweise der Weltgesundheitsorganisation (WHO), klassifizieren H. pylori mittlerweile als Karzinogen der Gruppe 1. Damit ist das Bakterium eindeutig als krebserregend für den Menschen eingestuft. Diese Einstufung unterstreicht die weitreichende Bedeutung von Warrens und Marshalls Entdeckung für die öffentliche Gesundheit.
Die globale Krankheitslast durch Magenkrebs konnte durch diesen neuen Ansatz bereits positiv beeinflusst werden. Die gezielte Bekämpfung eines bakteriellen Erregers zur Krebsprävention war vor Warrens Arbeit ein kaum vorstellbares Konzept und markiert einen Meilenstein in der präventiven Medizin.
Aktuelle Herausforderungen: Antibiotikaresistenzen
Trotz des großen Erfolgs der Eradikationstherapie sieht sich die moderne Medizin heute mit einer wachsenden Herausforderung konfrontiert: Antibiotikaresistenzen. Helicobacter pylori-Stämme entwickeln zunehmend Resistenzen gegen Standardantibiotika wie Clarithromycin und Metronidazol.
- Regionale Variation: Die Resistenzraten variieren global stark und erfordern lokale Anpassungen der Therapieprotokolle.
- Therapieversagen: Resistenzen führen zu einer erhöhten Rate an Therapieversagen, was die Behandlung komplexer und kostenintensiver macht.
- Leitlinien-Anpassung: Fachgesellschaften passen ihre Empfehlungen kontinuierlich an, basierend auf aktuellen Resistenzdaten, und empfehlen zunehmend Kombinationstherapien oder Resistenztestungen.
Diese Entwicklung unterstreicht die Dynamik im Feld, das Warren mitbegründet hat. Die Forschung konzentriert sich nun auf die Entwicklung neuer Therapieregimes, die auch gegen resistente Stämme wirksam sind. Es ist ein fortlaufender Kampf, der die anhaltende Relevanz der H. pylori-Forschung beweist.
Die gezielte Bekämpfung eines bakteriellen Erregers zur Krebsprävention war vor Warrens Arbeit ein kaum vorstellbares Konzept.
Auszeichnungen und späte Würdigungen
Neben dem Nobelpreis erhielten J. Robin Warren und Barry J. Marshall zahlreiche weitere prestigeträchtige Auszeichnungen, die ihre Arbeit schon vor der breiten Nobelpreis-Würdigung anerkannten. Diese Preise spiegelten die wachsende Akzeptanz und die revolutionäre Bedeutung ihrer Entdeckung in der Fachwelt wider.
Bedeutende Preise im Überblick
Bereits 1994 wurden die beiden Forscher mit dem Warren Alpert Foundation Prize ausgezeichnet. 1997 folgte einer der renommiertesten deutschen Forschungspreise, der Paul-Ehrlich-und-Ludwig-Darmstaedter-Preis. Diese Ehrungen kamen zu einem Zeitpunkt, als sich die neue Theorie international durchgesetzt hatte und ihren Siegeszug in den klinischen Leitlinien antrat.
Die höchste australische zivile Ehrung erhielt Warren im Jahr 2007, als er zum Companion of the Order of Australia ernannt wurde. Diese Auszeichnung würdigte nicht nur seinen wissenschaftlichen Dienst, sondern seinen herausragenden Beitrag zum Wohlstand der australischen Nation und der gesamten Menschheit.
Jede dieser Ehrungen markiert einen Schritt auf dem Weg von einer umstrittenen Hypothese hin zu einem unumstößlichen Bestandteil des medizinischen Wissens. Sie zeichnen die Karriere eines Mannes nach, der unbeirrt an seiner Beobachtung festhielt.
Die Methodik: Vom Mikroskop zur klinischen Studie
Warrens Erfolg basierte auf einer konsequenten und methodisch vielschichtigen Herangehensweise. Sie begann am Mikroskop, fand aber erst durch die Integration weiterer Disziplinen ihren Weg in die weltweite klinische Praxis. Dieser methodische Mix war entscheidend für den letztendlichen Durchbruch.
Die ersten Schritte waren rein histologischer Natur. Warren dokumentierte systematisch das Vorkommen der unbekannten Bakterien in Gewebeproben und korrelierte seinen Befund mit dem klinischen Zustand der Patienten. Dieser pathologische Ansatz lieferte die initiale Hypothese.
Der nächste, entscheidende Schritt war die Kultivierung des Erregers durch Barry Marshall. Erst mit einem reinen Bakterienstamm konnten experimentelle und klinische Studien durchgeführt werden. Die Kombination aus Pathologie und Mikrobiologie schuf eine solide wissenschaftliche Basis.
Den abschließenden Beweis erbrachten dann klinische Interventionsstudien. Sie zeigten, dass die antibiotische Eradikation von H. pylori tatsächlich zur Abheilung von Geschwüren und zur dauerhaften Verhinderung von Rezidiven führte. Dieser Dreiklang aus Beobachtung, Experiment und klinischer Bestätigung ist bis heute ein Musterbeispiel für erfolgreiche medizinische Forschung.
Tod und weltweite Reaktionen
J. Robin Warren verstarb am 23. Juli 2024 friedlich in Perth im hohen Alter von 87 Jahren. Die Nachricht von seinem Tod löste weltweit eine Welle der Würdigung und des Gedenkens aus. Fachgesellschaften, Universitäten und ehemalige Kollegen betonten unisono seinen bescheidenen Charakter und seinen unerschütterlichen Forschungswillen.
Medien auf der ganzen Welt hoben die globale Bedeutung seiner Entdeckung hervor. Sie betonten, wie seine Arbeit direkt dazu beigetragen hat, menschliches Leid zu lindern und lebensverändernde Behandlungen zu etablieren. Sein Tod markierte das Ende einer Ära, aber die Prinzipien seiner Forschung bleiben lebendig.
Barry J. Marshall, sein langjähriger Partner und Mit-Nobelpreisträger, würdigte Warren als ruhigen und präzisen Denker, dessen Entdeckung ohne seine akribische Arbeit am Mikroskop niemals möglich gewesen wäre. Diese Partnerschaft zwischen dem geduldigen Pathologen und dem draufgängerischen Kliniker wurde als ideale Symbiose für den wissenschaftlichen Fortschritt beschrieben.
Die Lehren aus Warrens Karriere für junge Forscher
Die Laufbahn von Robin Warren bietet zahlreiche wertvolle Lektionen für angehende Wissenschaftler und Ärzte. Sie ist ein Lehrstück darüber, wie wichtige Entdeckungen oft jenseits der ausgetretenen Pfade gemacht werden und welche persönlichen Eigenschaften diesen Erfolg ermöglichen.
Die Kraft der Beharrlichkeit
Warrens Weg war nicht einfach. Seine Beobachtungen wurden zunächst von vielen etablierten Kollegen und Fachzeitschriften angezweifelt oder ignoriert. Seine Beharrlichkeit und sein Glaube an die eigene sorgfältige Arbeit waren entscheidend, um diese Phase des Widerstands zu überstehen. Dies unterstreicht, wie wichtig intellektuelle Unabhängigkeit in der Forschung ist.
Eine weitere zentrale Lehre ist der Wert der klinischen Beobachtung. In einem Zeitalter hochtechnisierter Medizin demonstrierte Warren, dass das geschulte Auge und die Frage nach dem "Warum" immer noch zu den mächtigsten Werkzeugen eines Arztes gehören. Seine Arbeit begann nicht mit einem teuren Gerät, sondern mit Neugier und einem Mikroskop.
Schließlich zeigt seine Kooperation mit Marshall die Bedeutung interdisziplinärer Zusammenarbeit. Warrens pathologischer Befund allein hätte nicht ausgereicht; Marshalls klinische und mikrobiologische Expertise war nötig, um die Theorie zu beweisen. Erfolg entsteht oft an den Schnittstellen der Fächer.
Helicobacter pylori heute: Stand der Forschung 2025
Die Forschung zu Helicobacter pylori ist auch fast 50 Jahre nach seiner Entdeckung hoch dynamisch. Die aktuellen Schwerpunkte spiegeln sowohl die Erfolge als auch die neuen Herausforderungen wider, die aus der bahnbrechenden Arbeit von Warren und Marshall erwachsen sind.
- Präzisionsmedizin: Die Behandlung wird zunehmend individualisiert, basierend auf lokalen Resistenzmustern und genetischen Markern des Bakteriums, um die Eradikationsraten weiter zu steigern.
- Impfstoffentwicklung: Obwohl immer noch herausfordernd, bleibt die Entwicklung eines prophylaktischen oder therapeutischen Impfstoffs ein langfristiges Ziel, um die Infektion und ihre Folgen grundlegend zu bekämpfen.
- Mikrobiom-Interaktion: Forscher untersuchen intensiv die Wechselwirkung von H. pylori mit dem restlichen Magen- und Darmmikrobiom und deren Einfluss auf die Krankheitsentstehung.
- Früherkennungsstrategien: In Hochrisikoregionen werden Programme zur gezielten Früherkennung und Eradikation von H. pylori als Teil von Magenkrebs-Präventionsprogrammen evaluiert und implementiert.
Seine Arbeit begann nicht mit einem teuren Gerät, sondern mit Neugier und einem Mikroskop.
Damit bleibt H. pylori ein faszinierender Modellerreger, an dem grundlegende Prinzipien der chronischen Infektion, Krebsentstehung und Wirt-Pathogen-Interaktion erforscht werden. Warrens Erbe lebt in jedem dieser Forschungsprojekte fort.
Fazit: Ein Pionier, der die Medizin neu definierte
Robin Warrens Lebenswerk steht für einen der größten Paradigmenwechsel in der Medizingeschichte des 20. Jahrhunderts. Er verwandelte die Sichtweise auf die Volkskrankheit "Maggengeschwür" von einem lebensstilbedingten, chronischen Leiden in eine heilbare Infektionskrankheit. Dieser Perspektivwechsel rettete unzähligen Patienten invasive Operationen und brachte ihnen nachhaltige Heilung.
Seine Karriere demonstriert die transformative Macht der Grundlagenforschung in der Pathologie. Sie beweist, dass die scheinbar stille Arbeit am Mikroskop die Kraft hat, klinische Leitlinien weltweit umzuschreiben und neue Standards der Versorgung zu setzen. Warren war kein lauter Revolutionär, sondern ein stiller Beobachter, dessen Beobachtungen die Welt lauter erschallen ließen.
Das anhaltende Vermächtnis
Das Vermächtnis von J. Robin Warren ist in jeder erfolgreichen Eradikationstherapie, in jedem vermiedenen chirurgischen Eingriff und in jeder präventiven Magenkrebs-Beratung greifbar. Er hat gezeigt, dass wissenschaftlicher Fortschritt Geduld, Genauigkeit und den Mut erfordert, etablierte Wahrheiten in Frage zu stellen.
Seine Geschichte ist eine zeitlose Erinnerung daran, dass große Entdeckungen manchmal direkt vor unseren Augen liegen – wir müssen nur, wie Robin Warren, genau hinsehen. Sein Beitrag zur Menschheit wird weiterleben, solange Ärzte Magengeschwüre mit einer einfachen Antibiotikakur heilen können. In der Geschichte der Medizin bleibt sein Name für immer mit der Überwindung eines Dogmas und dem Beginn einer neuen Ära der gastroenterologischen Heilkunst verbunden.
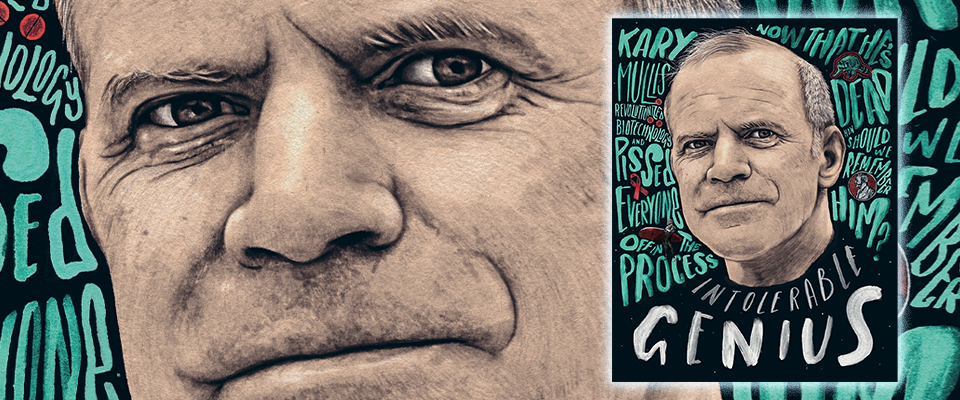
Kary Mullis and the PCR Revolution in DNA Analysis
Kary Mullis, the American biochemist, is renowned for fundamentally transforming molecular biology. His invention, the polymerase chain reaction (PCR), became one of the most significant scientific techniques of the 20th century. This article explores the life, genius, and controversies of the Nobel laureate who gave science the power to amplify DNA.
Who Was Kary Mullis?
Kary Banks Mullis was born on December 28, 1944, in Lenoir, North Carolina. He died at age 74 on August 7, 2019, in Newport Beach, California. Best known as the architect of PCR, Mullis was a brilliant yet unconventional figure.
His work earned him the 1993 Nobel Prize in Chemistry, which he shared with Michael Smith. Beyond his monumental scientific contribution, Mullis’s life was marked by eccentric personal pursuits and controversial views that often placed him at odds with the scientific mainstream.
Early Life and Academic Foundation
Mullis’s journey into science began with foundational education in chemistry. He earned his Bachelor of Science in Chemistry from the Georgia Institute of Technology in 1966. This undergraduate work provided the critical base for his future research.
He then pursued a Ph.D. in biochemistry at the University of California, Berkeley. Mullis completed his doctorate in 1972 under Professor J.B. Neilands. His doctoral research focused on the structure and synthesis of microbial iron transport molecules.
An Unconventional Career Path
After earning his Ph.D., Kary Mullis took a highly unusual detour from science. He left the research world to pursue fiction writing. During this period, he even spent time working in a bakery, a stark contrast to his future in a biotechnology lab.
This hiatus lasted roughly two years. Mullis eventually returned to scientific work, bringing with him a uniquely creative and unorthodox perspective. His non-linear path highlights the unpredictable nature of scientific discovery and genius.
The Invention of the Polymerase Chain Reaction (PCR)
The polymerase chain reaction invention is a landmark event in modern science. Mullis conceived the technique in 1983 while working as a DNA chemist at Cetus Corporation, a pioneering California biotechnology firm. His role involved synthesizing oligonucleotides, the short DNA strands crucial for the process.
The iconic moment of inspiration came not in a lab, but on a night drive. Mullis was traveling to a cabin in northern California with colleague Jennifer Barnett. He later recounted that the concept of PCR crystallized in his mind during that spring drive, a flash of insight that would change science forever.
PCR allows a specific stretch of DNA to be copied billions of times in just a few hours.
How Does PCR Work? The Basic Principle
The PCR technique is elegantly simple in concept yet powerful in application. It mimics the natural process of DNA replication but in a controlled, exponential manner. The core mechanism relies on thermal cycling and a special enzyme.
The process involves three key temperature-dependent steps repeated in cycles:
- Denaturation: High heat (around 95°C) separates the double-stranded DNA into two single strands.
- Annealing: The temperature is lowered to allow short DNA primers to bind to complementary sequences on each single strand.
- Extension: The temperature is raised to an optimal level for a heat-stable DNA polymerase enzyme to synthesize new DNA strands by adding nucleotides.
Each cycle doubles the amount of target DNA. After 30 cycles, this results in over a billion copies, enabling detailed analysis of even the smallest genetic sample.
Initial Scientific Rejection and Eventual Publication
Despite its revolutionary potential, Mullis’s PCR concept initially faced significant skepticism from the scientific establishment. His original manuscript detailing the method was rejected by two of the world’s most prestigious journals.
- The journal Nature declined to publish it in 1985, suggesting it might be better for a more specialized publication.
- Science magazine rejected it just one month later, stating the paper could not compete for their limited space.
The groundbreaking work was finally published in the journal Methods in Enzymology. This early rejection is a classic example of how transformative ideas can struggle for acceptance before their immense value is universally recognized.
The Immense Impact and Applications of PCR
The impact of PCR is nearly impossible to overstate. It became an indispensable tool across a vast spectrum of fields almost overnight. The technique’s ability to amplify specific DNA sequences with high fidelity and speed opened new frontiers.
It fundamentally changed the scale and speed of genetic research. Experiments that once took weeks or required large amounts of biological material could now be completed in hours with minute samples.
Revolutionizing Medical Research and Diagnostics
In medical diagnostics, PCR became a game-changer. It enabled the rapid detection of pathogenic bacteria and viruses long before traditional culture methods could. This speed is critical for effective treatment and containment of infectious diseases.
The technique is central to genetic testing for hereditary conditions. It allows clinicians to identify specific mutations with precision, facilitating early diagnosis and personalized medicine strategies for countless patients worldwide.
Transforming Forensic Science and Criminal Justice
Forensic science was revolutionized by the advent of PCR. The method allows crime labs to generate analyzable DNA profiles from extremely small or degraded biological evidence. This includes traces like a single hair follicle, a tiny spot of blood, or skin cells.
This capability has made DNA evidence a cornerstone of modern criminal investigations. It has been instrumental in both convicting the guilty and exonerating the wrongly accused, dramatically increasing the accuracy of the justice system.
Enabling Major Breakthroughs in Genetics
PCR was the catalyst for the monumental Human Genome Project. The project, which mapped the entire human genetic code, relied heavily on PCR to amplify DNA segments for sequencing. This would have been technologically and economically infeasible without Mullis’s invention.
In basic genetic research, PCR allows scientists to clone genes, study gene expression, and investigate genetic variation. It remains the foundational technique in virtually every molecular biology laboratory on the planet.
Back from the Bakery: Joining Cetus Corporation and the Road to PCR
After his departure from science, Kary Mullis rejoined the scientific community with renewed perspective. In 1979, he secured a position as a DNA chemist at Cetus Corporation in Emeryville, California. This biotech company was a hotbed of innovation, focusing on pharmaceutical products and recombinant DNA technology.
His primary role involved the chemical synthesis of oligonucleotides, short strands of DNA. These custom-built DNA fragments were essential tools for other scientists at Cetus. Synthesizing them was a tedious, manual process, requiring meticulous attention to detail.
This hands-on work with the fundamental building blocks of genetics proved crucial. It gave Mullis an intimate, practical understanding of DNA chemistry. This foundational knowledge was the perfect precursor to his revolutionary insight into DNA amplification.
The Eureka Moment: A Drive Through the Mountains
The story of PCR's conception has become legendary in scientific lore. In the spring of 1983, Mullis was driving to a cabin he was building in Mendocino County with his colleague, Jennifer Barnett. The California buckeyes were in bloom, scenting the night air.
As he navigated the winding roads, his mind was working on a problem. He was trying to find a better way to detect point mutations in DNA, a task that was notoriously difficult with existing methods. Suddenly, the complete concept for the polymerase chain reaction unfolded in his mind.
He later described visualizing the process: the double helix splitting, primers binding, and the enzyme building new strands, all happening repeatedly in a test tube.
Mullis pulled over to jot down notes and run calculations. He realized that the process could be exponential. A single DNA molecule could be amplified to billions of copies in just a few hours. This was the birth of a methodology that would redefine genetic engineering.
The Critical Role of Thermostable Enzymes
An initial challenge with PCR was the enzyme. Early experiments used the E. coli DNA polymerase, which was heat-sensitive. Since the first step of each PCR cycle required high heat to denature the DNA, the enzyme would be destroyed after the first cycle.
This meant scientists had to manually add fresh enzyme after each heating step, making the process impractical. The breakthrough came with the adoption of Taq polymerase, an enzyme isolated from the heat-loving bacterium Thermus aquaticus found in hot springs.
- Taq polymerase is thermostable, surviving the high temperatures of the denaturation step.
- This allowed the entire PCR process to be automated in a thermal cycler machine.
- The automation of PCR was the final piece that turned a brilliant concept into a practical, world-changing tool.
Achieving the Peak: The 1993 Nobel Prize in Chemistry
The significance of Kary Mullis's invention was formally recognized a decade after its conception. In 1993, the Royal Swedish Academy of Sciences awarded him the Nobel Prize in Chemistry. He shared the prestigious award with Michael Smith, who was honored for his work on site-directed mutagenesis.
The Nobel committee stated that PCR "has already had a decisive influence on research in basic biology, medicine, biotechnology, and forensic science." This acknowledgment cemented PCR's status as one of the most important scientific techniques ever developed.
Mullis's Nobel lecture, titled "The Polymerase Chain Reaction," detailed the method's conception and its profound implications. The prize brought him international fame and solidified his legacy within the scientific community, despite his later controversial stances.
The Significance of the Nobel Recognition
Winning a Nobel Prize is the pinnacle of scientific achievement. For Mullis, it validated his unconventional thought process and the power of a simple, elegant idea. The prize highlighted how a fundamental methodological advance could have a broader impact than a specific discovery.
The recognition also underscored the growing importance of biotechnology. PCR was a tool that originated in a biotech company, Cetus, demonstrating how industry research could drive fundamental scientific progress. The award brought immense prestige to the fledgling biotech sector.
Controversies Surrounding the Prize
As with many monumental discoveries, the Nobel Prize for PCR was not without controversy. Some scientists at Cetus argued that the invention was a collective effort. They felt that colleagues who helped refine and prove the method's utility were not adequately recognized.
Mullis, however, was always credited as the sole inventor of the core concept. The Nobel committee's decision affirmed that the initial flash of insight was his alone. The debates highlight the complex nature of attributing credit in collaborative research environments.
Kary Mullis's Controversial Views and Public Persona
Beyond his scientific genius, Kary Mullis was a deeply complex and controversial figure. He held strong, often contrarian, opinions on a range of scientific and social issues. These views frequently placed him in direct opposition to the mainstream scientific consensus.
Mullis was famously outspoken and relished his role as a scientific maverick. His autobiography, Dancing Naked in the Mind Field (1997), openly detailed his unconventional lifestyle and beliefs. This included his experiences with psychedelics, his skepticism of authority, and his rejection of established theories.
His provocative stance made him a polarizing character. While revered for PCR, he was often criticized for promoting ideas considered fringe or dangerous by the majority of his peers. This duality defines his legacy as both a brilliant innovator and a contentious voice.
Denial of the HIV-AIDS Link
One of Mullis's most prominent and damaging controversies was his rejection of the established fact that HIV causes AIDS. He became a vocal adherent of the fringe movement that denied this link, a position thoroughly debunked by decades of overwhelming scientific evidence.
Mullis argued that the correlation between HIV and AIDS was not sufficient proof of causation. His background in chemistry led him to demand what he considered a higher standard of proof, which he felt was lacking. This stance alarmed and frustrated the global public health community.
- His position was used by denialist groups to lend false credibility to their claims.
- Public health experts warned that his statements could undermine HIV prevention and treatment efforts.
- This controversy significantly tarnished his reputation among many scientists and medical professionals.
Skepticism of Climate Change and the Ozone Hole
Mullis also expressed deep skepticism about human-induced climate change. He questioned the scientific consensus on global warming, often framing it as a form of political dogma rather than evidence-based science. Similarly, he doubted the science behind the anthropogenic causes of the ozone hole.
His criticisms were not based on new climate research but on a general distrust of large scientific institutions and political motives. He positioned himself as a defender of free thought against what he perceived as groupthink. This further isolated him from the mainstream scientific establishment.
The Influence of Psychedelic Experiences
Mullis was remarkably open about his use of lysergic acid diethylamide (LSD) during his graduate studies at Berkeley and beyond. He did not view this as illicit drug use but as a meaningful intellectual and exploratory pursuit.
He directly credited his psychedelic experiences with broadening his consciousness and enhancing his creativity. Mullis claimed that his mind was opened to the non-linear thinking that led to the PCR breakthrough. He described vivid, conceptual visions that helped him visualize complex molecular processes.
"Would I have invented PCR if I hadn't taken LSD? I seriously doubt it," Mullis stated in a 1994 interview.
While this connection is anecdotal, it underscores his belief that unconventional paths could lead to profound scientific discoveries. It remains a fascinating aspect of his unique intellectual journey.
Life After Cetus: Later Career and Entrepreneurial Ventures
After the monumental success of PCR at Cetus, Kary Mullis’s career took several turns. He left the company in the fall of 1986, not long after his method began to gain widespread attention. His departure marked the beginning of a varied and entrepreneurial phase of his professional life.
Mullis briefly served as the Director of Molecular Biology at Xytronyx, Inc. in San Diego in 1986. Following this, he embraced the role of a consultant for multiple corporations. His expertise was sought by major companies including Angenics, Cytometrics, Eastman Kodak, and Abbott Laboratories.
This consultancy work allowed him to apply his unique biochemical insights across different industries. He was not confined to academia or a single corporate lab, preferring the freedom to explore diverse scientific and business challenges.
Founding Altermune and the Quest for Novel Therapies
One of Mullis's significant later ventures was founding a company named Altermune. The name was derived from "altering the immune system." The company's goal was to develop a novel class of therapeutics based on a concept Mullis called chemically programmed immunity.
The Altermune approach aimed to create molecules that could redirect the body’s existing immune defenses to new targets. Mullis envisioned using aptamers (small nucleic acid molecules) to guide antibodies to pathogens or diseased cells. This innovative idea, while scientifically intriguing, never progressed to a widely commercialized therapy.
Altermune represented Mullis's continued drive for disruptive innovation. It showcased his ability to think beyond PCR and tackle complex problems in immunology and drug development, even if the practical outcomes were limited.
The Enduring Legacy of the Polymerase Chain Reaction
The true measure of Kary Mullis’s impact lies in the pervasive, ongoing use of his invention. Decades after its conception, PCR remains a foundational technique in thousands of laboratories worldwide. Its applications have only expanded and diversified over time.
PCR's influence extends far beyond basic research. It has become a critical tool in clinical diagnostics, forensic laboratories, agricultural biotechnology, and environmental monitoring. The method's core principle has spawned numerous advanced variations and next-generation technologies.
- Real-time PCR (qPCR) allows scientists to quantify DNA in real-time, enabling precise measurement of gene expression.
- Reverse Transcription PCR (RT-PCR) converts RNA into DNA, making it essential for studying RNA viruses and gene activity.
- Digital PCR provides absolute quantification of DNA molecules, offering unparalleled sensitivity for detecting rare genetic variants.
PCR's Role in the COVID-19 Pandemic
The global COVID-19 pandemic provided a stark, real-world demonstration of PCR's indispensable value. The standard diagnostic test for detecting SARS-CoV-2 infection was, and remains, a form of RT-PCR. This test amplified viral RNA from patient swabs to detectable levels.
Without PCR technology, mass testing and surveillance during the pandemic would have been scientifically impossible. The ability to process millions of samples rapidly was directly built upon Mullis's 1983 insight. This global event highlighted how a fundamental research tool could become a central pillar of public health infrastructure.
The pandemic underscored that PCR is not just a lab technique but a critical component of modern global health security.
The Commercial and Economic Impact of PCR
The invention of PCR sparked the creation of a multi-billion dollar industry. Companies specializing in thermal cyclers, reagents, enzymes, and diagnostic kits grew rapidly. The technique created vast economic value in the biotechnology and pharmaceutical sectors.
Cetus Corporation, where Mullis worked, eventually sold the PCR patent portfolio to Hoffmann-La Roche for $300 million in 1991. This landmark deal highlighted the immense commercial potential of the technology. Today, the global PCR market continues to expand, driven by advancements in personalized medicine and point-of-care testing.
Kary Mullis: A Complicated Legacy in Science
Kary Mullis's legacy is a study in contrasts. He is universally hailed as the brilliant inventor of one of history's most important scientific methods. Yet, he is also remembered as a controversial figure who publicly rejected well-established science on issues like HIV and climate change.
This duality makes him a fascinating subject for historians of science. It raises questions about the relationship between scientific genius and scientific consensus. Mullis proved that a single individual with a transformative idea could change the world, yet he also demonstrated that expertise in one field does not confer authority in all others.
A Polarizing Figure Remembered
In the scientific community, discussions about Mullis often separate his unequivocal contribution from his controversial personal views. Most scientists celebrate PCR while distancing themselves from his denialist stances. His death in 2019 prompted reflections on this complex legacy.
Obituaries in major publications grappled with how to honor the inventor while acknowledging the provocateur. They credited his monumental achievement but did not shy away from detailing his fringe beliefs. This balanced remembrance reflects the nuanced reality of his life and career.
The Future Built on PCR Technology
The future of biotechnology and medicine is deeply intertwined with the ongoing evolution of PCR. Next-generation sequencing, the cornerstone of genomic medicine
Point-of-care and portable PCR devices are bringing DNA analysis out of central labs and into field clinics, airports, and even homes. The drive for faster, cheaper, and more accessible nucleic acid testing ensures that Mullis’s invention will remain at the forefront of scientific and medical progress for decades to come.
New applications continue to emerge in areas like liquid biopsy for cancer detection, non-invasive prenatal testing, and monitoring of infectious disease outbreaks. The core principle of amplifying specific DNA sequences remains as powerful and relevant today as it was in 1983.
Awards and Honors Beyond the Nobel Prize
While the Nobel Prize was his most famous honor, Kary Mullis received numerous other accolades for his work on PCR. These awards recognized the transformative power of his invention across different domains.
- He received the Japan Prize in 1993, the same year as his Nobel.
- He was awarded the R&D Scientist of the Year award in 1991.
- Mullis also received the National Biotechnology Award and the Gairdner Foundation International Award.
- He was inducted into the National Inventors Hall of Fame in 1997.
Conclusion: The Eccentric Genius Who Changed the World
Kary Mullis's story is one of unconventional brilliance. From his detour into fiction writing and bakery work to his psychedelic-inspired eureka moment on a California highway, his path was anything but ordinary. Yet, his singular idea, the polymerase chain reaction, created a before-and-after moment in the history of biology.
PCR democratized access to the genetic code. It turned DNA from a molecule that was difficult to study in detail into one that could be copied, analyzed, and manipulated with ease. The technique accelerated the pace of biological discovery at a rate few inventions ever have.
The legacy of Kary Mullis is thus permanently etched into the fabric of modern science. Every time a pathogen is identified, a genetic disease is diagnosed, a criminal is caught through DNA evidence, or a new gene is sequenced, his invention is at work. The undeniable utility and omnipresence of PCR secure his place as one of the most influential scientists of the modern era, regardless of the controversies that surrounded him.
In the end, Kary Mullis exemplified how a simple, elegant concept can have an exponentially greater impact than its originator might ever imagine. His life reminds us that scientific progress can spring from the most unexpected minds and moments, forever altering our understanding of life itself.
In conclusion, Kary Mullis's invention of PCR revolutionized molecular biology, leaving an indelible mark on science despite his unconventional life and views. His legacy compels us to consider how profound innovation can arise from the most unexpected individuals. Reflect on how a single idea can amplify its impact across countless fields, from medicine to forensics.


Uterine Peristalsis: Mechanisms, Hormonal Control, and Clinical Implications
Introduction to Uterine Peristalsis
Uterine peristalsis refers to the wave-like contractions of the subendometrial myometrium, the inner muscular layer of the uterus. These contractions play a crucial role in reproductive health, particularly during the follicular phase of the menstrual cycle. Controlled primarily by estradiol and influenced by oxytocin, peristalsis facilitates sperm transport and may aid in embryo implantation.
Research, including a foundational 1998 study cited 161 times, highlights the importance of these contractions in fertility and assisted reproductive technologies (ART). Understanding the mechanisms behind uterine peristalsis can improve clinical outcomes in treatments like in vitro fertilization (IVF).
Hormonal Regulation of Uterine Peristalsis
Role of Estradiol in Peristaltic Activity
The dominant follicle releases estradiol, which drives the frequency of uterine contractions. During the follicular phase, estradiol levels rise, peaking just before ovulation. This hormonal surge enhances peristaltic waves, ensuring optimal conditions for gamete transport.
Studies show that exogenous estradiol, such as estradiol valerate, mimics natural peristaltic patterns. However, high doses do not significantly increase contraction frequency due to system refractoriness.
Influence of Oxytocin on Uterine Contractions
Oxytocin acts locally within the endometrial-subendometrial unit, enhancing the effects of estradiol. Unlike systemic oxytocin, which has limited impact, autocrine/paracrine oxytocin plays a key role in modulating peristalsis.
Clinical trials with intravenous oxytocin in the late follicular phase showed minimal additional effects, suggesting that oxytocin's role is supportive rather than primary.
Pharmacological Insights and Clinical Observations
Impact of Clomiphene Citrate on Peristalsis
Clomiphene citrate, a common fertility drug, slightly suppresses peristaltic frequency despite elevating estradiol levels. This paradoxical effect underscores the complexity of hormonal interactions in uterine contractions.
Research indicates that while clomiphene increases estradiol, it does not proportionally enhance peristalsis, likely due to receptor downregulation or other compensatory mechanisms.
Effects of Exogenous Hormones on Uterine Contractions
Administration of human menopausal gonadotropin (hMG) or estradiol valerate closely replicates natural peristaltic patterns. These findings are critical for fertility treatments, where timing and hormonal balance are essential.
Key observations include:
- Natural cycles show a baseline increase in peristalsis, peaking preovulatorily.
- Estradiol valerate/hMG interventions match natural contraction frequencies.
- High estradiol doses do not exceed normal peristaltic peaks, indicating refractoriness.
Physiological Role of Uterine Peristalsis
Directed Peristaltic Waves vs. Luteal-Phase Dysperistalsis
During the follicular phase, peristaltic waves are directed, facilitating rapid transport of sperm and embryos toward the fundus. In contrast, the luteal phase exhibits dysperistalsis—retrograde contractions that may contribute to conditions like endometriosis.
This distinction is vital for diagnosing and treating reproductive disorders, as abnormal peristalsis can impair fertility.
Study Design and Key Findings
Researchers used vaginal sonography to track peristalsis across different phases of the menstrual cycle. The study confirmed that estradiol is the primary driver of contractions, with oxytocin playing a secondary, synergistic role.
Key findings include:
"Peristaltic contractions in the subendometrial myometrium are critical for reproductive success, with estradiol and oxytocin working in tandem to optimize uterine function."
Clinical Relevance and Therapeutic Implications
Applications in Fertility Treatments
Understanding uterine peristalsis is crucial for IVF protocols. Timing embryo transfer with peak peristaltic activity can improve implantation rates. Clinicians must consider hormonal balance to avoid refractoriness in superovulation treatments.
For example:
- IVF timing: Aligning embryo transfer with natural peristaltic peaks enhances success.
- Avoiding high estradiol doses: Prevents system refractoriness and suboptimal contractions.
Research Gaps and Future Directions
While the 1998 study remains foundational, gaps exist in understanding long-term impacts and molecular pathways. Modern imaging techniques and AI-driven analysis could provide real-time insights into peristaltic activity.
Future research should explore:
- Oxytocin receptor dynamics in the endometrial-subendometrial unit.
- Non-invasive monitoring techniques for clinical applications.
- Long-term effects of hormonal interventions on uterine function.
Conclusion of Part 1
This section has introduced the mechanisms, hormonal regulation, and clinical implications of uterine peristalsis. In Part 2, we will delve deeper into diagnostic techniques, therapeutic strategies, and emerging research trends.
Diagnostic Techniques for Assessing Uterine Peristalsis
Vaginal Sonography: The Gold Standard
Vaginal sonography remains the most reliable method for visualizing uterine peristalsis. This non-invasive technique allows clinicians to observe subendometrial contractions in real-time, providing critical insights into reproductive health.
Key advantages of vaginal sonography include:
- High-resolution imaging of the endometrial-subendometrial unit.
- Real-time monitoring of peristaltic waves during different menstrual phases.
- Minimal discomfort for patients, making it ideal for repeated assessments.
Emerging Technologies in Peristalsis Monitoring
Advancements in medical imaging and artificial intelligence (AI) are revolutionizing the study of uterine peristalsis. 3D ultrasound and MRI offer deeper insights into contraction patterns, while AI algorithms can analyze large datasets to predict optimal fertility windows.
Potential future developments include:
- Automated peristalsis tracking via machine learning.
- Portable ultrasound devices for at-home monitoring.
- Integrated hormone-peristalsis mapping for personalized fertility plans.
Therapeutic Strategies for Optimizing Uterine Peristalsis
Hormonal Interventions in Fertility Treatments
Hormonal therapies play a pivotal role in regulating uterine peristalsis, particularly in assisted reproductive technologies (ART). Clinicians often use estradiol supplements to mimic natural cycles, while oxytocin modulators may enhance contraction efficiency.
Common hormonal interventions include:
- Estradiol valerate to simulate follicular phase conditions.
- Human menopausal gonadotropin (hMG) for controlled ovarian stimulation.
- Clomiphene citrate (with caution due to its suppressive effects on peristalsis).
Timing Embryo Transfer with Peristaltic Peaks
In IVF procedures, synchronizing embryo transfer with peak peristaltic activity can significantly improve implantation rates. Studies suggest that transfers performed during the late follicular phase—when contractions are most robust—yield better outcomes.
Key considerations for timing include:
- Monitoring estradiol levels to predict peristaltic peaks.
- Avoiding luteal phase dysperistalsis, which may hinder embryo movement.
- Personalizing protocols based on individual peristaltic patterns.
Uterine Peristalsis and Reproductive Disorders
Link Between Dysperistalsis and Endometriosis
Endometriosis is closely associated with luteal-phase dysperistalsis, where retrograde contractions may contribute to the displacement of endometrial tissue. Research indicates that women with endometriosis exhibit abnormal peristaltic patterns, which could serve as a diagnostic marker.
Clinical observations include:
- Increased retrograde contractions during the luteal phase.
- Reduced directed peristalsis in the follicular phase.
- Correlation with pelvic pain and infertility.
Impact on Unexplained Infertility
In cases of unexplained infertility, abnormal uterine peristalsis may be a contributing factor. Women with suboptimal contraction patterns often struggle with sperm transport and embryo implantation, even when other fertility parameters appear normal.
Potential solutions include:
- Peristalsis-enhancing therapies (e.g., low-dose oxytocin).
- Targeted hormonal adjustments to restore natural contraction rhythms.
- Advanced imaging to identify subtle peristaltic dysfunctions.
Research Gaps and Future Directions
Molecular Pathways and Oxytocin Receptor Dynamics
While the 1998 study established the role of estradiol and oxytocin, molecular mechanisms remain poorly understood. Future research should explore:
- Oxytocin receptor expression in the endometrial-subendometrial unit.
- Signal transduction pathways governing peristaltic contractions.
- Genetic factors influencing individual peristaltic patterns.
Long-Term Effects of Hormonal Interventions
Most studies focus on short-term peristaltic responses to hormonal treatments. However, long-term effects—such as receptor downregulation or uterine fatigue—require further investigation. Clinicians must balance immediate fertility goals with potential long-term risks.
Key questions include:
- Does prolonged estradiol exposure alter peristaltic efficiency?
- Can repeated oxytocin use lead to desensitization?
- Are there cumulative effects of fertility drugs on uterine function?
Conclusion of Part 2
This section has explored diagnostic techniques, therapeutic strategies, and the link between uterine peristalsis and reproductive disorders. In Part 3, we will conclude with a summary of key takeaways, practical recommendations, and the future of peristalsis research.
Key Takeaways and Practical Recommendations
Summarizing the Role of Uterine Peristalsis in Fertility
Uterine peristalsis is a critical yet often overlooked factor in reproductive health. Driven by estradiol and modulated by oxytocin, these contractions facilitate sperm transport and embryo implantation. Understanding their mechanisms can significantly improve fertility treatments and diagnostic approaches.
Key insights include:
- Estradiol dominance in the follicular phase enhances peristaltic frequency.
- Oxytocin’s local action supports but does not override estradiol’s effects.
- Dysperistalsis in the luteal phase may contribute to conditions like endometriosis.
Clinical Recommendations for Fertility Specialists
For clinicians, optimizing uterine peristalsis involves a combination of hormonal balance, timing strategies, and advanced monitoring. Practical steps include:
- Monitoring estradiol levels to predict peak peristaltic activity.
- Avoiding excessive clomiphene citrate, which may suppress contractions.
- Using vaginal sonography to assess peristaltic patterns before IVF.
- Personalizing embryo transfer timing based on individual peristaltic rhythms.
Future Research and Technological Advancements
Potential Breakthroughs in Peristalsis Research
While the 1998 study remains foundational, modern research must address unanswered questions. Future directions include:
- Molecular studies on oxytocin receptor dynamics.
- AI-driven peristalsis tracking for real-time fertility predictions.
- Long-term effects of hormonal interventions on uterine function.
Emerging technologies like 3D ultrasound and machine learning could revolutionize how we diagnose and treat peristaltic dysfunctions.
The Role of AI and Machine Learning
Artificial intelligence is poised to transform fertility research by analyzing vast datasets to identify patterns in uterine contractions. Potential applications include:
- Automated peristalsis analysis from ultrasound scans.
- Predictive modeling for optimal embryo transfer timing.
- Personalized treatment plans based on individual peristaltic profiles.
"The integration of AI into reproductive medicine could unlock new possibilities for diagnosing and treating infertility linked to uterine peristalsis."
Addressing Common Misconceptions
Myth: Higher Estradiol Levels Always Improve Fertility
A common misconception is that maximizing estradiol will always enhance fertility. However, research shows that excessive estradiol can lead to system refractoriness, where the uterus no longer responds optimally to hormonal signals.
Key clarifications:
- Optimal estradiol levels vary by individual.
- High doses may not improve peristalsis beyond natural peaks.
- Balanced hormonal protocols yield better results than aggressive stimulation.
Myth: Oxytocin Is the Primary Driver of Peristalsis
While oxytocin plays a supportive role, it is not the primary regulator of uterine contractions. Estradiol remains the dominant hormone, with oxytocin acting as a modulator rather than a driver.
Important distinctions:
- Oxytocin enhances but does not initiate peristalsis.
- Local oxytocin action (autocrine/paracrine) is more critical than systemic administration.
- Excessive oxytocin does not significantly increase contraction frequency.
Conclusion: The Future of Uterine Peristalsis Research
Uterine peristalsis is a dynamic and essential component of female reproductive health. From its hormonal regulation to its clinical implications, understanding these contractions can lead to better fertility outcomes and more effective treatments for conditions like endometriosis and unexplained infertility.
As research advances, integrating AI, modern imaging, and personalized medicine will further illuminate the complexities of uterine function. Clinicians and researchers must continue collaborating to translate these insights into practical, patient-centered solutions.
"The study of uterine peristalsis is not just about contractions—it’s about unlocking the potential for healthier pregnancies and more successful fertility treatments."
By staying informed and embracing innovation, the medical community can ensure that uterine peristalsis remains a cornerstone of reproductive endocrinology and assisted reproductive technologies.
एक्यूट एन्सेफेलाइटिस सिंड्रोम (AES): कारण, लक्षण और बचाव
एक्यूट एन्सेफेलाइटिस सिंड्रोम (AES) एक गंभीर न्यूरोलॉजिकल विकार है जो मुख्य रूप से बच्चों को प्रभावित करता है। इसमें मस्तिष्क में सूजन हो जाती है जिसके कारण तेज बुखार, दौरे और चेतना में कमी जैसे लक्षण दिखाई देते हैं। भारत के कई राज्यों में यह एक चुनौतीपूर्ण सार्वजनिक स्वास्थ्य समस्या बना हुआ है।
AES क्या है? समझें इसकी मूल परिभाषा
एक्यूट एन्सेफेलाइटिस सिंड्रोम कोई एक विशेष बीमारी नहीं बल्कि एक लक्षणों का समूह है। यह समूह मस्तिष्क संबंधी गंभीर संक्रमण या अन्य कारणों से उत्पन्न होता है। जब किसी बच्चे में अचानक तेज बुखार के साथ मानसिक भ्रम या बेहोशी जैसे लक्षण दिखें, तो उसे AES का संदेह होता है। इसके पीछे कई कारक जिम्मेदार हो सकते हैं।
AES के प्रमुख कारण और वाहक
जापानी एन्सेफेलाइटिस (JE) वायरस AES का एक प्रमुख ज्ञात कारण है, जो मच्छरों के काटने से फैलता है। हालांकि, कई AES के मामलों में कोई विशिष्ट वायरस भी पहचान में नहीं आता। अन्य संभावित कारणों में बैक्टीरियल संक्रमण जैसे लेप्टोस्पायरोसिस, स्क्रब टाइफस या फिर विषाक्त पदार्थ शामिल हैं। यह बीमारी अक्सर ग्रामीण क्षेत्रों में सामने आती है जहां स्वच्छता, जल भंडारण और मच्छरों के प्रजनन की अनुकूल परिस्थितियां होती हैं।
विशेषज्ञों का मानना है कि AES के कई मामले कुपोषण और गंदगी से भी प्रत्यक्ष रूप से जुड़े हुए हैं। शुरुआती निदान और उचित चिकित्सा जीवनरक्षक साबित हो सकती है।
भारत में AES का ऐतिहासिक और वर्तमान संदर्भ
भारत में AES का प्रकोप दशकों से एक विकट समस्या रही है। बिहार, उत्तर प्रदेश, असम और पश्चिम बंगाल जैसे राज्य इससे सबसे अधिक प्रभावित रहे हैं। वर्ष 2005 में मुजफ्फरपुर, बिहार में आए भयावह प्रकोप ने इस बीमारी को वैश्विक स्तर पर चर्चा में ला दिया था।
उस समय सैकड़ों बच्चों की मृत्यु ने स्वास्थ्य व्यवस्था पर गंभीर सवाल खड़े कर दिए थे। तब से लेकर आज तक सरकारी और गैर-सरकारी स्तर पर इसके नियंत्रण और रोकथाम के प्रयास जारी हैं। फिर भी, हर साल मानसून के मौसम में नए मामले सामने आ जाते हैं।
AES से जुड़े प्रमुख जोखिम कारक
कुछ विशेष परिस्थितियां AES के खतरे को कई गुना बढ़ा देती हैं। इनमें निम्नलिखित प्रमुख हैं:
- आयु: पांच साल से कम उम्र के बच्चे, विशेषकर शिशु, सबसे अधिक संवेदनशील होते हैं।
- कुपोषण: कम वजन और कमजोर प्रतिरक्षा प्रणाली वाले बच्चों में जोखिम अधिक होता है।
- स्वच्छता की कमी: खुले में शौच, गंदा पानी और मच्छरों का प्रजनन जोखिम बढ़ाते हैं।
- निवास स्थान: ग्रामीण, दूर-दराज के इलाके जहां चिकित्सा सुविधाएं सीमित हैं।
AES के लक्षणों को कैसे पहचानें?
AES के लक्षण अचानक और बहुत तेजी से उभरते हैं। प्रारंभिक अवस्था में इसे सामान्य बुखार समझने की भूल हो सकती है। इसलिए सतर्कता बेहद जरूरी है। मुख्य लक्षणों में शामिल हैं:
- तेज बुखार: शरीर का तापमान अचानक बहुत अधिक बढ़ जाना।
- दौरे पड़ना: शरीर में ऐंठन या बार-बार झटके आना।
- चेतना में कमी: सुस्ती, भ्रम की स्थिति, बेहोशी या कोमा में चले जाना।
- सिरदर्द और उल्टी: तेज सिरदर्द के साथ बार-बार उल्टी आना।
- गर्दन अकड़ना: बच्चे की गर्दन ढीली न पड़ना या अकड़न महसूस होना।
इनमें से कोई भी लक्षण दिखाई देने पर तुरंत नजदीकी अस्पताल में तत्काल चिकित्सकीय सहायता लेनी चाहिए। समय पर उपचार जान बचाने में निर्णायक भूमिका निभाता है।
AES के निदान और प्रबंधन की प्रक्रिया
AES के संदिग्ध मामले में डॉक्टर कई प्रकार के परीक्षण करते हैं। इनका उद्देश्य बीमारी के सटीक कारण का पता लगाकर उचित इलाज शुरू करना है। निदान में निम्नलिखित शामिल हो सकते हैं:
- रक्त और मूत्र परीक्षण: संक्रमण या अन्य असामान्यताओं की जांच के लिए।
- सेरेब्रोस्पाइनल फ्लूइड (CSF) विश्लेषण: रीढ़ की हड्डी से द्रव लेकर मस्तिष्क की सूजन की जांच।
- इमेजिंग: सीटी स्कैन या एमआरआई के जरिए मस्तिष्क की स्थिति देखना।
- ईईजी (इलेक्ट्रोएन्सेफलोग्राम): मस्तिष्क की विद्युत गतिविधि का अध्ययन।
उपचार के मुख्य आधार
AES का उपचार मुख्य रूप से सहायक चिकित्सा पर निर्भर करता है, क्योंकि अधिकांश वायरल संक्रमणों की कोई विशिष्ट दवा नहीं होती। उपचार का लक्ष्य रोगी के लक्षणों को नियंत्रित करना और जीवन को स्थिर रखना होता है।
इसमें बुखार कम करने की दवाएं, दौरे रोकने के लिए एंटी-कनवल्सेंट, द्रव चढ़ाना और सांस लेने में मदद करना शामिल है। यदि कारण बैक्टीरिया है तो एंटीबायोटिक दवाओं का उपयोग किया जाता है। रोगी को आईसीयू में रखकर लगातार निगरानी की आवश्यकता होती है।
AES से बचाव के उपाय और सरकारी पहल
एक्यूट एन्सेफलाइटिस सिंड्रोम की रोकथाम बेहद आवश्यक है क्योंकि इसका उपचार अक्सर जटिल होता है। सरकार ने इस दिशा में कई महत्वपूर्ण कदम उठााए हैं, जिनमें जापानी एन्सेफलााइटिस (JE) के टीकाकरण को प्रमुखता दी गई है। इसके अलावा, स्वच्छता अभियान और जागरूकता कार्यक्रम चलााए जा रहे हैं।
टीकाकरण: सबसे प्रभावी सुरक्षा कवच
जापानी एन्सेफलााइटिस का टीका AES को रोकने में एक मील का पत्थर साबित हुआ है। यह टीका सरकारी स्वास्थ्य केंद्रों पर निःशुल्क लगाया जाता है और इसे बच्चों के टीकाकरण कार्यक्रम में शामिल किया गया है। टीके की खास बात यह है कि यह दीर्र्घकालिक सुरक्षा प्रदान करता है।
- टीकाकरण अनुसूची: पहला टीका 9 महीने की आयु में और बूस्टर डोज 16-24 महीने में।
- उच्च जोखिम वाले क्षेत्र: बििहार, उत्तर प्रदेश, असम आदि राज्यों में वि विशेष अभियान।
- दुष्प्रभाव: सामान्यतः हल्का बुखार या इंजेक्शन वाली जगह पर दर्र्द।
विश्व स्वास्थ्य संगठन (WHO) के अनुसार, JE टीकाकरण से प्रभावित क्षेत्रों में इस बीमारी के मामलों में 70-80% तक की कमी देखी गई है। यह आँकड़ा टीके की प्रभावशीलता को सााबित करता है।
सामुदायिक स्तर पर रोकथाम के उपाय
AES के प्रसार को रोकने के लिए सामुदायिक भागीदारी अत्यंत महत्वपूर्ण है। स्थानीय निवासी ही सबसे पहले खतरे के संकेतों को पहचान सकते हैं। मच्छरों के प्रजनन को रोकना इसका एक प्रमुख हिस्सा है।
निम्नलििखित उपायों को अपनाकर जोखिम को कााफी हद तक कम किया जा सकता है:
- मच्छरदानी का उपयोग: विशेषकर बच्चों और गर्भवती महिलाओं के लिए अनिवार्य।
- सााफ-सफाई: खुले में पानी जमा न होने देना और कीटनाशकों का छिड़काव।
- शीघ्र निदान: बुखार आने पर तुरंत स्वास्थ्य कार्यकर्ता को सूचित करना।
- जल प्रबंधन: साफ पीने का पानी उपलब्ध कराना और हैण्डपम्पों के आस-पास सूखा रखना।
AES के दीर्र्घकालिक प्रभाव और पुनर्वास
जो बच्चे AES के गंभीर मामले से उबरते हैं, उन्हें अक्सर दीर्घकालिक स्वास्थ्य समस्यााओं का सामना करना पड़ सकता है। मस्तिष्क में हुई क्षति के कारण शारीरिक और मानसिक विकास प्रभावित होता है। ऐसे में समय पर पुनर्वास सेवााएं जीवन की गुणवत्ता में सुधार ला सकती हैं।
सामान्य दीर्र्घकालिक प्रभाव
AES से ठीक होने वाले बच्चों में देखे जाने वाले कुछ प्रमुख दीर्घकालिक प्रभाव निम्नलििखित हैं:
- संज्ञानात्मक अक्षमताएं: याददाश्त कमजोर होना, सीखने की गति धीमी होना।
- मोटर कौशल में कमी: चलने-फिरने या हााथों के समन्वय में समस्या।
- मिरगी के दौरे: AES के बाद मिरगी की बीमारी होने का खतरा बढ़ जाता है।
- मानसिक स्वास्थ्य समस्यााएं: व्यवहार में बदलाव, चिंता या अवसाद।
पुनर्वास की प्रक्रिया और महत्व
पुनर्वास एक सतत प्रक्रिया है जिसमें डॉक्टर, फिजियोथेरेपिस्ट, व्यावसायिक चिकित्सक और परिवार सभी की महत्वपूर्ण भूमिका होती है। इसका लक्ष्य बच्चे को स्वावलंबी बनाना और उसे सामान्य जीवन में वापस लाना होता है। पुनर्वास में शामिल हैं:
- फिजियोथेरेपी: मांसपेशियों की ताकत और चलने-फिरने की क्षमता को वापस लाना।
- व्यावसायिक चिकित्सा: दैनिक गतिविधियों जैसे खाना, कपड़े पहनना सििखाना।
- बोलचाल की थेरेपी: अगर बोलने या नििगलने में कोई समस्या हो।
- विशेष शिक्षा: सीखने की अक्षमता को दूर करने के लिए वि विशेषज्ञों की मदद।
अध्ययन बताते हैं कि शीघ्र और नियमित पुनर्वास से लगभग 60% बच्चों में कार्यात्मक क्षमता में बहुत सुधार देखा गया है। परिवार का सहयोग इसकी सफलता की कुंजी है।
AES पर वर्तमान शोध और भविष्य की दिशााएं
वैज्ञानिक लगातार AES के कारणों, निदान और उपचार के बेहतर तरीकों पर शोध कर रहे हैं। तकनीकी उन्नति ने इस क्षेत्र में नई संभावनाएं खोली हैं। डििजििटल नििगरानी प्रणाली और त्वरित नैदानिक किटों पर काम चल रहा है।
नैदानिक क्षमतााओं में सुधार
पारंपरिक लैब टेस्टों में समय लगता है, जबकि AES के मामले में शीघ्र निदान जीवनरक्षक होता है। इस चुनौती से निपटने के लिए पॉइंट-ऑफ-केयर टेस्टिंग डिवाइस विकसित की जा रही हैं। ये डिवाइस गांव के स्वास्थ्य केंद्रों पर भी तुरंत परििणाम दे सकती हैं।
- मल्टीप्लेक्स PCR टेस्ट: एक ही नमूने में कई वायरसों की पहचान करना।
- सीरोलॉजी बेस्ड रैपिड टेस्ट: रक्त में एंटीबॉडी की जांच करना।
- नेक्स्ट-जनरेशन सीक्वेंसिंग: नए और अज्ञात रोगजनकों की पहचान करना।
डििजििटल निगरानी और डेटा एनालिटिक्स
आज के दौर में डििजििटल हेल्थ टूल्स का उपयोग करके AES के प्रकोपों की भविष्यवाणी की कोशिश की जा रही है। मौसम के डेटा, मच्छरों की आबादी और ऐतिहासिक रुुझानों को मिलाकर अर्ली वार्निंग सिस्टम विकसित किए जा रहे हैं।
इन प्रणालियों के लाभ स्पष्ट हैं:
- समय पर चेतावनी: स्वास्थ्यकर्मी प्रकोप से पहले ही तैयारी कर सकते हैं।
- संसाधनों का कुशल आवंटन: टीके और दवााएं उचित स्थानों पर पहुुँचाई जा सकती हैं।
- नीति निर्माण में मदद: वास्तविक समय के डेटा से बेहतर नीतियां बन सकती हैं।
इस प्रकार, शोध और तकनीक AES की रोकथाम और नियंत्रण की लड़ाई में नए हथियार प्रदान कर रहे हैं। सही दिशा में किए गए प्रयास भविष्य में इस बीमारी को हराने की उम्मीद जगाते हैं।
एक्यूट एन्सेफेलाइटिस सिंड्रोम (AES) और पोषण का गहरा संबंध
कई अध्ययनों ने यह स्पष्ट किया है कि AES और कुपोषण के बीच एक मजबूत संबंध है। जिन बच्चों का शारीरिक और मानसिक विकास उचित पोषण के अभाव में अवरुद्ध हो जाता है, वे AES जैसी संक्रामक बीमारियों के प्रति अधिक संवेदनशील होते हैं। यह एक चक्र बनाता है जहां कुपोषण बीमारी का कारण भी बन सकता है और परिणाम भी।
लाइची और AES: मिथक व तथ्य
बिहार के मुजफ्फरपुर जैसे क्षेत्रों में, अतीत में AES के प्रकोप को कच्ची लाइची के सेवन से जोड़कर देखा गया था। शोध बताते हैं कि कुपोषित बच्चों द्वारा खाली पेट अधिक मात्रा में लाइची खाने से हाइपोग्लाइसीमिक एन्सेफेलोपैथी हो सकती है। हालांकि, यह AES का एकमात्र या प्रमुख कारण नहीं है।
वास्तविकता यह है कि AES के अधिकांश मामले JE वायरस या अन्य संक्रमणों से जुड़े हैं। लाइची को लेकर सतर्कता जरूरी है, परंतु ध्यान मच्छर नियंत्रण, स्वच्छता और टीकाकरण जैसे प्रमुख उपायों पर केंद्रित होना चाहिए।
विशेषज्ञों का मत है कि संतुलित भोजन और रात में खाना खाकर सोना बच्चों को न केवल लाइची से होने वाले जोखिम से, बल्कि सामान्य रूप से कुपोषण से भी बचा सकता है।
AES के प्रबंधन में स्वास्थ्य प्रणाली की भूमिका
AES जैसी जटिल बीमारी से लड़ने के लिए एक मजबूत और तैयार स्वास्थ्य प्रणाली का होना अनिवार्य है। इसमें प्राथमिक स्वास्थ्य केंद्रों से लेकर जिला अस्पतालों तक, सभी स्तरों पर विशेष प्रशिक्षण और संसाधनों की आवश्यकता होती है। स्वास्थ्य कर्मियों का समय पर प्रशिक्षण, निदान किटों की उपलब्धता और आपातकालीन प्रतिक्रिया प्रणाली महत्वपूर्ण हैं।
राष्ट्रीय एवं राज्य स्तर पर कार्यक्रम
भारत सरकार ने AES के नियंत्रण के लिए कई राष्ट्रीय कार्यक्रम चलाए हैं। राष्ट्रीय वेक्टर जनित रोग नियंत्रण कार्यक्रम (NVBDCP) इसका एक प्रमुख हिस्सा है। इसके तहत निम्नलिखित गतिविधियाँ शामिल हैं:
- जन-जागरूकता अभियान: ग्रामीण क्षेत्रों में AES के लक्षण और बचाव के उपाय बताना।
- स्वास्थ्य कर्मियों का प्रशिक्षण: प्रारंभिक निदान और प्रबंधन पर विशेष फोकस।
- निगरानी तंत्र को मजबूत करना: HMIS (स्वास्थ्य प्रबंधन सूचना प्रणाली) के माध्यम से मामलों की ट्रैकिंग।
- अंतर-मंत्रालयी समन्वय: स्वास्थ्य, जल शक्ति और स्वच्छता विभागों का संयुक्त प्रयास।
AES से निपटने में सामुदायिक जागरूकता का महत्व
किसी भी बीमारी को हराने में सामुदायिक भागीदारी सबसे बड़ा हथियार साबित होती है। AES के मामले में, गाँव के निवासी, आंगनवाड़ी कार्यकर्ता और ASHA (अक्रांतित सामाजिक स्वास्थ्य कार्यकर्ता) सैनिकों की भूमिका निभाते हैं। इनके माध्यम से सही जानकारी तेजी से फैलाई जा सकती है।
जागरूकता के प्रमुख बिंदु
सामुदायिक स्तर पर फैलाई जाने वाली जानकारी में निम्नलिखित बातें शामिल होनी चाहिए:
- तत्काल कार्रवाई: बच्चे में AES के शुरुआती लक्षण दिखते ही तुरंत अस्पताल ले जाना।
- टीकाकरण का महत्व: JE का टीका समय पर लगवाने की आवश्यकता को समझाना।
- स्वच्छता के उपाय: मच्छरों से बचाव, साफ पानी और शौचालय के उपयोग के तरीके।
- पोषण: बच्चों को पौष्टिक आहार देने और रात को खाली पेट न सोने देने की सलाह।
यह अनुमान लगाया गया है कि सामुदायिक जागरूकता और सहभागिता से AES के मामलों में 40% तक की कमी लाई जा सकती है। शिक्षा ही सबसे प्रभावी दवा है।
निष्कर्ष: AES एक रोकथाम योग्य चुनौती
एक्यूट एन्सेफेलाइटिस सिंड्रोम (AES) एक गंभीर स्वास्थ्य समस्या है, लेकिन यह पूरी तरह रोकथाम योग्य भी है। पिछले कुछ वर्षों में JE टीकाकरण अभियानों और जागरूकता कार्यक्रमों के सकारात्मक परिणाम सामने आए हैं। हालांकि, अभी भी चुनौतियाँ बनी हुई हैं।
इन चुनौतियों का सामना करने के लिए एक बहु-स्तरीय रणनीति अपनाने की आवश्यकता है। इस रणनीति के मुख्य स्तंभ हैं:
- सार्वभौमिक टीकाकरण: हर बच्चे तक JE का टीका पहुँचाना सुनिश्चित करना।
- स्वास्थ्य अवसंरचना को मजबूत करना: ग्रामीण अस्पतालों में आईसीयू सुविधाओं का विस्तार।
- त्वरित निदान: उन्नत और तेज़ डायग्नोस्टिक किट्स को प्राथमिक स्वास्थ्य केंद्रों तक ले जाना।
- सामुदायिक सशक्तिकरण: लोगों को ज्ञान से लैस करना ताकि वे अपने बच्चों की रक्षा स्वयं कर सकें।
अंतिम संदेश और भविष्य की आशा
AES के खिलाफ लड़ाई केवल चिकित्सा क्षेत्र तक सीमित नहीं है। यह एक सामाजिक, आर्थिक और पर्यावरणीय चुनौती है जिसका समाधान समग्र दृष्टिकोण से ही संभव है। स्वच्छ पानी की आपूर्ति, बेहतर स्वच्छता, पोषण सुरक्षा और शिक्षा जैसे कारक भी इसमें महत्वपूर्ण भूमिका निभाते हैं।
हमारा ध्यान न केवल बीमारी का इलाज करने पर, बल्कि उसे होने से रोकने पर केंद्रित होना चाहिए। हर बच्चा सुरक्षित और स्वस्थ बचपन जीने का हकदार है। सरकार, स्वास्थ्य कर्मी, शोधकर्ता और समुदाय मिलकर काम करें, तो AES जैसी बीमारी को हराया जा सकता है। आइए, हम सब मिलकर एक ऐसे भविष्य की ओर कदम बढ़ाएं जहाँ AES का नाम मात्र एक स्मृति बनकर रह जाए।
सचेत रहें, सुरक्षित रहें। अपने बच्चों का टीकाकरण ज़रूर कराएं और किसी भी गंभीर लक्षण पर तुरंत चिकित्सकीय सलाह लें। सही जानकारी और सामूहिक प्रयास ही इस लड़ाई में हमारी सबसे बड़ी ताकत है।
Felix d Herelle: Pioneer of Bacteriophages
The story of Félix d'Hérelle is one of unconventional genius. Born in Montreal in 1873, this French-Canadian microbiologist revolutionized science with a discovery that would shape modern medicine and molecular biology. Félix d'Hérelle is celebrated as the co-discoverer of bacteriophages, the viruses that infect bacteria. Despite having only a high school education, his pioneering work in phage therapy and biological pest control cemented his legacy.
His journey from self-taught scientist to world-renowned researcher is a testament to sharp observation and intellectual daring. D'Hérelle's work laid the foundation for entire fields of study, from virology to genetic engineering.
The Unlikely Path of a Microbiological Genius
Félix d'Hérelle's early life did not predict a future as a scientific luminary. His formal education ended with high school. Yet, an intense curiosity about the natural world drove him to teach himself microbiology. This self-directed learning became the cornerstone of a remarkable career that defied the academic norms of his era.
He began his practical work far from Europe's prestigious institutes. D'Hérelle served as a bacteriologist at the General Hospital in Guatemala City. There, he organized public health defenses against deadly diseases like malaria and yellow fever.
From Sisal to Locusts: A Pivotal Assignment
D'Hérelle's path to discovery took a decisive turn in Mexico. Initially, he was tasked with studying the alcoholic fermentation of sisal residue. This industrial project unexpectedly led him into the world of insect pathology.
While investigating diseases affecting locusts, he made a critical observation. On agar cultures of bacteria infecting the insects, he noticed clear spots where the bacterial lawn had been wiped out. This simple observation sparked the idea of using pathogens to control pests.
Joining the Pasteur Institute and Early Recognition
In 1911, d'Hérelle's growing expertise earned him a position at the famed Pasteur Institute in Paris. He started as an unpaid assistant, yet his talent quickly shone. He gained international attention for his successful campaigns against Mexican locust plagues.
He utilized a bacterium called Coccobacillus to devastate locust populations. This work established him as an innovative thinker in applied microbiology. It also foreshadowed his future title as the "father of biological pest control."
His methods represented a groundbreaking approach to agriculture. They preceded modern biocontrol agents like Bacillus thuringiensis (Bt) by decades. The stage was now set for his most profound contribution to science.
The Groundbreaking Discovery of Bacteriophages
The year 1917 marked a watershed moment in microbiology. On September 10, Félix d'Hérelle published a landmark note in the Comptes rendus de l'Academie des sciences. He described a mysterious "obligate intracellular parasite" of bacteria. This discovery would define his career and alter the course of biological science.
The discovery occurred during World War I. D'Hérelle was investigating a severe dysentery outbreak afflicting a French cavalry squadron. He filtered bacterial cultures from sick soldiers and observed something extraordinary.
The filtrate, even when diluted, could rapidly and completely destroy cultures of dysentery bacteria. D'Hérelle termed the invisible agent a "bacteria-eater," or bacteriophage.
Methodological Brilliance in Virology
D'Hérelle's genius extended beyond the initial observation. He developed a simple yet powerful technique to quantify these invisible entities. He serially diluted suspensions containing the phage and spread them on bacterial lawns.
Instead of uniformly killing the bacteria, the highest dilutions created discrete, clear spots called plaques. D'Hérelle reasoned correctly that each plaque originated from a single viral particle.
- He counted the plaques on the most diluted sample.
- He multiplied that count by the dilution factor.
- This calculation gave him the number of bacteriophage viruses in his original suspension.
This method established the foundational plaque assay, a technique still central to virology today. Between 1918 and 1921, he identified different phages targeting various bacterial species, including the deadly Vibrio cholerae.
A Note on Precedence: Twort vs. d'Hérelle
History notes that British microbiologist F.W. Twort observed a similar phenomenon in 1915. However, Twort was hesitant to pursue or promote his finding. D'Hérelle's systematic investigation, relentless promotion, and coining of the term "bacteriophage" made his work the definitive cornerstone of the field.
His discovery provided the first clear evidence of viruses that could kill bacteria. This opened a new frontier in the battle against infectious disease.
The Dawn of Phage Therapy
Félix d'Hérelle was not content with mere discovery. He immediately envisioned a therapeutic application. He pioneered phage therapy, the use of bacteriophages to treat bacterial infections. His first successful experiment was dramatic.
In early 1919, he isolated phages from chicken feces. He used them to treat a virulent chicken typhus plague, saving the birds. This success in animals gave him the confidence to attempt human treatment.
The first human trial occurred in August 1919. D'Hérelle successfully treated a patient suffering from severe bacterial dysentery using his phage preparations. This milestone proved the concept that viruses could be used as healers.
He consolidated his findings in his 1921 book, Le bactériophage, son rôle dans l'immunité ("The Bacteriophage, Its Role in Immunity"). This work firmly established him as the father of phage therapy. The potential for a natural, self-replicating antibiotic alternative was now a reality.
Global Impact and Controversies of Phage Therapy
The success of d'Hérelle's initial human trial catapulted phage therapy into the global spotlight. Doctors worldwide began experimenting with bacteriophages to combat a range of bacterial infections. This period marked the first major application of virology in clinical medicine.
D'Hérelle collaborated with the pharmaceutical company L'Oréal to produce and distribute phage preparations. Their products targeted dysentery, cholera, and plague, saving countless lives. This commercial partnership demonstrated the immense therapeutic potential he had unlocked.
However, the rapid adoption of phage therapy was not without significant challenges. The scientific understanding of bacteriophage biology was still in its infancy. These inconsistencies led to skeptical reactions from parts of the medical establishment.
The Soviet Union Embraces Phage Research
While Western medicine grew cautious, the Soviet Union enthusiastically adopted d'Hérelle's work. In 1923, he was invited to Tbilisi, Georgia, by microbiologist George Eliava. This collaboration led to the founding of the Eliava Institute of Bacteriophage.
The Institute became a global epicenter for phage therapy research and application. It treated Red Army soldiers during World War II, using phages to prevent gangrene and other battlefield infections. To this day, the institute remains a leading facility for phage therapy.
The partnership between d'Hérelle and Eliava was scientifically fruitful but ended tragically. George Eliava was executed in 1937 during Stalin's Great Purge, a severe blow to their shared vision.
Challenges in the West
In Europe and North America, phage therapy faced a more skeptical reception. Early clinical studies often produced inconsistent results due to several critical factors that were not yet understood.
- Poor Phage Purification: Early preparations often contained bacterial debris, causing adverse reactions in patients.
- Phage Specificity: Doctors did not always match the specific phage to the specific bacterial strain causing the infection.
- Bacterial Resistance: The ability of bacteria to develop resistance to phages was not fully appreciated.
The discovery and mass production of chemical antibiotics like penicillin in the 1940s further sidelined phage therapy in the West. Antibiotics were easier to standardize and had a broader spectrum of activity. For decades, phage therapy became a largely Eastern European practice.
Expanding the Scope: Public Health and Biological Control
Félix d'Hérelle's vision for bacteriophages extended far beyond individual patient treatment. He was a pioneering thinker in the field of public health. He saw phages as a tool for preventing disease on a massive scale.
He conducted large-scale experiments to prove that bacteriophages could be used to sanitize water supplies. By introducing specific phages into wells and reservoirs, he aimed to eliminate waterborne pathogens like cholera. This proactive approach was revolutionary for its time.
Combating Cholera Epidemics
D'Hérelle applied his public health philosophy to combat real-world epidemics. He traveled to India in the late 1920s to fight cholera, a disease that ravaged the population. His work there demonstrated the potential for community-wide prophylaxis.
He administered phage preparations to thousands of individuals in high-risk communities. His efforts showed a significant reduction in cholera incidence among those treated. This large-scale application provided compelling evidence for the power of phage-based prevention.
Despite these successes, logistical challenges and the rise of alternative public health measures limited widespread adoption. Yet, his work remains a landmark in the history of epidemiological intervention.
Return to Biological Pest Control
D'Hérelle never abandoned his early interest in using microbes against insect pests. His discovery of bacteriophages reinforced his belief in biological solutions. He continued to advocate for the use of pathogens to control agricultural threats.
His early success with Coccobacillus against locusts paved the way for modern biocontrol. This approach is now a cornerstone of integrated pest management. It reduces the reliance on chemical pesticides, benefiting the environment.
D'Hérelle is rightly credited as a founding father of this field. His ideas directly anticipated the development and use of Bacillus thuringiensis (Bt), a bacterium used worldwide as a natural insecticide.
Scientific Recognition and Academic Pursuits
Despite his lack of formal academic credentials, Félix d'Hérelle achieved remarkable recognition. His groundbreaking discoveries could not be ignored by the scientific community. He received numerous honors and prestigious appointments.
In 1924, the University of Leiden in the Netherlands appointed him a professor. This was a significant achievement for a self-taught scientist. He also received an honorary doctorate from the University of Leiden, validating his contributions to science.
His work earned him a nomination for the Nobel Prize in Physiology or Medicine. Although he never won, the nomination itself placed him among the most elite researchers of his generation. His legacy was secured by the profound impact of his discoveries.
The Nature of Viruses and Theoretical Contributions
D'Hérelle was not just an experimentalist; he was also a theorist who pondered the fundamental nature of life. He engaged in spirited debates about whether bacteriophages were living organisms or complex enzymes. He passionately argued that they were living viruses.
His theories on immunity were also advanced. He proposed that bacteriophages played a crucial role in natural immunity. He suggested that the body's recovery from bacterial infections was often mediated by the natural activity of these viruses.
- Theory of Natural Immunity: D'Hérelle believed phages in the environment provided a first line of defense.
- Debate on Viral Life: His arguments helped shape the early field of virology.
- Host-Parasite Relationship: He provided a clear model for understanding obligate parasitism.
These theoretical battles were vital for the development of microbiology. They forced the scientific community to confront and define the boundaries of life at the microscopic level.
Later Career and Move to Yale
In 1928, d'Hérelle accepted a position at Yale University in the United States. This move signaled his high standing in American academic circles. At Yale, he continued his research and mentored a new generation of scientists.
His later work focused on refining phage therapy techniques and understanding phage genetics. He continued to publish prolifically, sharing his findings with the world. However, his unwavering and sometimes stubborn adherence to his own theories occasionally led to friction with colleagues.
Despite these interpersonal challenges, his productivity remained high. His time at Yale further cemented the importance of bacteriophage research in American institutions.
Later Years and Scientific Legacy
Félix d'Hérelle remained an active and prolific researcher well into his later years. After his tenure at Yale University, he returned to France, continuing his work with undiminished passion. He maintained a laboratory in Paris, where he pursued his investigations into viruses and their applications.
Despite facing occasional isolation from the mainstream scientific community due to his strong-willed nature, his dedication never wavered. He continued to write and publish, defending his theories and promoting the potential of bacteriophages. His later writings reflected a lifetime of observation and a deep belief in the power of biological solutions.
D'Hérelle passed away in Paris on February 22, 1949, from pancreatic cancer. His death marked the end of a remarkable life dedicated to scientific discovery. He left behind a legacy that would only grow in significance with time.
The Modern Revival of Phage Therapy
For decades after the antibiotic revolution, phage therapy was largely forgotten in the West. However, the late 20th and early 21st centuries have witnessed a dramatic resurgence of interest. The driving force behind this revival is the global crisis of antibiotic resistance.
As multidrug-resistant bacteria like MRSA and CRE have become major public health threats, scientists have returned to d'Hérelle's work. Phage therapy offers a promising alternative or complement to traditional antibiotics. Modern clinical trials are now validating many of his early claims with rigorous scientific methods.
- Personalized Medicine: Phages can be tailored to target specific bacterial strains infecting a patient.
- Fewer Side Effects: Phages are highly specific, reducing damage to the body's beneficial microbiome.
- Self-Replicating Treatment: Phages multiply at the site of infection until the host bacteria are eliminated.
Research institutions worldwide, including in the United States and Western Europe, are now investing heavily in phage research. This represents a full-circle moment for d'Hérelle's pioneering vision.
Foundation of Molecular Biology
Perhaps d'Hérelle's most profound, though indirect, legacy is his contribution to the birth of molecular biology. In the 1940s and 1950s, bacteriophages became the model organism of choice for pioneering geneticists.
The "Phage Group," led by scientists like Max Delbrück and Salvador Luria, used phages to unravel the fundamental principles of life. Their experiments with phage replication and genetics answered critical questions about how genes function and how DNA operates as the genetic material.
Key discoveries like the mechanism of DNA replication, gene regulation, and the structure of viruses were made using bacteriophages. The 1969 Nobel Prize in Physiology or Medicine was awarded to Delbrück, Luria, and Herschel for their work on phage genetics.
This means that the tools and knowledge that underpin modern biotechnology and genetic engineering can trace their origins back to d'Hérelle's initial isolation and characterization of these viruses. He provided the raw material for a scientific revolution.
Honors, Recognition, and Lasting Tributes
Although Félix d'Hérelle did not receive a Nobel Prize, his work earned him numerous other prestigious accolades during his lifetime. These honors acknowledged the transformative nature of his discoveries.
He was awarded the Leeuwenhoek Medal by the Royal Netherlands Academy of Arts and Sciences in 1925. This medal, awarded only once every decade, is considered the highest honor in microbiology. It recognized him as the most significant microbiologist of his era.
He was also made an honorary member of numerous scientific societies across Europe and North America. These memberships were a testament to the international respect he commanded, despite his unconventional background.
The Eliava Institute: A Living Legacy
The most enduring tribute to d'Hérelle's work is the Eliava Institute of Bacteriophage, Microbiology, and Virology in Tbilisi, Georgia. Founded with his close collaborator George Eliava, the institute has remained a global leader in phage therapy for over a century.
While the Western world abandoned phage therapy for antibiotics, the Eliava Institute continued to treat patients and refine its techniques. Today, it attracts patients from around the globe who have infections untreatable by conventional antibiotics.
The institute stands as a physical monument to d'Hérelle's vision. It continues his mission of healing through the intelligent application of natural biological agents.
Conclusion: The Enduring Impact of Félix d'Hérelle
Félix d'Hérelle's story is a powerful reminder that revolutionary ideas can come from outside established systems. His lack of formal academic training did not hinder his ability to see what others missed. His greatest strength was his power of observation and his willingness to follow the evidence wherever it led.
He was a true pioneer who entered uncharted scientific territory. His discovery of bacteriophages opened up multiple new fields of study. From medicine to agriculture to genetics, his influence is deeply woven into the fabric of modern science.
Key Takeaways from a Revolutionary Career
The life and work of Félix d'Hérelle offer several critical lessons for science and innovation.
- Curiosity Drives Discovery: A simple observation of clear spots on a细菌 lawn led to a world-changing breakthrough.
- Application is Key: D'Hérelle immediately sought to apply his discovery to solve real-world problems like disease and famine.
- Persistence Overcomes Skepticism: He championed his ideas relentlessly, even when faced with doubt from the establishment.
- Interdisciplinary Vision: He effortlessly connected microbiology with medicine, public health, and agriculture.
His career demonstrates that the most significant scientific contributions often defy traditional boundaries and expectations.
A Legacy for the Future
Today, as we confront the looming threat of a post-antibiotic era, d'Hérelle's work is more relevant than ever. Phage therapy is being re-evaluated as a crucial weapon in the fight against superbugs. Research into using phages in food safety and agriculture is also expanding.
Furthermore, bacteriophages continue to be indispensable tools in laboratories worldwide. They are used in genetic engineering, synthetic biology, and basic research. The field of molecular biology, which they helped create, continues to transform our world.
Félix d'Hérelle's legacy is not confined to the history books. It is a living, evolving force in science and medicine. From a self-taught microbiologist in Guatemala to a father of modern virology, his journey proves that a single curious mind can indeed change the world. His story inspires us to look closely, think boldly, and harness the power of nature to heal and protect.


Decoding Life: The Scientific Legacy of Sydney Brenner
Few scientists have shaped our understanding of life's fundamental processes like Sydney Brenner, a South African-born British biologist. As a central architect of modern molecular biology, Sydney Brenner made groundbreaking discoveries across genetics, developmental biology, and genomics. His work to decipher the genetic code and establish powerful model organisms created a blueprint for biological research that continues to guide scientists today.
The Architect of Molecular Biology's Golden Age
Sydney Brenner was a pivotal figure during what many call the golden age of molecular biology. His intellectual curiosity and collaborative spirit led to discoveries that answered some of the 20th century's most profound biological questions. Brenner's career was marked by a unique ability to identify crucial biological problems and pioneer the experimental tools needed to solve them.
Born in Germiston, South Africa, Brenner demonstrated exceptional scientific promise from a young age. He entered the University of Witwatersrand at just 14 years old and earned his medical degree. His quest for deeper biological understanding led him to Oxford University, where he completed his doctorate. This academic foundation set the stage for his historic contributions.
Brenner is widely recognized as one of the pioneers who presided over the golden age of molecular biology, establishing principles that enabled modern gene technology.
Groundbreaking Work in Cracking the Genetic Code
One of Sydney Brenner's earliest and most significant contributions was his work on deciphering the genetic code. After joining the prestigious Medical Research Council Laboratory of Molecular Biology in Cambridge, Brenner began collaborating with Francis Crick. Together, they tackled the mystery of how genetic information stored in DNA translates into functional proteins.
Proving the Triplet Nature of Codons
Brenner and Crick's collaboration produced a monumental breakthrough: proving that the genetic code is based on triplet codons. Through brilliant theoretical reasoning and experimentation, they demonstrated that a sequence of three nucleotides encodes a single amino acid. Brenner himself coined the essential term "codon" to describe these three-letter genetic words.
His work provided critical evidence against the theory of overlapping coding sequences. Brenner proved that the coding function of DNA was separate from its structural constraints, a fundamental concept in molecular genetics. This separation was essential for understanding how genetic information flows from genes to proteins.
Identifying the Stop Signal for Protein Synthesis
Beyond establishing the triplet code, Brenner made another crucial discovery. He identified a specific nonsense codon—the combination of uracil, adenine, and guanine—that signals the termination of protein translation. This discovery explained how cells know when to stop building a protein chain, completing our understanding of the genetic code's punctuation.
The impact of this work cannot be overstated. Cracking the genetic code provided the Rosetta Stone of molecular biology, allowing scientists to read and interpret the instructions within DNA. Brenner's contributions in this area alone would have secured his legacy, but he was only beginning his revolutionary scientific journey.
The Co-Discovery of Messenger RNA (mRNA)
While working on the genetic code, Sydney Brenner made another earth-shattering discovery with François Jacob and Matthew Meselson. In 1961, they proved the existence of messenger RNA (mRNA), solving a major mystery in molecular biology. Their experiments demonstrated that mRNA acts as a transient intermediate, carrying genetic instructions from DNA in the nucleus to the protein-making ribosomes in the cytoplasm.
This discovery filled a critical gap in the central dogma of molecular biology, which describes the flow of genetic information. Before Brenner's work, scientists struggled to understand exactly how DNA's information reached the cellular machinery that builds proteins. The identification of mRNA provided the missing link.
The significance of this breakthrough was immediately recognized by the scientific community. For his role in discovering messenger RNA, Brenner received the prestigious Albert Lasker Award for Basic Medical Research in 1971. This achievement highlights Brenner's extraordinary talent for identifying and solving foundational biological problems.
The discovery of messenger RNA was so significant that it earned Sydney Brenner the prestigious Albert Lasker Award for Basic Medical Research in 1971.
Establishing C. elegans: A Revolution in Biological Research
By the mid-1960s, with the genetic code essentially solved, Sydney Brenner deliberately shifted his research focus. He recognized that biology needed a new model organism to tackle the complexities of development and neurobiology. His visionary choice was the tiny, transparent roundworm Caenorhabditis elegans.
Why C. elegans Became the Perfect Model
Brenner selected C. elegans for several brilliant strategic reasons that demonstrated his deep understanding of experimental science:
- Genetic Simplicity: The worm has a small, manageable genome.
- Transparent Body: Researchers can observe cell division and development in living organisms under a microscope.
- Short Lifecycle: It completes its life cycle in just three days, enabling rapid genetic studies.
- Invariant Cell Lineage: Every worm develops identically, with exactly 959 somatic cells in the adult hermaphrodite.
Brenner's pioneering work proved that the worm's development—the timing, location, and fate of every cell division—was completely determined by genetics. He published his foundational paper, "The Genetics of Caenorhabditis elegans," in 1974, effectively creating an entirely new field of research.
The Transformational Impact of a Tiny Worm
The establishment of C. elegans as a model organism was arguably Brenner's most transformative contribution to biological science. This simple nematode became a powerful experimental system for investigating:
- Genetic regulation of organ development
- Programmed cell death (apoptosis)
- Nervous system structure and function
- Ageing and longevity
- Human disease mechanisms
Brenner succeeded in cloning most portions of the C. elegans DNA, creating essential tools for future researchers. His vision created a research paradigm that allowed scientists to study complex processes in a simple, genetically tractable animal. The choice of this model organism would ultimately lead to Nobel Prize-winning discoveries and continues to drive biomedical research today.
Genomics Pioneering and Vertebrate Model Development
Never content to rest on past achievements, Sydney Brenner continued to push scientific boundaries throughout his career. In the 1990s, he turned his attention to vertebrate genomics, recognizing the need for compact model genomes to advance genetic research. His innovative approach led to the introduction of an unusual but brilliant model organism: the pufferfish.
The Fugu Genome Project Breakthrough
Brenner introduced the pufferfish (Takifugu rubripes, commonly known as fugu) as a model vertebrate genome for comparative genomics. Despite being a vertebrate with complex biology similar to humans, the fugu has an exceptionally compact genome approximately 400 million base pairs in size. This is roughly eight times smaller than the human genome.
The compact nature of the fugu genome made it ideal for genetic studies. Brenner recognized that this streamlined DNA contained essentially the same genes as other vertebrates but with less non-coding "junk" DNA. This allowed researchers to identify functional elements and genes more efficiently than in larger, more complex genomes.
Brenner introduced the pufferfish as a model vertebrate genome, pioneering comparative genomics with its compact 400 million base pair genome.
Revolutionizing DNA Sequencing Technology
Sydney Brenner's contributions extended beyond biological discovery into technological innovation. He played a crucial role in advancing DNA sequencing methods that would eventually enable massive genomic projects. His work helped bridge the gap between early sequencing techniques and the high-throughput methods we rely on today.
Inventing Microbead Array-Based Sequencing
Brenner pioneered microbead array-based DNA sequencing technology, an approach that would influence future generations of sequencing platforms. This innovative method used microscopic beads to capture DNA fragments, allowing for parallel processing of multiple sequences simultaneously. This represented a significant step toward the high-throughput sequencing methods essential for modern genomics.
His work demonstrated the power of parallel processing in genetic analysis. By processing many DNA sequences at once, researchers could achieve unprecedented scale and efficiency. This approach foreshadowed the next-generation sequencing technologies that would later revolutionize biological research and medical diagnostics.
Commercial Applications and Lynx Therapeutics
Brenner's sequencing innovations found practical application through his work with Lynx Therapeutics. He collaborated with the company to develop massively parallel signature sequencing (MPSS), one of the first true next-generation sequencing methods. This technology could process millions of DNA fragments simultaneously, dramatically increasing sequencing capacity.
The MPSS system represented a quantum leap in sequencing capability. It utilized complex biochemical processes on microbeads to decode short DNA sequences in parallel. This work laid important groundwork for the DNA sequencing revolution that would follow in the 2000s, making large-scale genomic projects economically feasible.
Nobel Prize Recognition and Scientific Honors
The ultimate recognition of Sydney Brenner's scientific impact came in 2002 when he received the Nobel Prize in Physiology or Medicine. He shared this prestigious award with H. Robert Horvitz and John E. Sulston for their discoveries concerning "genetic regulation of organ development and programmed cell death."
The Nobel-Winning Research on Programmed Cell Death
The Nobel Committee specifically recognized Brenner's foundational work establishing C. elegans as a model organism for studying development. His colleagues Sulston and Horvitz had built upon this foundation to make crucial discoveries about programmed cell death (apoptosis). Their research revealed the genetic pathway that controls how and when cells deliberately die during development.
This Nobel Prize highlighted the far-reaching implications of Brenner's decision to work with C. elegans. The discoveries about cell death regulation have profound implications for understanding cancer, autoimmune diseases, and neurodegenerative disorders. When apoptosis fails to function properly, cells may multiply uncontrollably or fail to die when they should.
In 2002, Sydney Brenner shared the Nobel Prize in Physiology or Medicine for discoveries concerning genetic regulation of organ development and programmed cell death.
Additional Prestigious Awards and Recognition
Beyond the Nobel Prize, Brenner received numerous other honors throughout his distinguished career. These awards reflect the breadth and depth of his scientific contributions across multiple domains of biology:
- Albert Lasker Award for Basic Medical Research (1971) for the discovery of messenger RNA
- Royal Medal from the Royal Society (1974) for his contributions to molecular biology
- Gairdner Foundation International Award (1991) recognizing his outstanding biomedical research
- King Faisal International Prize in Science (1992) for his genetic research
- Copley Medal (2017) from the Royal Society, its oldest and most prestigious award
Brenner was elected to numerous prestigious academies, including the Royal Society, the National Academy of Sciences, and Germany's national academy of sciences, the Leopoldina. These memberships reflected the international recognition of his scientific leadership and the global impact of his research.
Leadership in Scientific Institutions and Mentorship
Throughout his career, Sydney Brenner demonstrated exceptional leadership in shaping scientific institutions and mentoring future generations of researchers. His vision extended beyond his own laboratory work to creating environments where innovative science could flourish.
The Molecular Sciences Institute in Berkeley
In 1995, Brenner founded the Molecular Sciences Institute in Berkeley, California with support from the Philip Morris Company. He sought to create an unconventional research environment where young scientists could pursue ambitious projects with intellectual freedom. The institute reflected Brenner's belief in supporting creative, boundary-pushing science without excessive bureaucratic constraints.
Brenner led the Institute until his retirement in 2000, establishing it as a center for innovative biological research. His leadership philosophy emphasized scientific independence and intellectual rigor. He believed that the best science emerged when talented researchers had the freedom to follow their scientific curiosity wherever it led.
Later Career at the Salk Institute
After retiring from the Molecular Sciences Institute, Brenner was appointed a Distinguished Professor at the Salk Institute in La Jolla, California. This appointment brought him full circle, reuniting him with his longtime collaborator Francis Crick, who had also joined the Salk Institute. Their renewed collaboration continued until Crick's death in 2004.
At Salk, Brenner continued to contribute his immense knowledge and experience to the scientific community. He maintained an active interest in emerging fields and technologies, always looking toward the future of biological research. His presence at Salk provided invaluable mentorship to younger scientists and continued his legacy of scientific excellence.
Scientific Philosophy and Approach to Research
Sydney Brenner's extraordinary scientific output was guided by a distinctive philosophy and approach to research. His methods and mindset offer valuable lessons for scientists across all disciplines.
The Importance of Choosing the Right Problem
Brenner was legendary for his ability to identify fundamental biological problems that were both important and solvable. He often emphasized that asking the right question was more important than having the right answer to the wrong question. This strategic approach to problem selection allowed him to make contributions that transformed entire fields.
His decision to switch from genetic code research to developmental biology demonstrated this philosophy perfectly. Having essentially solved the coding problem, he deliberately moved to what he saw as the next great challenge in biology: understanding multicellular development. This strategic shift led to his most influential work with C. elegans.
Innovation in Experimental Design
Brenner's innovative spirit extended to his experimental approaches. He consistently developed or adapted new methods to answer his scientific questions. From establishing C. elegans as a model organism to pioneering new sequencing technologies, Brenner understood that scientific progress often required methodological innovation.
His work demonstrates the importance of creating the right tools for the job. Rather than being limited by existing techniques, Brenner frequently invented new approaches when necessary. This willingness to innovate methodologically was a key factor in his ability to make breakthrough discoveries across multiple areas of biology.
The Enduring Scientific Legacy of Sydney Brenner
Sydney Brenner's impact on biological science extends far beyond his specific discoveries. His work established foundational principles that continue to guide research across multiple disciplines. Brenner's legacy includes not only what he discovered, but how he approached scientific problems and the tools he created for future generations.
The establishment of C. elegans as a model organism alone has generated an entire research ecosystem. Thousands of laboratories worldwide continue to use this tiny worm to study fundamental biological processes. Brenner's vision created a research paradigm that has produced multiple Nobel Prizes and countless scientific breakthroughs.
Impact on Modern Biomedical Research
Brenner's contributions directly enabled advances in understanding human disease mechanisms. The genetic pathways discovered in C. elegans have proven remarkably conserved in humans. Research on programmed cell death has led to new cancer treatments that target apoptosis pathways.
His work on the genetic code and mRNA laid the foundation for modern biotechnology and pharmaceutical development. Today's mRNA vaccines and gene therapies stand on the foundation Brenner helped build. The sequencing technologies he pioneered enable personalized medicine and genetic diagnostics.
Brenner's Influence on Scientific Culture and Education
Beyond his research achievements, Sydney Brenner shaped scientific culture through his mentorship and scientific communication. He trained numerous scientists who themselves became leaders in their fields. His approach to science emphasized creativity, intellectual courage, and collaboration.
Mentorship and Training Future Leaders
Brenner's laboratory served as a training ground for many prominent biologists. His mentorship style combined high expectations with generous intellectual freedom. He encouraged young scientists to pursue ambitious questions and develop their own research directions.
Many of his trainees have described how Brenner's guidance shaped their scientific careers. He emphasized the importance of scientific intuition and creative problem-solving. His legacy includes not only his discoveries but the generations of scientists he inspired and trained.
Scientific Communication and Writing
Brenner was known for his clear, often witty scientific writing and presentations. His ability to explain complex concepts in accessible terms made him an effective communicator. He wrote extensively about the philosophy of science and the future of biological research.
His famous "Life Sentences" columns in Current Biology showcased his talent for synthesizing complex ideas. These writings demonstrated his broad knowledge and his ability to connect disparate fields of science. Brenner's communication skills helped shape how molecular biology is taught and understood.
Brenner is widely recognized as one of the pioneers who presided over the golden age of molecular biology, establishing principles that enabled modern gene technology.
Brenner's Later Years and Final Contributions
Even in his later career, Sydney Brenner remained actively engaged with scientific developments. He continued to attend conferences, mentor younger scientists, and contribute to scientific discussions. His perspective as one of the founders of molecular biology gave him unique insights into the field's evolution.
Continued Scientific Engagement
Brenner maintained his characteristic curiosity throughout his life. He followed developments in genomics, neuroscience, and computational biology with keen interest. His ability to see connections between different scientific domains remained sharp until his final years.
He continued to offer valuable perspectives on the direction of biological research. Brenner often commented on emerging technologies and their potential impact. His experience allowed him to distinguish between fleeting trends and truly transformative developments.
Recognition and Honors in Later Life
In his final decades, Brenner received numerous additional honors recognizing his lifetime of achievement. These included the 2002 Nobel Prize and the Royal Society's Copley Medal in 2017. These late-career recognitions underscored the enduring significance of his contributions.
The scientific community continued to celebrate his work through special symposia and dedicated issues of scientific journals. These events brought together scientists whose work built upon Brenner's foundational discoveries. They demonstrated how his influence continued to shape biological research.
The Philosophical Underpinnings of Brenner's Approach
Sydney Brenner's scientific philosophy represented a unique blend of rigorous methodology and creative thinking. His approach to research offers enduring lessons for scientists across all disciplines.
The Importance of Simple Model Systems
Brenner's most profound insight may have been his recognition that complex biological problems often require simple experimental systems. His choice of C. elegans demonstrated that understanding basic principles in simple organisms could illuminate human biology. This approach has become central to modern biomedical research.
He understood that biological complexity could be best unraveled by studying systems where variables could be controlled. This philosophy has guided the development of model organisms from yeast to zebrafish. Brenner proved that simplicity could be the key to understanding complexity.
Interdisciplinary Thinking
Brenner's work consistently crossed traditional disciplinary boundaries. He moved seamlessly between genetics, biochemistry, developmental biology, and computational science. This interdisciplinary approach allowed him to see connections that specialists might miss.
His career demonstrates the power of synthesis across fields. Brenner's ability to incorporate insights from different domains enabled his most creative work. This approach has become increasingly important as biology becomes more integrated with physics, engineering, and computer science.
Quantifying Brenner's Scientific Impact
The scale of Sydney Brenner's influence can be measured through various metrics that demonstrate his extraordinary impact on biological science.
Citation Impact and Scientific Publications
Brenner's publications have been cited tens of thousands of times, with several papers achieving classic status. His 1974 paper "The Genetics of Caenorhabditis elegans" alone has been cited over 5,000 times. This paper essentially created an entire field of research that continues to grow.
His work on messenger RNA and the genetic code generated foundational papers that are still referenced today. The enduring relevance of his publications demonstrates how his work established principles that remain central to molecular biology.
Nobel Prize Legacy and Scientific Lineage
The Nobel Prize Brenner shared in 2002 was just one indicator of his impact. More significantly, his work directly enabled at least two additional Nobel Prizes awarded to scientists who built upon his foundations. The C. elegans system he created has been described as a "Nobel Prize factory."
His scientific lineage extends through multiple generations of researchers. Many prominent biologists today can trace their intellectual ancestry back to Brenner's laboratory. This scientific genealogy represents one of the most meaningful measures of his lasting influence.
Conclusion: The Enduring Legacy of a Scientific Visionary
Sydney Brenner's career represents one of the most productive and influential in the history of biological science. His contributions span the foundational discoveries of molecular biology's golden age to the genomic revolution of the 21st century. Brenner exemplified the combination of deep theoretical insight and practical experimental innovation.
His work established fundamental principles that continue to guide biological research. The genetic code, messenger RNA, model organism genetics, and DNA sequencing technologies all bear his distinctive imprint. Brenner's ability to identify crucial problems and develop innovative solutions set a standard for scientific excellence.
The most remarkable aspect of Brenner's legacy may be its continuing expansion. Each year, new discoveries build upon the foundations he established. The C. elegans system he created continues to yield insights into human biology and disease. The sequencing technologies he helped pioneer enable new approaches to medicine and research.
Sydney Brenner demonstrated that scientific progress depends on both brilliant discovery and the creation of tools for future discovery. His career reminds us that the most important scientific contributions are those that enable further exploration. Through his work and the generations of scientists he inspired, Brenner's influence will continue to shape biology for decades to come.
His life's work stands as a testament to the power of curiosity, creativity, and courage in scientific pursuit. Sydney Brenner not only decoded life's fundamental processes but also showed us how to ask the questions that matter most. This dual legacy ensures his permanent place among the greatest scientists of any generation.

Frederick Banting: Nobel Laureate Who Discovered Insulin
Sir Frederick Grant Banting stands as a monumental figure in medical history. His co-discovery of insulin in the early 1920s transformed a deadly diagnosis into a manageable condition. This article explores his life, his groundbreaking research, and his lasting legacy in diabetes care and beyond.
A Canadian physician and surgeon, Banting's work saved and continues to save millions of lives worldwide. His Nobel Prize-winning achievement at the age of 32 remains one of science's most profound humanitarian breakthroughs. We will delve into the journey that led to this momentous discovery.
Early Life and Path to Medicine
Frederick Banting was born on November 14, 1891, on a farm near Alliston, Ontario. His rural upbringing instilled a strong sense of perseverance and hard work. Initially, he enrolled at Victoria College, University of Toronto, to study divinity and become a minister.
A pivotal change in direction occurred when he transferred to the study of medicine. He graduated in 1916, as World War I raged in Europe. His medical training was accelerated due to the wartime need for physicians. This decision set him on the path that would later change the world.
Service and Injury in World War I
After graduation, Banting immediately joined the Canadian Army Medical Corps. He served as a surgeon in England and later in France. During the Battle of Cambrai in 1918, he displayed exceptional courage while treating wounded soldiers under heavy fire.
Despite being severely wounded in the arm by shrapnel, he continued to care for patients for over sixteen hours. For his heroism, he was awarded the Military Cross, one of the highest military honors. This injury, however, complicated his initial plans for a career as an orthopedic surgeon.
Post-War Medical Practice and Research Idea
After the war, Banting completed his surgical training and began a practice in orthopedic surgery in London, Ontario. He also took a part-time teaching position at the University of Western Ontario. It was while preparing a lecture on the pancreas in October 1920 that a transformative idea struck him.
He read a medical journal article linking pancreatic islets to diabetes. Banting conceived a novel method to isolate the internal secretion of these islets. He famously scribbled his idea in a notebook: "Diabetus. Ligate pancreatic ducts of dog. Keep dogs alive till acini degenerate leaving Islets. Try to isolate the internal secretion of these to relieve glycosurea."
The Historic Discovery of Insulin
Driven by his hypothesis, Banting moved to Toronto in the summer of 1921 to pursue his research. Professor J.J.R. Macleod of the University of Toronto provided laboratory space and resources. Macleod also assigned a young medical student, Charles Best, to assist Banting for the summer.
Their early experiments involved surgically ligating the pancreatic ducts in dogs to degenerate the enzyme-producing cells, leaving the islet cells intact. They then extracted the material from these islets, which they initially called "isletin."
Critical Experiments and Refinement
The team faced numerous challenges and failures. However, by July 30, 1921, they successfully extracted a pancreatic extract that lowered the blood sugar of a diabetic dog. This proved the extract's life-saving potential. The substance was soon renamed insulin.
To purify the extract for human use, biochemist James Collip joined the team later in 1921. His expertise was crucial in refining a sufficiently pure and consistent batch of insulin. This collaborative effort was intense and sometimes fraught with personal tension.
Banting and Best famously sold the insulin patent to the University of Toronto for a symbolic $1, with Banting stating, "Insulin belongs to the world, not to me."
First Human Trial and Immediate Impact
The first human recipient was a 14-year-old boy named Leonard Thompson, who was dying from type 1 diabetes in Toronto General Hospital. The first injection in January 1922 caused an allergic reaction due to impurities. After Collip's further purification, a second injection was administered.
The results were nothing short of miraculous. Thompson's dangerously high blood glucose levels dropped to near-normal ranges. His strength returned, and he gained weight. Leonard Thompson survived, living for another 13 years with insulin therapy, proving the treatment's revolutionary efficacy.
The Nobel Prize and Controversy
In 1923, the Nobel Assembly awarded the Nobel Prize in Physiology or Medicine for the discovery of insulin. The prize was awarded jointly to Frederick Banting and J.J.R. Macleod. This decision immediately sparked controversy, as it overlooked the direct laboratory contributions of Charles Best and James Collip.
Feeling that Best's role was seminal, Banting publicly announced he would share his prize money with his young assistant. Macleod later split his share with Collip. This episode highlights the often-complex nature of attributing credit in scientific discoveries made by teams.
- Youngest Winner: At 32, Banting became the youngest Nobel laureate in Physiology or Medicine at that time.
- First Canadian: He was also the first Canadian to win a Nobel Prize in this category.
- Enduring Debate: Historical accounts continue to analyze the contributions of all four key figures.
The award solidified the importance of insulin on the world stage. It also brought Banting immense fame and pressure. Despite the acclaim, he remained deeply committed to the humanitarian purpose of his work, ensuring affordable access to the life-saving hormone.
Banting's Later Scientific Career and Aviation Medicine
After the whirlwind of the insulin discovery and Nobel Prize, Frederick Banting continued his scientific pursuits with vigor. He was appointed a professor at the University of Toronto and continued medical research. However, his interests expanded significantly beyond endocrinology into new and critical fields.
He dedicated considerable energy to cancer research and the study of silicosis. Banting also maintained his artistic side, taking up painting as a serious hobby. His paintings, often landscapes, provided a creative outlet from his intense scientific work.
Pioneering Contributions to Aviation Medical Research
With the growing threat of World War II, Banting turned his formidable research skills to a national defense priority. In 1939, he was appointed Chairman of Canada's Associate Committee on Aviation Medical Research. He threw himself into this role, focusing on the physiological challenges faced by pilots.
His committee's work was pragmatic and directly aimed at improving pilot safety and performance. Key research areas included the effects of high-altitude flight, oxygen deprivation, and G-forces on the human body. Banting understood that aviation medicine was crucial for Allied air superiority.
- Carbon Monoxide Detection: His team developed improved methods for detecting deadly carbon monoxide in aircraft cabins.
- Protective Eyewear: They pioneered the development of anti-fogging and shatterproof goggles for pilots.
- Early Helmet Design: Research was conducted on protective helmets to mitigate the impact of crashes and turbulence.
- Cold Weather Survival: Studies focused on the physiology of survival in extreme cold for downed airmen.
This work established a foundation for Canadian expertise in aerospace medicine that continues to this day. Banting's ability to pivot from a laboratory-focused researcher to a leader in applied military science demonstrated his versatility and deep patriotism.
The Tragic Death of a National Hero
Frederick Banting's life was cut short on February 21, 1941. He was en route to England aboard a Lockheed Hudson bomber to deliver crucial research findings and discuss wartime collaboration in aviation medicine. The plane crashed shortly after takeoff from Gander, Newfoundland, killing Banting and two other crew members instantly.
The pilot, Captain Joseph Mackey, survived the crash and later recounted that Banting, though seriously injured, helped him escape the wreckage before succumbing to his own injuries. This final act of heroism was consistent with Banting's character, evidenced decades earlier on the battlefields of WWI.
Banting's death at age 49 was mourned across Canada and the scientific world as a profound loss. Prime Minister Mackenzie King called him "one of Canada's greatest sons," and he was given a state funeral in Toronto.
The Enduring Legacy of His Final Mission
His mission to England underscored the strategic importance he placed on his aviation research. The work of his committee directly contributed to the safety and effectiveness of Allied air crews throughout the war. While the insulin discovery defined his public legacy, his contributions to wartime science were a significant second act.
The crash site remains a place of historical significance. A memorial was later erected near Musgrave Harbour, Newfoundland. His death highlighted the risks taken by scientists and personnel during the war, even those not on the front lines of direct combat.
Frederick Banting's Legacy and Honors
Frederick Banting's legacy is multifaceted, encompassing medical innovation, national pride, and ongoing scientific inspiration. His name is synonymous with one of the most important medical breakthroughs of the 20th century. This legacy is preserved through numerous honors, institutions, and continued public remembrance.
In Canada, he is celebrated as a national hero. His image appeared on the Canadian $100 bill for many years until the series was redesigned. This prominent placement on the banknote was a testament to his status as a figure of monumental national importance.
Institutions and Memorials
Several major institutions bear his name, ensuring his contributions are never forgotten. The Banting and Best Department of Medical Research at the University of Toronto continues his tradition of inquiry. Banting House in London, Ontario, where he had his crucial idea, is now a National Historic Site of Canada and museum dubbed "The Birthplace of Insulin."
Furthermore, the Banting Research Foundation was established to fund innovative health research in Canada. World Diabetes Day, observed on November 14th, is held on his birthday, creating a permanent global link between his legacy and the ongoing fight against the disease.
- Banting Postdoctoral Fellowships: Prestigious Canadian government awards for top-tier researchers.
- Statues and Plaques: Numerous public memorials exist across Canada, including at the University of Toronto and the Parliament of Canada.
- International Recognition: He was knighted by King George V in 1934, becoming Sir Frederick Banting.
The Centennial of Insulin and Modern Reflections
The year 2021 marked the 100th anniversary of Banting and Best's initial successful experiments. This centennial was commemorated worldwide by diabetes organizations, research institutions, and patient communities. It was a moment to reflect on how far treatment has come and the distance still to go.
The University of Toronto and other institutions hosted special events, publications, and exhibitions. These highlighted not only the historical discovery but also its modern implications. The centennial underscored insulin as a starting point, not an endpoint, in diabetes care.
From Animal Extract to Modern Analogs
The insulin Banting's team extracted from dogs and later cows was life-saving but imperfect. It was relatively short-acting and could cause immune reactions. Today, thanks to genetic engineering, we have human insulin and advanced analogs.
Modern synthetic insulins offer precise action profiles—rapid-acting, long-acting, and premixed varieties. This allows for much tighter and more flexible blood glucose management. Delivery methods have also evolved dramatically from syringes to insulin pumps and continuous glucose monitors.
Despite these advancements, the core principle Banting proved—that replacing the missing hormone could treat diabetes—remains the bedrock of therapy for millions with type 1 diabetes worldwide.
Ongoing Challenges and Access to Medicine
A central theme of the 2021 reflections was Banting's humanitarian ethos. His decision to sell the patent for $1 was a conscious effort to ensure broad, affordable access. This stands in stark contrast to modern controversies over the high cost of insulin in some countries, particularly the United States.
Advocates often invoke Banting's original intent in campaigns for drug pricing reform. The centennial served as a reminder that the moral imperative of accessibility is as important as the scientific breakthrough itself. Ensuring all who need insulin can afford it is viewed by many as fulfilling Banting's vision.
Recent articles from institutions like the University of Toronto have also revisited his lesser-known legacy in aviation medicine. This has brought a more complete picture of his scientific career to public attention, showcasing his versatility and commitment to applying science to urgent human problems, whether chronic disease or wartime survival.
The Team Behind the Discovery: Collaboration and Controversy
The story of insulin’s discovery is a powerful case study in scientific collaboration and its attendant complexities. While Frederick Banting is the most famous name associated with insulin, he worked within a talented team. The roles of Charles Best, J.J.R. Macleod, and James Collip were all indispensable to the final success.
Banting provided the initial hypothesis and relentless drive, while Best executed the day-to-day experiments with skill and dedication. Macleod provided the essential institutional support, laboratory resources, and broader physiological expertise. Collip’s biochemical prowess was critical for purifying the extract for human use.
Analyzing the Nobel Prize Decision
The Nobel Committee's 1923 decision to award the prize only to Banting and Macleod remains a subject of historical debate. This choice reflected the scientific conventions of the era, which often credited the senior supervising scientist and the principal ideator. The contributions of junior researchers like Best and specialists like Collip were frequently overlooked.
Banting’s immediate and public decision to share his prize money with Best was a clear acknowledgment of this perceived injustice. Similarly, Macleod shared his portion with Collip. This action speaks to the internal acknowledgment within the team that the discovery was a collective achievement.
- Banting's Role: Vision, surgical skill, and determination.
- Best's Role: Technical execution of experiments and data collection.
- Macleod's Role: Supervision, resources, and scientific guidance.
- Collip's Role: Biochemical purification for clinical application.
Modern historical analysis tends to recognize the "Toronto Four" as the complete team behind the discovery. This nuanced view honors the collaborative nature of modern scientific breakthroughs, where diverse expertise is essential for turning an idea into a life-saving therapy.
Banting's Personal Life and Character
Beyond the laboratory, Frederick Banting was a man of strong character, humility, and diverse interests. He was known for his straightforward manner, resilience, and a deep sense of duty. These personal qualities profoundly shaped his scientific and medical career.
He married twice, first to Marion Robertson in 1924, with whom he had one son, William. The marriage ended in divorce in 1932. He later became engaged to Henrietta Ball, who was with him in Newfoundland before his final flight. His personal life, however, was often secondary to his consuming dedication to his work.
The Artist and the Scientist
Banting found a creative counterbalance to his scientific work in painting. He was a skilled amateur artist who took his painting seriously, studying under prominent Canadian artists like A.Y. Jackson of the Group of Seven. His landscapes demonstrate a keen eye for detail and a love for the Canadian wilderness.
This artistic pursuit was not merely a hobby; it was a refuge. It provided a mental space for reflection and a different mode of seeing the world. The combination of scientific rigor and artistic sensitivity made him a uniquely rounded individual, showing that creativity fuels innovation across disciplines.
Colleagues noted that Banting was intensely focused and could be stubborn, but he was also generous and deeply committed to the humanitarian application of science, famously forgoing vast wealth to ensure insulin reached those in need.
The Global Impact of Insulin on Diabetes Treatment
The introduction of insulin marked a paradigm shift in medicine. Before 1922, a diagnosis of type 1 diabetes was a virtual death sentence, particularly for children. Patients were subjected to starvation diets that only prolonged life for a short, miserable period.
Insulin therapy transformed this bleak reality almost overnight. It was the first effective treatment for a chronic endocrine disease, proving that hormone replacement could successfully manage a previously fatal condition. This paved the way for subsequent hormone therapies.
From Survival to Thriving: The Evolution of Diabetes Management
The initial goal of insulin therapy was simple survival. Today, the objectives are vastly more ambitious: enabling people with diabetes to live long, healthy, and fulfilling lives. Advances built upon Banting’s work have made this possible.
Modern diabetes care focuses on tight glycemic control to prevent complications such as heart disease, kidney failure, and blindness. Technology like continuous glucose monitors (CGMs) and insulin pumps allows for unprecedented precision in management. These tools represent the ongoing evolution of Banting’s foundational discovery.
- Increased Lifespan: Life expectancy for people with type 1 diabetes has increased by decades.
- Quality of Life: Modern regimens allow for greater dietary flexibility and physical activity.
- Ongoing Research: Work continues on islet cell transplantation, artificial pancreases, and ultimately, a cure.
Banting's Legacy in Modern Medical Research
Frederick Banting’s legacy extends far beyond the molecule of insulin. His story continues to inspire new generations of researchers, physicians, and students. He embodies the ideal of the physician-scientist who moves seamlessly from patient-oriented questions to fundamental laboratory investigation.
Research institutions that bear his name, like the Banting and Best Department of Medical Research, continue to operate at the forefront of biomedical science. The Banting Postdoctoral Fellowships are among Canada’s most prestigious awards, attracting top scientific talent from around the world to conduct research in the country.
Lessons for Today's Scientists
Banting’s career offers several enduring lessons. It demonstrates the power of a simple, well-defined idea pursued with tenacity. It highlights the critical importance of collaboration across different specialties. Most importantly, it shows that scientific achievement is fundamentally connected to human benefit.
His decision regarding the insulin patent remains a powerful ethical benchmark. In an era of biotechnology and pharmaceutical commerce, Banting’s stance that a life-saving discovery "belongs to the world" challenges us to balance innovation with accessibility and equity.
Conclusion: The Enduring Significance of Frederick Banting
Frederick Banting’s life was a remarkable journey from a rural Ontario farm to the pinnacle of scientific achievement. His co-discovery of insulin stands as one of the most transformative events in the history of medicine. It turned a deadly disease into a manageable condition and gave hope to millions.
His legacy is not confined to a single discovery. His heroic service in two world wars, his pioneering work in aviation medicine, and his artistic pursuits paint a portrait of a complex and multifaceted individual. Banting was a national hero who embodied perseverance, ingenuity, and profound humanity.
The story of insulin is ongoing. While Banting and his team provided the key that unlocked the door, scientists continue to build upon their work, striving for better treatments and a ultimate cure. The centennial celebrations in 2021 were not just about honoring the past but also about reinforcing commitment to the future of diabetes care.
Frederick Banting’s greatest legacy is the breath of life he gave to countless individuals and the enduring inspiration he provides to all who seek to use science as a force for good. His work reminds us that dedicated individuals can indeed change the world.
In remembering Sir Frederick Banting, we celebrate more than a historical figure; we celebrate the very ideal of scientific progress in the service of humanity. His life continues to inspire a simple, powerful truth: that curiosity, coupled with compassion, can conquer some of humanity’s most daunting challenges.


Asclepiades de Bitinia: El médico griego innovador
Asclepiades de Bitinia fue un médico griego que revolucionó la práctica médica en la antigua Roma. Nacido alrededor del 124 a.C., introdujo teorías basadas en partículas y un enfoque humanitario radicalmente diferente a las prácticas de su tiempo. Su legado sienta las bases precursoras de conceptos modernos como la medicina molecular y la psicoterapia.
Llegó a Roma hacia el 91 a.C., donde su filosofía médica, centrada en el bienestar del paciente, ganó rápida popularidad. Se opuso firmemente a tratamientos violentos como las sangrías, prefiriendo métodos como dietas, masajes y musicoterapia. Esta perspectiva lo consolidó como una figura pionera en la historia de la medicina.
Vida y contexto histórico de Asclepiades
Originario de Prusa, en Bitinia (actual Turquía), Asclepiades recibió una formación excepcional en filosofía y retórica antes de dedicarse a la medicina. Su traslado a Roma marcó un punto de inflexión, donde inicialmente ejerció como orador. Pronto, su aguda mente analítica lo llevó a aplicar principios filosóficos al arte de la curación, fundando la influyente Escuela Metódica.
Este contexto histórico se caracterizaba por el dominio de la teoría humoral hipocrática. Asclepiades desafió este dogma con un enfoque basado en la observación clínica directa y causas físicas naturales. Su éxito en Roma demostró la efectividad de sus métodos pragmáticos y romanos, alejados de las explicaciones sobrenaturales.
Formación y llegada a Roma
Se cree que Asclepiades estudió en la prestigiosa escuela de Alejandría, absorbiendo los conocimientos médicos más avanzados de su era. Su background en retórica le fue invaluable para persuadir a la sociedad romana de la validez de sus innovadoras ideas. No fue un médico común, sino un pensador revolucionario que aplicó la lógica a la práctica médica.
Su llegada a Roma coincidió con un período de receptividad hacia la cultura griega. Asclepiades supo capitalizar este entorno, ganando fama entre la élite romana por sus tratamientos efectivos y poco invasivos. Su carrera demuestra la integración del conocimiento griego en el mundo romano.
La teoría corpuscular: una visión revolucionaria
La contribución más significativa de Asclepiades fue su teoría corpuscular de la enfermedad. Postulaba que el cuerpo estaba compuesto de partículas infinitesimales, que llamó ónkos (masas o moléculas). Las enfermedades, según él, surgían cuando el movimiento o la disposición de estas partículas se alteraba, bloqueando los poros del cuerpo.
Esta idea fue un claro precursor de las teorías atómicas y moleculares modernas. Clasificó las enfermedades en dos categorías principales: agudas/graves y dinámicas/estáticas, basándose en el estado de estas partículas. Este sistema ofrecía un marco racional y físico para entender la salud, rompiendo con las explicaciones míticas.
Precursor de la microbiología moderna
Lo más sorprendente de su teoría es que, de manera visionaria, sugirió la existencia de partículas invisibles causantes de enfermedad. Un análisis reciente de 2025 lo posiciona como un precursor de la microbiología. Aunque no las llamó microbios, su concepto de partículas dañinas anticipó el trabajo de científicos como Louis Pasteur siglos después.
Esta perspectiva materialista y mecanicista permitía explicar los fenómenos patológicos sin recurrir a espíritus o desequilibrios de humores. Su enfoque ponía el acento en causas tangibles y observables, sentando las bases para el método científico en medicina.
La teoría de Asclepiades sobre partículas invisibles causantes de enfermedad lo erige como un visionario, precursor de campos modernos como la microbiología.
Innovaciones pioneras en la práctica médica
Asclepiades de Bitinia no solo fue un teórico, sino un médico de immense habilidad práctica. A él se le atribuye la realización de la primera traqueotomía electiva de la historia, según registran Galeno y Areteo de Capadocia. Este procedimiento, arriesgado para su época, salvaba vidas al evitar la asfixia.
Sus innovaciones abarcaron tanto lo físico como lo mental. Diferenció con notable precisión entre ilusiones y alucinaciones, un concepto avanzado para su tiempo. También estableció una clasificación pionera de las enfermedades psiquiátricas, distinguiedo entre condiciones agudas y crónicas.
Avances en el tratamiento de pacientes
Su enfoque de tratamiento era notablemente humanitario y no invasivo. Rechazaba las prácticas comunes y peligrosas de su época, como las sangrías profusas o la administración de fármacos extremadamente fuertes. En su lugar, abogaba por una medicina suave y natural centrada en la comodidad del paciente.
Entre sus terapias preferidas se encontraban:
- Dieta equilibrada: Ajustaba la alimentación como base de la recuperación.
- Hidroterapia y masajes: Utilizaba baños y manipulación corporal para restaurar el equilibrio.
- Ejercicio moderado: Promovía la actividad física como parte esencial del tratamiento.
- Musicoterapia: Empleaba la música para calmar la mente y el cuerpo.
Este conjunto de prácticas lo convierte en un claro antecedente histórico de disciplinas modernas como la fisioterapia y la psicoterapia. Su filosofía era simple pero poderosa: ayudar a la naturaleza en su trabajo de curación, no obstaculizarla con intervenciones violentas.
La Escuela Metódica y su legado duradero
El impacto de Asclepiades se institucionalizó con la fundación de la Escuela Metódica. Esta escuela representaba un enfoque pragmático y romano, en contraste con las escuelas griegas más teóricas. Se centraba en el tratamiento de síntomas observables, priorizando la eficacia práctica sobre el dogmatismo.
La influencia de esta escuela se extendió durante siglos, influyendo en figuras monumentales como Galeno, quien, aunque criticó algunos aspectos de su teoría, adoptó su énfasis en la observación. El legado de Asclepiades perduró en la medicina europea, enfatizando siempre el bienestar del paciente como objetivo principal.
Su visión de una medicina empírica y empática resuena profundamente con las tendencias actuales hacia un cuidado sanitario más holístico. Asclepiades demostró, hace más de dos milenios, que la eficacia médica y la compasión pueden y deben ir de la mano.
Tratamientos humanitarios y oposición a prácticas dañinas
Una de las mayores contribuciones de Asclepiades de Bitinia fue su firme rechazo a las prácticas médicas violentas comunes en la antigüedad. Se opuso radicalmente a las sangrías excesivas, los purgantes agresivos y el confinamiento de enfermos mentales. En su lugar, implementó un sistema de terapias suaves y naturales que priorizaban el bienestar del paciente.
Su filosofía se basaba en la creencia de que el cuerpo poseía una capacidad innata para la autocuración. El rol del médico, según Asclepiades, era facilitar este proceso natural, no interferir con él de manera traumática. Este enfoque humanitario y empático contrastaba fuertemente con los métodos predominantes de su tiempo.
Liberación y terapia para enfermos mentales
En el campo de la salud mental, Asclepiades fue un verdadero revolucionario. En una época donde los trastornos psíquicos se atribuían a posesiones demoníacas y se trataban con castigos, él defendió un tratamiento compasivo. Ordenaba liberar a los pacientes de sus cadenas y proponía terapias en entornos abiertos y tranquilos.
Su aproximación incluía:
- Conversación terapéutica: Dialogaba con los pacientes para entender sus angustias.
- Actividades ocupacionales: Incorporaba trabajos manuales sencillos como terapia.
- Exposición a la naturaleza: Creía en el poder curativo de los entornos naturales.
- Musicoterapia: Utilizaba melodías suaves para calmar la mente agitada.
Estas prácticas lo convierten en un precursor de la psiquiatría moderna. Su clasificación de enfermedades mentales en agudas y crónicas demostraba una comprensión sofisticada de los trastornos psíquicos, muy adelantada a su tiempo.
Diferenciación clave: Asclepiades vs. Asclepio
Es crucial no confundir a Asclepiades de Bitinia, el médico histórico, con Asclepio (Esculapio para los romanos), el dios griego de la medicina. Mientras Asclepio era una deidad cuyo culto implicaba curaciones milagrosas mediante rituales de incubación, Asclepiades representaba todo lo contrario: la medicina basada en la razón y la observación.
El culto a Asclepio floreció en santuarios como el de Epidauro, donde los enfermos dormían en recintos sagrados esperando sueños curativos del dios. Se documentan hasta 400 enclaves dedicados a su culto en el mundo griego. Asclepiades, en cambio, rechazaba explícitamente las explicaciones sobrenaturales de la enfermedad.
Dos visiones opuestas de la curación
La diferencia fundamental radica en sus enfoques:
- Asclepio (dios): Curación mediante intervención divina y rituales religiosos.
- Asclepiades (médico): Curación mediante métodos naturales y comprensión científica.
- Santuario de Epidauro: Centros de peregrinación para curaciones milagrosas.
- Escuela Metódica: Institución educativa basada en principios racionales.
Esta distinción es esencial para comprender la verdadera revolución que representó Asclepiades. Mientras la medicina tradicional dependía de la fe, él estableció las bases para una práctica médica independiente de lo sobrenatural, basada en causas físicas observables.
La claridad al diferenciar entre el dios Asclepio y el médico Asclepiades es fundamental para apreciar su contribución histórica a la secularización de la medicina.
Legado e influencia en la medicina posterior
El impacto de Asclepiades se extendió mucho más allá de su vida en la Roma del siglo I a.C. Su Escuela Metódica continuó influyendo en la práctica médica durante varios siglos, sentando las bases para el desarrollo de la medicina occidental. Figuras como Temisón de Laodicea y luego Sorano de Éfeso fueron importantes continuadores de su legado.
Incluso Galeno, aunque criticó aspectos específicos de la teoría corpuscular, adoptó muchos de los principios prácticos de Asclepiades. El énfasis en la observación clínica directa y el trato humano al paciente se convirtieron en pilares duraderos de la práctica médica gracias a su influencia.
Influencia en el Renacimiento y la medicina moderna
Durante el Renacimiento, el redescubrimiento de textos antiguos revitalizó el interés por las ideas de Asclepiades. Su enfoque mecanicista del cuerpo humano resonó con los nuevos paradigmas científicos emergentes. Muchos historiadores ven en su teoría corpuscular un antecedente directo de la fisiología moderna.
Su legado específico incluye:
- Medicina molecular: Su concepto de partículas (ónkos) anticipó la biología molecular.
- Psicoterapia humanista: Su trato a enfermos mentales influyó en approaches modernos.
- Fisioterapia: Sus uso de ejercicio y masajes como terapia fue pionero.
- Medicina preventiva: Su énfasis en dieta y estilo de vida saludable.
Lo más notable es cómo su filosofía médica anticipó tendencias actuales como la medicina integrativa y los enfoques centrados en el paciente. Su visión holística del cuidado sanitario demuestra una remarkable permanencia a través de los milenios.
Relevancia contemporánea y reconocimiento actual
En años recientes, ha resurgido el interés académico por la figura de Asclepiades de Bitinia. Publicaciones de 2024 y 2025 han destacado su papel pionero en la humanización de la medicina y su sorprendente anticipación de conceptos modernos. Su figura gana visibilidad en la divulgación científica contemporánea.
Particularmente notable es el reconocimiento de su idea sobre "partículas invisibles" causantes de enfermedad como un precursor de la teoría microbiana. Este insight, que pasó desapercibido durante siglos, hoy se valora como una de sus contribuciones más visionarias.
Asclepiades en el debate médico actual
Su legado es especialmente relevante en debates contemporáneos sobre:
- Medicina centrada en el paciente: Su enfoque anticipa movimientos modernos contra la medicalización excesiva.
- Salud mental humanitaria: Su tratamiento de enfermos psiquiátricos sigue siendo modelo de compasión.
- Enfoques holísticos: Su integración de múltiples terapias resuena con la medicina integrativa actual.
- Prevención sobre curación: Su énfasis en estilo de vida saludable anticipa medicina preventiva.
La cronología de su reconocimiento es elocuente: desde su práctica en Roma alrededor del 91 a.C. hasta publicaciones que en 2025 lo reivindican como visionario. Esta continuidad de influencia a lo largo de más de dos milenios testimonia la profundidad y permanencia de sus contribuciones al arte de curar.
El redescubrimiento contemporáneo de Asclepiades como precursor de la microbiología y la psiquiatría humanitaria demuestra la vigencia atemporal de su pensamiento médico.
La figura de Asclepiades sigue inspirando a profesionales de la salud que buscan equilibrar el avance tecnológico con un trato compasivo hacia los pacientes. Su legado subraya que la medicina efectiva debe combinar rigor científico con empatía humana, una lección tan relevante hoy como hace dos mil años.
Contribuciones específicas a la medicina moderna
Las ideas de Asclepiades de Bitinia anticiparon de manera extraordinaria varios campos médicos contemporáneos. Su enfoque basado en partículas y su comprensión de la enfermedad como un fenómeno físico sentaron las bases para desarrollos científicos posteriores. La conexión entre su pensamiento y disciplinas actuales es sorprendentemente directa.
Su clasificación de enfermedades y sus protocolos de tratamiento no farmacológicos encuentran eco en las tendencias más vanguardistas de la medicina del siglo XXI. Asclepiades demostró que la observación cuidadosa y la lógica podían producir avances médicos significativos sin necesidad de tecnología compleja.
Precursor de la fisiatría y rehabilitación
La insistencia de Asclepiades en el uso del ejercicio, los masajes y los baños terapéuticos lo convierte en un claro antecedente de la fisioterapia moderna. Él entendió el valor del movimiento para mantener la salud y restaurar la función corporal tras una enfermedad. Su enfoque integral del cuerpo como sistema que responde a estímulos físicos fue revolucionario.
Sus técnicas de rehabilitación incluían:
- Kinesiterapia temprana: Movimientos específicos para restaurar función.
- Hidroterapia sistemática: Uso terapéutico del agua a diferentes temperaturas.
- Masaje terapéutico: Manipulación de tejidos para aliviar dolencias.
- Terapia ocupacional básica: Actividades diseñadas para mejorar capacidades.
Estas prácticas, documentadas por sus seguidores, establecieron principios que solo serían redescubiertos y formalizados científicamente muchos siglos después. Su legado en este campo es fundamental pero a menudo subestimado en la historia de la rehabilitación médica.
La teoría corpuscular y su relación con la ciencia actual
La teoría corpuscular desarrollada por Asclepiades representa uno de los primeros intentos de explicar la salud y la enfermedad mediante principios físicos materiales. Su concepto de que el cuerpo estaba compuesto por partículas mínimas (ónkos) que podían desordenarse o bloquearse, aunque primitivo, contiene el germen de ideas científicas posteriores.
Esta visión mecanicista del cuerpo humano contrastaba radicalmente con las explicaciones sobrenaturales o humorales predominantes. Asclepiades propuso que las enfermedades tenían causas físicas identificables, un principio fundamental de la medicina científica moderna.
De las partículas a los microbios: una evolución conceptual
La conexión más fascinante entre la teoría de Asclepiades y la ciencia actual es su anticipación de la microbiología. Cuando hablaba de partículas diminutas causantes de enfermedad, esencialmente describía conceptualmente lo que siglos después se identificarían como microorganismos patógenos.
La visión de Asclepiades sobre partículas invisibles causantes de enfermedad representa un salto conceptual monumental hacia la teoría microbiana que solo sería confirmada en el siglo XIX.
Esta perspectiva incluye varios elementos proféticos:
- Agentes externos: Su idea de partículas dañinas que entran al cuerpo.
- Transmisión: Implícitamente, su teoría sugería mecanismos de contagio.
- Especificidad: Diferentes partículas para diferentes enfermedades.
- Tratamiento dirigido: Restaurar el orden de partículas específicas.
La revalorización reciente de esta dimensión de su pensamiento, especialmente en publicaciones de 2025, ha reposicionado a Asclepiades como una figura de importancia capital en la historia de las ideas científicas sobre la enfermedad.
Críticas y limitaciones de su pensamiento
A pesar de su brillantez visionaria, el sistema médico de Asclepiades tenía limitaciones importantes según los estándares actuales. Galeno, su gran sucesor crítico, señaló debilidades en su teoría corpuscular, particularmente su incapacidad para explicar ciertos fenómenos fisiológicos complejos. Estas críticas son importantes para una evaluación equilibrada y objetiva de su legado.
Su rechazo total a la farmacología fuerte y a ciertos procedimientos quirúrgicos, aunque humanitario, podría haber limitado su capacidad para tratar algunas condiciones graves. La medicina moderna reconoce que diferentes enfermedades requieren diferentes enfoques, desde terapias suaves hasta intervenciones agresivas cuando son necesarias.
Evaluación histórica contemporánea
Los historiadores de la medicina evalúan a Asclepiades considerando:
- Contexto histórico: Sus innovaciones vistas contra el trasfondo de su época.
- Influencia duradera: Su impacto en generaciones posteriores de médicos.
- Conceptos anticipatorios: Ideas que prefiguraron desarrollos científicos posteriores.
- Limitaciones inevitables: Restricciones impuestas por el conocimiento disponible en su tiempo.
Esta evaluación balanceada nos permite apreciar sus contribuciones sin caer en la hagiografía. Asclepiades fue un innovador extraordinario, pero también un producto de su tiempo con las limitaciones cognitivas y tecnológicas propias de la antigüedad.
Conclusión: el legado permanente de Asclepiades
El viaje histórico de Asclepiades de Bitinia desde la antigua Roma hasta el reconocimiento contemporáneo como visionario médico es testimonio de la profundidad de sus contribuciones. Su figura encarna la transición desde una medicina basada en lo sobrenatural hacia una práctica fundamentada en observación racional y empatía clínica.
Su legado multidimensional abarca desde anticipaciones conceptuales de la microbiología hasta la fundación de principios de la psicoterapia humanista. Asclepiades demostró que la compasión y la ciencia no son incompatibles, sino complementarias en el arte de curar.
Lecciones para la medicina contemporánea
La revalorización actual de Asclepiades ofrece lecciones cruciales para la práctica médica del siglo XXI:
- Equilibrio entre tecnología y humanismo: Su enfoque recuerda la importancia del trato humano junto al avance técnico.
- Prevención y tratamiento suave: Su énfasis en terapias naturales anticipa la medicina integrativa.
- Enfoque holístico del paciente: Su visión del enfermo como persona integral, no como conjunto de síntomas.
- Escepticismo científico saludable: Su rechazo a dogmas establecidos sin evidencia observacional.
Estas lecciones resuenan especialmente en nuestra era de medicalización extrema y especialización fragmentada. Asclepiades representa un modelo de práctica médica integral que trasciende su contexto histórico específico.
La figura de Asclepiades de Bitinia permanece como un faro en la historia de la medicina, recordándonos que el progreso científico debe ir siempre acompañado de compasión humana y respeto por la autonomía del paciente.
Desde su innovadora teoría corpuscular hasta su revolucionario tratamiento de enfermos mentales, desde su fundación de la Escuela Metódica hasta su influencia en Galeno y más allá, Asclepiades modeló un camino diferente para la medicina. Su cronología vital, desde su nacimiento alrededor del 124 a.C. hasta su práctica en Roma desde el 91 a.C., enmarca una carrera de extraordinaria influencia y visionaria anticipación.
Hoy, cuando la medicina enfrenta desafíos de deshumanización y excesiva especialización, el legado de Asclepiades ofrece un recordatorio poderoso: que en el corazón de la práctica médica efectiva yace siempre la combinación de observación cuidadosa, razonamiento lógico y compasión genuina hacia quien sufre. Su historia nos inspira a buscar ese equilibrio en nuestra propia búsqueda por aliviar el dolor y promover la salud en todas sus dimensiones.
En conclusión, Asclepiades de Bitinia fue un pionero cuya filosofía humanitaria y sus teorías basadas en partículas desafiaron las convenciones médicas de su época. Su legado innovador no solo transformó la práctica en la antigua Roma, sino que también anticipó conceptos médicos modernos. Reflexionar sobre sus métodos nos invita a considerar cuáles de nuestras prácticas actuales serán vistas como obsoletas en el futuro.



Understanding HLA: The Immune System's Genetic Blueprint
What is Human Leukocyte Antigen (HLA)?
The Human Leukocyte Antigen (HLA) system is a critical component of the human immune system. Located on chromosome 6, these genes encode cell-surface proteins that play a pivotal role in regulating immune responses. By presenting peptide antigens to T cells, HLA molecules help the body distinguish between self and non-self cells, a fundamental process in immune defense.
The Structure and Function of HLA
Class I and Class II HLA Molecules
HLA molecules are categorized into two main classes: Class I (HLA-A, B, C) and Class II (HLA-DR, DQ, DP). Class I molecules are present on nearly all nucleated cells and are responsible for displaying intracellular peptides, such as those derived from viruses, to CD8+ cytotoxic T cells. This interaction is crucial for the elimination of infected or malignant cells.
Class II molecules, on the other hand, are found on antigen-presenting cells and present extracellular antigens to CD4+ helper T cells. This process is essential for initiating and coordinating immune responses against pathogens.
Class III Genes
In addition to Class I and II, HLA also includes Class III genes, which encode proteins involved in inflammation, such as complement components and tumor necrosis factor-alpha (TNF-alpha). These proteins play a significant role in the body's inflammatory responses and overall immune regulation.
The Role of HLA in Immune Regulation
Distinguishing Self from Non-Self
The primary function of HLA is to distinguish between self and non-self cells. This is achieved through the presentation of peptide antigens to T cells. In a healthy state, HLA molecules suppress the presentation of self-antigens, preventing autoimmune responses. Disruptions in this process can lead to autoimmunity, where the immune system mistakenly attacks the body's own cells.
Influence on Disease Susceptibility
Variations in HLA genes can influence an individual's susceptibility to certain diseases. For example, specific HLA alleles have been linked to an increased risk of developing autoimmune diseases such as multiple sclerosis (MS) and severe infections. Understanding these genetic variations is crucial for developing personalized treatment strategies.
The Importance of HLA in Transplantation
Matching Donors and Recipients
HLA typing is essential for matching donors and recipients in organ and stem cell transplants. A close match between the donor and recipient HLA types minimizes the risk of transplant rejection. Incompatible HLA molecules can trigger host T-cell or antibody responses, leading to graft rejection.
Transplant Success and HLA Matching
The success of a transplant is significantly influenced by the degree of HLA matching. A 6/6 HLA match is considered ideal for unrelated donors. Mismatches can increase the risk of rejection by 20-50%, highlighting the importance of precise HLA typing in transplant procedures.
Recent Advances in HLA Research
Precision Medicine and Immunotherapy
Recent trends in HLA research emphasize the role of precision medicine. Advances in HLA typing are enhancing the effectiveness of immunotherapies, such as CAR-T cells and cancer vaccines. By targeting allele-specific peptide presentation, these therapies can be tailored to individual patients, improving treatment outcomes.
Computational Models for HLA-Peptide Binding
Improving computational models for HLA-peptide binding is another area of active research. These models support the development of personalized vaccines by predicting how different HLA alleles will interact with specific peptides. This approach holds great promise for the future of personalized medicine.
Conclusion
The Human Leukocyte Antigen (HLA) system is a cornerstone of the human immune system, playing a vital role in distinguishing self from non-self cells and regulating immune responses. Its significance in transplantation, disease susceptibility, and precision medicine underscores the importance of ongoing research and advancements in HLA typing and computational modeling.
The Genetic Diversity of HLA: A Double-Edged Sword
Extreme Polymorphism and Its Implications
The HLA system is renowned for its extreme polymorphism, with over 20,000 alleles identified across various loci. This genetic diversity is a double-edged sword: it enhances the body's ability to recognize a wide range of pathogens but also complicates transplantation processes. Each individual inherits one set of HLA genes from each parent, resulting in a unique combination that influences immune responses.
Heterozygosity and Pathogen Recognition
Most individuals are heterozygous at HLA loci, meaning they have different alleles for each gene. This heterozygosity is advantageous as it broadens the spectrum of peptides that can be presented to T cells, thereby enhancing pathogen recognition. However, this diversity also means that finding a perfect match for organ transplants can be challenging.
HLA and Autoimmune Diseases: The Connection
HLA Alleles and Disease Susceptibility
Certain HLA alleles have been strongly associated with an increased risk of developing autoimmune diseases. For instance, specific variants of HLA-DRB1 are linked to conditions such as rheumatoid arthritis and multiple sclerosis. These associations highlight the critical role of HLA in maintaining immune tolerance and preventing autoimmune responses.
Mechanisms of Autoimmunity
In autoimmunity, the immune system fails to distinguish between self and non-self antigens, leading to the destruction of healthy tissues. HLA molecules play a pivotal role in this process by presenting self-antigens to T cells. When this presentation goes awry, it can trigger an autoimmune response. Understanding these mechanisms is crucial for developing targeted therapies.
HLA in Cancer Immunity and Immunotherapy
Tumor Surveillance and HLA
HLA molecules are integral to the body's ability to surveil and eliminate cancerous cells. They present tumor-specific antigens to T cells, which can then mount an immune response against the tumor. However, cancer cells often evolve mechanisms to evade this surveillance, such as downregulating HLA expression or altering the peptides presented.
Advances in Cancer Immunotherapy
Recent advances in cancer immunotherapy have leveraged the HLA system to enhance the body's natural defenses against tumors. Techniques such as CAR-T cell therapy and cancer vaccines are designed to target specific HLA-peptide complexes, thereby improving the precision and effectiveness of these treatments. These innovations hold great promise for the future of cancer treatment.
The Role of HLA in Pregnancy and Alloimmunization
Maternal-Fetal HLA Interactions
During pregnancy, the maternal immune system must tolerate the presence of fetal cells that express paternal HLA molecules. This tolerance is crucial for a successful pregnancy. However, in some cases, the maternal immune system may develop antibodies against these foreign HLA molecules, leading to complications such as alloimmunization.
Alloimmunization and Its Consequences
Alloimmunization can occur not only during pregnancy but also as a result of blood transfusions or organ transplants. When the immune system is exposed to foreign HLA molecules, it may produce antibodies that can attack these molecules, leading to transplant rejection or other complications. Understanding and managing alloimmunization is essential for improving the outcomes of these medical procedures.
Computational Models and HLA-Peptide Binding
Predicting HLA-Peptide Interactions
Computational models are increasingly being used to predict how different HLA alleles will interact with specific peptides. These models are based on extensive databases of HLA-peptide binding data and use machine learning algorithms to make accurate predictions. This approach is particularly useful for developing personalized vaccines and immunotherapies.
Applications in Personalized Medicine
The use of computational models in HLA research is revolutionizing the field of personalized medicine. By accurately predicting HLA-peptide interactions, researchers can design vaccines and therapies that are tailored to an individual's unique HLA profile. This personalized approach has the potential to significantly improve the efficacy and safety of medical treatments.
Challenges and Future Directions in HLA Research
Overcoming Transplant Rejection
One of the major challenges in HLA research is overcoming transplant rejection. Despite advances in HLA typing and matching, finding a perfect match for organ transplants remains difficult. Future research aims to develop new strategies for inducing immune tolerance and reducing the risk of rejection, thereby improving transplant outcomes.
Enhancing Immunotherapy Efficacy
Another key area of focus is enhancing the efficacy of immunotherapies. While current immunotherapies have shown promise, they are not effective for all patients. Future research aims to identify new targets and develop more precise therapies that can overcome the limitations of current treatments.
Conclusion
The Human Leukocyte Antigen (HLA) system is a complex and dynamic component of the human immune system. Its role in distinguishing self from non-self, regulating immune responses, and influencing disease susceptibility underscores its importance in health and medicine. Ongoing research and advancements in HLA typing, computational modeling, and immunotherapy hold great promise for the future of personalized medicine and transplant success.
HLA Testing: Methods and Clinical Applications
Traditional HLA Typing Techniques
Historically, HLA typing relied on serological methods, where antibodies were used to identify specific HLA antigens on cells. While effective, these techniques had limitations in resolution and specificity. Modern molecular methods, such as PCR-based sequencing, have revolutionized HLA typing by providing higher resolution and accuracy.
Next-Generation Sequencing (NGS) in HLA Typing
The advent of Next-Generation Sequencing (NGS) has significantly advanced HLA typing capabilities. NGS allows for high-throughput sequencing of HLA genes, enabling the identification of novel alleles and providing a more comprehensive understanding of an individual's HLA profile. This technology is particularly valuable in transplant matching and disease association studies.
The Impact of HLA on Drug Hypersensitivity
HLA-Associated Adverse Drug Reactions
Certain HLA alleles are strongly associated with an increased risk of adverse drug reactions. For example, the HLA-B*57:01 allele is linked to hypersensitivity reactions to the HIV drug abacavir. Identifying these associations is crucial for predicting and preventing adverse drug reactions, thereby improving patient safety.
Pharmacogenomics and HLA
The field of pharmacogenomics explores how genetic variations, including those in HLA genes, influence drug responses. By integrating HLA typing into pharmacogenomic testing, healthcare providers can tailor drug therapies to individual patients, minimizing the risk of adverse reactions and optimizing treatment efficacy.
HLA and Infectious Disease Susceptibility
HLA Variants and Pathogen Resistance
Specific HLA variants have been shown to confer resistance or susceptibility to certain infectious diseases. For instance, the HLA-B*53 allele is associated with protection against severe malaria. Understanding these genetic associations can provide valuable insights into the mechanisms of infectious disease resistance and inform the development of targeted therapies.
HLA in Viral Infections
HLA molecules play a critical role in the immune response to viral infections. They present viral peptides to T cells, initiating an immune response. However, some viruses have evolved mechanisms to evade HLA-mediated immunity, such as downregulating HLA expression or producing proteins that interfere with antigen presentation. Research in this area is essential for developing effective antiviral therapies.
Ethical Considerations in HLA Research and Applications
Privacy and Genetic Data
The use of HLA typing and genetic data raises important ethical considerations, particularly regarding privacy and data security. As HLA typing becomes more widespread, it is crucial to establish robust protocols for protecting individuals' genetic information and ensuring that it is used responsibly and ethically.
Equity in Access to HLA-Based Therapies
Ensuring equitable access to HLA-based therapies is another critical ethical issue. Advances in personalized medicine and immunotherapy should be accessible to all individuals, regardless of socioeconomic status or geographic location. Addressing disparities in access to these technologies is essential for promoting health equity.
The Future of HLA Research: Innovations and Breakthroughs
CRISPR and HLA Gene Editing
The emergence of CRISPR-Cas9 gene editing technology holds immense potential for HLA research. By precisely modifying HLA genes, researchers can explore new avenues for treating autoimmune diseases, improving transplant outcomes, and enhancing cancer immunotherapies. This technology could revolutionize the field of HLA-based medicine.
Artificial Intelligence in HLA Research
Artificial intelligence (AI) is increasingly being integrated into HLA research to analyze vast datasets and predict HLA-peptide interactions. AI algorithms can identify patterns and correlations that may not be apparent through traditional methods, accelerating the discovery of new therapeutic targets and improving the precision of personalized medicine.
Conclusion: The Pivotal Role of HLA in Health and Medicine
The Human Leukocyte Antigen (HLA) system is a cornerstone of the human immune system, playing a vital role in distinguishing self from non-self, regulating immune responses, and influencing disease susceptibility. From its critical function in transplantation to its impact on autoimmune diseases, cancer immunity, and infectious disease resistance, HLA is integral to numerous aspects of health and medicine.
Advances in HLA typing techniques, such as Next-Generation Sequencing, have significantly enhanced our ability to understand and utilize HLA information. These advancements, combined with innovations in gene editing and artificial intelligence, are paving the way for groundbreaking therapies and personalized medical approaches.
As we continue to unravel the complexities of the HLA system, it is essential to address ethical considerations and ensure equitable access to HLA-based technologies. By doing so, we can harness the full potential of HLA research to improve health outcomes and transform the landscape of modern medicine.
In conclusion, the HLA system stands as a testament to the intricate and dynamic nature of the human immune system. Its profound impact on health and disease underscores the importance of ongoing research and innovation in this field. As we look to the future, the possibilities for HLA-based therapies and personalized medicine are boundless, offering hope for improved treatments and enhanced quality of life for individuals worldwide.