Louis Pasteur: Pioneer of Microbiology and Modern Medicine
Louis Pasteur, a name synonymous with germ theory and lifesaving vaccines, fundamentally reshaped our understanding of the invisible world of microorganisms. His groundbreaking work in the 19th century laid the foundation for modern microbiology, immunology, and sterile medical practices. From developing the process of pasteurization to creating the first scientific vaccines, Pasteur's legacy continues to protect global public health today.
The Formative Years of a Scientific Mind
Born in Dole, France, in 1822, Louis Pasteur's early academic career was marked by a profound interest in chemistry and the physical sciences. His initial research focused on molecular asymmetry, specifically the optical activity of tartrate crystals, which earned him early recognition. This work demonstrated his meticulous approach to experimentation and observation, skills that would become crucial in his later microbiological studies. His academic appointments took him to universities in Strasbourg and Lille, where he began to apply his chemical expertise to practical industrial problems.
From Crystals to Fermentation: A Pivotal Shift
The local industries in Lille, particularly those involving fermentation for beer and vinegar production, presented Pasteur with a new set of challenges. Manufacturers were experiencing inconsistent results and spoilage, which led to significant economic losses. Pasteur's investigation into fermentation revealed that it was not a purely chemical process but was instead caused by living microorganisms, specifically yeast. Furthermore, he discovered that spoilage was caused by other, undesirable microbes contaminating the batches. This was a radical departure from the prevailing chemical theories of the time and marked his entry into the field of microbiology.
Confronting and Conquering Spontaneous Generation
The dominant scientific belief of the era, known as the doctrine of spontaneous generation, held that life could arise spontaneously from non-living matter. This theory suggested that microorganisms could simply appear in decaying broth. Pasteur, armed with his findings from fermentation studies, became a leading voice against this idea. He designed a series of elegant and decisive experiments to prove that microbes were present in the air and could be introduced to sterile environments, causing contamination.
The Swan-Neck Flask Experiment
Pasteur's most famous experiment involved the use of swan-neck flasks. He boiled a nutrient broth in these flasks to sterilize it, killing any existing microorganisms. The unique curved neck of the flask allowed air to enter but trapped dust particles and airborne microbes, preventing them from reaching the broth. The broth in these flasks remained clear and sterile indefinitely. However, when the flask was tilted so that the broth came into contact with the trapped particles in the neck, the broth quickly became cloudy with microbial growth. This simple yet powerful experiment effectively disproved spontaneous generation and provided strong evidence for the germ theory of disease.
Pasteur's work demonstrated that microorganisms are everywhere and are the true agents of fermentation, putrefaction, and disease.
The Birth of Pasteurization
Building on his understanding that microbes cause spoilage, Pasteur sought a practical solution for the French wine industry, which was suffering from unreliable products. He discovered that by heating wine to a specific temperature, well below its boiling point, he could kill the harmful bacteria responsible for spoilage without adversely affecting the wine's taste. This process, later named pasteurization in his honor, revolutionized food and beverage safety.
The application of pasteurization was soon extended to milk, drastically reducing the incidence of diseases like tuberculosis, scarlet fever, and typhoid that were transmitted through contaminated dairy. The principles of pasteurization remain a cornerstone of food safety protocols worldwide, saving countless lives.
Key Principles of Pasteurization:
- Temperature Control: Heating liquids to a specific temperature (e.g., 72°C for milk) for a set time.
- Pathogen Elimination: Effectively destroys harmful pathogens like E. coli and Listeria.
- Preservation: Significantly extends the shelf life of perishable goods.
A Foundation for Modern Medicine: Germ Theory and Antisepsis
Pasteur's work provided the scientific basis for the germ theory of disease, which posits that specific microorganisms are the cause of specific illnesses. This was a monumental shift from previous beliefs that diseases were caused by miasmas or imbalances in bodily humors. His research directly influenced contemporary surgeons, like Joseph Lister, who pioneered antiseptic surgery. By using carbolic acid to disinfect wounds and surgical instruments, Lister dramatically reduced post-operative infections, applying Pasteur's microbiological principles to clinical practice.
Pasteur himself contributed to the field of asepsis and antisepsis by developing methods to create and maintain sterile environments for his experiments. He designed specialized flasks and techniques to exclude external contaminants, ensuring the purity of his microbial cultures. This rigorous approach to sterility became the standard for microbiological and medical research laboratories.
Vaccinology: From Chicken Cholera to Rabies
Louis Pasteur's contributions to immunology represent one of the most profound advancements in medical history. His systematic approach moved vaccination from a practice based on observation, like Edward Jenner's smallpox vaccine, to a rigorous science. The journey began almost by accident in 1879 while he was studying chicken cholera. A culture of the bacteria was left unattended over a holiday, and when it was later injected into chickens, the birds became ill but did not die.
Pasteur made a brilliant deduction. He realized that the bacteria had become attenuated, or weakened, after exposure to oxygen. When these same chickens were later injected with a fresh, virulent strain of cholera, they proved to be immune. Pasteur had scientifically demonstrated that exposure to a weakened pathogen could confer immunity against its more dangerous form. He famously declared, "In the fields of observation, chance favors only the prepared mind," a testament to his methodical approach.
The Anthrax Vaccine Breakthrough
Emboldened by his success with chicken cholera, Pasteur turned his attention to anthrax, a devastating disease affecting livestock. He developed a method to attenuate the anthrax bacillus by cultivating it at a slightly elevated temperature. To prove the vaccine's efficacy to a skeptical public, he conducted a landmark public experiment in 1881 at a farm in Pouilly-le-Fort.
The experiment involved 50 sheep. Twenty-five were vaccinated with Pasteur's attenuated strain, while the other twenty-five served as controls. After a set period, all 50 sheep were injected with a lethal dose of anthrax. The results were dramatic and conclusive: all 25 vaccinated sheep survived, while the unvaccinated control group died. This public demonstration was a monumental success, silencing critics and proving the power of scientifically developed vaccines.
The Race for a Rabies Vaccine
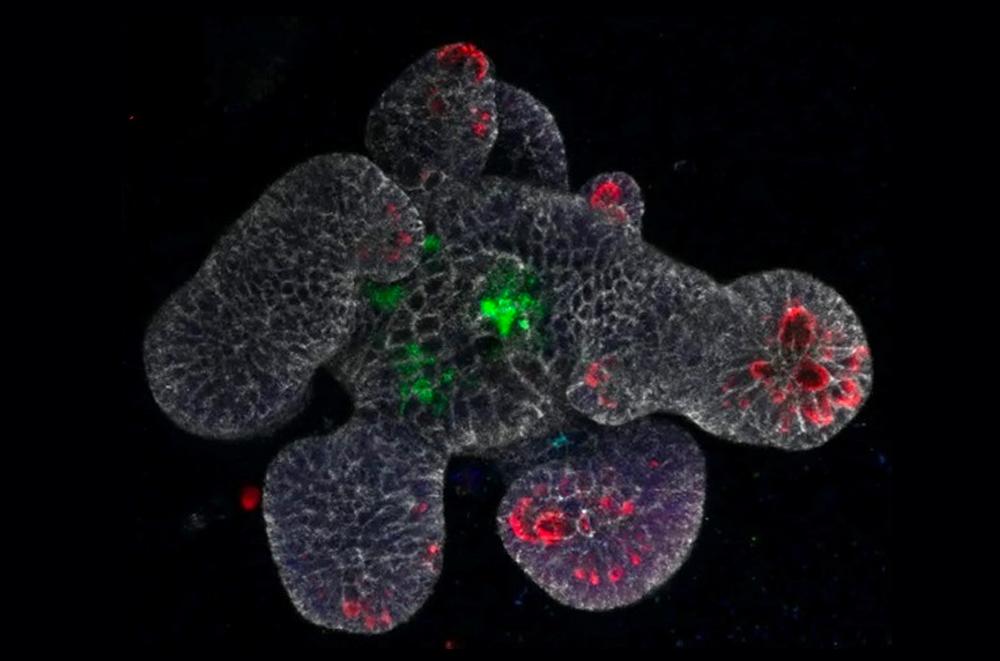
Perhaps Pasteur's most famous and daring work was on rabies, a fatal viral disease that terrified populations. Unlike bacteria, viruses were too small to be seen with the microscopes of the day, making the work exceptionally challenging. Pasteur and his team developed a method of attenuating the rabies virus by serial passage through rabbit spinal cords, which were then dried to weaken the pathogen further.
The ultimate test came in 1885 with nine-year-old Joseph Meister, who had been severely bitten by a rabid dog. With the boy facing almost certain death, Pasteur, though not a medical doctor, made the courageous decision to administer his untested vaccine. The treatment was a success, and Joseph Meister survived. This event catapulted Pasteur to international fame and marked the first successful human rabies vaccination, establishing a blueprint for future viral vaccines.
The successful treatment of Joseph Meister was a turning point, demonstrating that science could conquer even the most feared diseases.
The Establishment of the Pasteur Institute
The overwhelming international demand for the rabies vaccine, coupled with the need for a dedicated research center, led to the founding of the Pasteur Institute in Paris in 1888. Funded by a successful public subscription, the institute was created with a dual mission: to treat rabies and to serve as a center for research into infectious diseases. Pasteur served as its first director, setting its scientific course until his death.
The institute quickly became a world-leading center for microbiological research, attracting brilliant scientists from across the globe. It fostered an environment where groundbreaking discoveries continued to flourish long after Pasteur's own work. The institution's model combined fundamental research with practical applications, a philosophy that continues to drive its mission today.
A Global Legacy of Public Health
The Pasteur Institute expanded into a global network of institutions dedicated to fighting disease. These centers, located in over 20 countries, work on the front lines of public health, conducting research and responding to outbreaks. They have been instrumental in battling diseases such as the bubonic plague, diphtheria, influenza, and more recently, HIV/AIDS and COVID-19.
This global network ensures that Pasteur's legacy is not confined to history books but is an active, living force in contemporary medicine. The institutes continue the work he started, focusing on virology, immunology, and epidemiology to address the health challenges of the 21st century.
Pasteur's Enduring Impact on Modern Science
The principles established by Louis Pasteur form the bedrock of modern biomedical science. His insistence on rigorous experimentation, coupled with the practical application of findings, created a new paradigm for scientific inquiry. The fields of microbiology, immunology, and epidemiology all trace their modern foundations directly back to his work.
His refutation of spontaneous generation and championing of the germ theory provided a coherent framework for understanding the cause and spread of infectious diseases. This shift in thinking was as important as the individual discoveries themselves, as it provided the necessary context for future medical breakthroughs.
Core Scientific Principles Pioneered by Pasteur:
- The Germ Theory of Disease: Establishing that specific microbes cause specific illnesses.
- Attenuated Vaccines: Creating the scientific methodology for developing live-attenuated vaccines.
- Aseptic Technique: Developing protocols to maintain sterile environments in research and medicine.
- Biotechnology Foundations: Applying biological processes, like fermentation, for industrial use.
Influence on Food Safety and Public Health Policy
Beyond the laboratory and clinic, Pasteur's impact on daily life is immense. The mandatory pasteurization of milk and many other beverages has prevented millions of cases of foodborne illness. Public health policies regarding sanitation, water treatment, and food handling are all rooted in the understanding that invisible microbes must be controlled to ensure public safety.
Governments worldwide have established agencies, like the Centers for Disease Control and Prevention (CDC) in the United States, whose very existence is justified by the principles Pasteur helped establish. These organizations monitor disease, develop prevention strategies, and respond to outbreaks, all operating within the scientific framework he pioneered.
The Modern Applications of Pasteurian Microbiology
More than a century after his death, Louis Pasteur's principles are more relevant than ever. Modern microbiology, while vastly more complex, operates on the foundational framework he established. His core concepts—that specific microbes cause disease, that they can be controlled, and that immunity can be artificially induced—guide contemporary research in infectious diseases, vaccine development, and antimicrobial resistance.
Today's advanced vaccinology platform technologies, including mRNA and viral vector vaccines, are direct intellectual descendants of Pasteur's work with attenuated pathogens. While the tools have evolved, the goal remains identical: to safely train the immune system to recognize and defeat a pathogen. The rapid development of COVID-19 vaccines stands as a testament to the enduring power of the immunology principles he pioneered.
Combating Antimicrobial Resistance (AMR)
The global crisis of antimicrobial resistance finds its roots in Pasteur's warnings about the dynamic nature of microbes. His work established that microorganisms are living entities capable of adaptation and change. Modern strategies to combat AMR, such as phage therapy and the development of narrow-spectrum antibiotics, rely on a deep, Pasteurian understanding of microbial ecology and host-pathogen interactions.
Research into the human microbiome—the trillions of bacteria, viruses, and fungi that live in and on us—also stems from his recognition that microbes are not solely agents of disease. This field explores the delicate balance between health and illness, expanding germ theory into a more nuanced understanding of microbial symbiosis.
Pasteur's Legacy in Contemporary Research and Education
The Pasteur Institute remains a powerhouse of global health research. Its scientists are at the forefront of studying emerging infectious diseases, neuroscience, and genomics. The institute's ongoing work, from tracking viral evolution to developing new diagnostic tools, ensures that Pasteur's mandate to pursue science for the benefit of humanity continues unabated.
In academic settings worldwide, his experiments are still taught as masterclasses in the scientific method. The swan-neck flask experiment is a staple of biology textbooks, demonstrating the power of a simple, well-designed test to overturn longstanding dogma. His career is presented as a model of translating fundamental discovery into practical application that saves lives.
Key Institutions Upholding His Legacy
- The Pasteur Institute International Network: Over 30 institutes across five continents conducting collaborative research.
- National Public Health Agencies: Bodies like the CDC and WHO operate on principles of disease surveillance and control he helped establish.
- Food and Drug Administrations Globally: Regulatory bodies that enforce food safety standards based on pasteurization and microbial control.
Pasteur's greatest contribution may be the intellectual framework that allows each new generation of scientists to ask better questions.
Chronology of a Scientific Revolution
Understanding the sequence of Pasteur's discoveries reveals a logical progression from chemistry to applied microbiology. Each breakthrough built upon the last, creating a cohesive body of work that transformed multiple scientific fields.
Timeline of Major Contributions
1848 - 1857: Early work on molecular asymmetry and crystallography. Appointed professor at the University of Strasbourg and later Lille.
1856 - 1863: Investigations into fermentation, proving it is a biological process. Begins work disproving spontaneous generation.
1864 - 1870: Publicly demonstrates his swan-neck flask experiments. Develops pasteurization for wine and beer at the request of French industry.
1879 - 1881: Discovers principle of attenuation and creates first vaccine for chicken cholera. Develops and publicly validates the anthrax vaccine.
1885: Successfully administers the first rabies vaccine to Joseph Meister, achieving worldwide acclaim.
1888: The Pasteur Institute is inaugurated in Paris, with Pasteur as its first director.
Conclusion: The Indelible Mark of a Pioneer
Louis Pasteur's life and work represent a pivotal turning point in human history. He moved medicine from an era of superstition and observation into the age of scientific certainty and intervention. By proving the germ theory of disease, he gave humanity the knowledge needed to fight microscopic enemies effectively. His development of vaccines created a powerful shield against some of history's greatest killers.
The practical applications of his research are incalculable. Pasteurization alone has saved millions of lives by ensuring the safety of the food supply. The global vaccine industry, which prevents an estimated 2-3 million deaths per year from diseases like diphtheria, tetanus, and measles, is built upon his foundational discoveries. His establishment of aseptic technique transformed surgery from a deadly gamble into a safe, life-saving practice.
Final Takeaways on Pasteur's Impact
- Foundational Science: He established microbiology and immunology as distinct, rigorous scientific disciplines.
- Practical Humanitarian: He insisted on applying scientific discovery to solve real-world problems in industry and health.
- Methodological Rigor: His experimental designs remain gold standards for clarity and proof.
- Enduring Institutions: He created a model for collaborative research institutes that continues to drive discovery today.
In an era facing new pandemics, antimicrobial resistance, and emerging pathogens, the lessons of Louis Pasteur are not historical footnotes but essential guides. His legacy is not merely a list of discoveries, but a permanent shift in how humanity perceives and engages with the microbial world. He taught us to see the invisible, understand its mechanisms, and courageously intervene. From a glass of safe milk to a life-saving vaccination, the profound and benevolent shadow of Louis Pasteur, the father of microbiology, touches every life on the planet.

Manuel Elkin Patarroyo: Pioneer of Synthetic Malaria Vaccines
Manuel Elkin Patarroyo, a Colombian physician-scientist, revolutionized tropical disease research by creating the first modern chemically synthesized malaria vaccine candidate, SPf66. His work laid the foundation for modern vaccine development and highlighted the challenges of translational medicine. Patarroyo’s legacy combines groundbreaking science, institutional leadership, and ongoing debates about efficacy and ethics.
Manuel Elkin Patarroyo Biography and Early Career
Born in 1949, Patarroyo pursued medical studies in Colombia before specializing in tropical medicine. He earned a scholarship to study in London, where he became fascinated by malaria’s molecular biology. This early exposure sparked his lifelong mission to develop affordable vaccines for neglected diseases.
Educational Milestones and Scientific Awakening
Patarroyo’s academic journey included training at the London School of Hygiene & Tropical Medicine. His focus shifted to chemical synthesis of vaccine candidates, a radical departure from traditional methods. This approach would later define his pioneering work on synthetic peptides.
The Development of SPf66 Vaccine
In the mid-1980s, Patarroyo pioneered a novel approach: using synthetic peptides to mimic Plasmodium falciparum antigens. His team synthesized these peptides to create SPf66, published in 1987. The vaccine combined two key malaria proteins to trigger immune responses without live pathogens.
“Access to effective vaccines is a fundamental right, especially for those suffering from diseases ignored by global health systems.” – Manuel Elkin Patarroyo
Scientific Breakthrough and Initial Trials
Initial trials in Colombia showed promising results, leading to large-scale field tests across three continents. While 28% efficacy was reported in South America, results varied significantly in Africa and Asia. These disparities highlighted the complexity of malaria’s global impact.
- First published results: 1987
- Patent donated to WHO: 1993
- Major trial locations: Gambia, Tanzania, Thailand
Founding the Institute of Immunology
In the 1970s, Patarroyo established the Institute of Immunology at San Juan de Dios Hospital in Bogotá. This center became a hub for synthetic vaccine research, focusing on diseases like leishmaniasis and tuberculosis. The institute trained generations of scientists committed to affordable solutions for developing nations.
Institutional Impact and Legacy
The institute’s work emphasized low-cost vaccine development, aligning with Patarroyo’s belief in health equity. Researchers there developed protocols for synthesizing peptides at scale, reducing production costs. This model influenced vaccine programs across Latin America.
International Recognition and Honors
Patarroyo’s contributions earned global acclaim. He received the Prince of Asturias Prize and the Robert Koch Prize, among numerous other accolades. His work positioned Colombia as a leader in tropical disease research.
- Prince of Asturias Prize for Technical and Scientific Research
- Robert Koch Prize for Microbiology
- Over 20 honorary doctorates worldwide
These honors underscored his role in advancing “orphan diseases” affecting developing countries. Patarroyo consistently argued that scientific innovation must serve the most vulnerable populations.
Ethical Controversies and Scientific Criticisms
While Manuel Elkin Patarroyo’s work earned global praise, his career also faced significant criticism. Allegations about research ethics and mixed trial results sparked debates that continue to shape discussions about vaccine development standards.
Animal Welfare Concerns
Patarroyo’s preclinical testing involved capturing wild Aotus monkeys for SPf66 trials. Conservationists and animal-welfare groups raised alarms about sourcing practices and stress levels during experiments. These controversies led to increased scrutiny of primate use in vaccine research.
- Concerns focused on wild-caught monkeys from Colombian rainforests
- Critics cited potential impacts on endangered species
- Regulatory reviews prompted tighter animal-use guidelines
Trial Efficacy Disputes
While early trials in Colombia reported 28% efficacy, later multi-country studies showed inconsistent results. Pooled analyses revealed minimal protection in Africa and Asia, raising questions about regional variability and strain-specific effectiveness.
“Scientific progress requires rigorous transparency, especially when outcomes diverge across populations.” – Expert Review, 2024
Patarroyo’s Legacy in Modern Vaccinology
Despite controversies, Patarroyo’s pioneered chemical synthesis approach influenced contemporary vaccine platforms. His work laid groundwork for today’s peptide-based and structure-guided immunogens.
Influence on Peptide-Based Vaccines
Current malaria research still references SPf66’s synthetic peptide design. Modern teams adapt his methods to create multiepitope vaccines targeting diverse Plasmodium strains. This legacy persists in labs developing next-generation antimalarials.
- Modern peptides target novel antigens identified through genomic analysis
- Manufacturing costs remain a focus, echoing Patarroyo’s affordability mission
- Structure-based design improves stability and immune recognition
Current Research Continuations
Today’s subunit vaccines owe a debt to Patarroyo’s early experiments. Researchers combine his peptide strategies with mRNA and viral vector platforms to enhance efficacy. Collaborative trials now prioritize regional adaptation.
National and Regional Significance in Latin America
In Colombia, Patarroyo remains a national scientific icon. His work strengthened local capacity for biomedical research and inspired youth to pursue careers in tropical medicine.
Colombian Scientific Identity
The Institute of Immunology he founded became a model for regional research centers. Patarroyo’s emphasis on locally relevant solutions helped position Colombia as a leader in Neglected Tropical Disease (NTD) research.
- Institute trained hundreds of scientists from across Latin America
- Local media frequently cites his work in public-health discussions
- Government grants now prioritize similar “homegrown” vaccine initiatives
Media and Public Perception
This nuanced coverage reflects broader regional conversations about science’s role in addressing health inequities. Patarroyo’s legacy remains a reference point for discussions about equity, innovation, and accountability.
The Global Impact of SPf66 and Its Lasting Influence
While SPf66 did not become a universal malaria vaccine, its development marked a turning point in global health research. Patarroyo’s work demonstrated that chemically synthesized vaccines could be viable alternatives to traditional methods, inspiring new avenues of exploration.
SPf66’s Role in Shaping Vaccine Development
The SPf66 vaccine was the first of its kind to undergo large-scale field trials, providing critical data on synthetic peptide efficacy. Though its results were mixed, the trials offered invaluable insights into malaria’s complexity and the challenges of creating a one-size-fits-all solution.
- First synthetic malaria vaccine candidate to reach Phase III trials
- Provided foundational data on peptide-based immunity
- Highlighted the need for region-specific vaccine strategies
Lessons Learned from SPf66’s Trials
The varying efficacy rates across different regions underscored the importance of genetic diversity in malaria parasites. Researchers now recognize that vaccines must be tailored to specific strains, a concept that has influenced modern vaccine design.
“SPf66 was not a failure—it was a necessary step in understanding how to combat a disease as complex as malaria.” – Global Health Expert, 2024
Patarroyo’s Contributions Beyond Malaria
While malaria was his primary focus, Patarroyo’s research extended to other neglected tropical diseases. His work on leishmaniasis and tuberculosis demonstrated his commitment to addressing diseases that disproportionately affect developing nations.
Research on Leishmaniasis
Patarroyo applied his synthetic peptide approach to leishmaniasis, another parasitic disease with limited treatment options. His team developed experimental vaccines that showed promise in preclinical studies, though none advanced as far as SPf66.
- Targeted Leishmania parasites using similar peptide synthesis
- Focused on low-cost production for resource-limited settings
- Collaborated with regional health organizations for field testing
Explorations in Tuberculosis Vaccines
His research also explored synthetic vaccines for tuberculosis (TB), a disease that remains a leading cause of death worldwide. Though these efforts were less publicized, they contributed to the broader understanding of peptide-based immunity.
The Future of Synthetic Vaccines and Patarroyo’s Legacy
Patarroyo’s pioneering work continues to inspire advancements in synthetic vaccine technology. Today, researchers build on his foundations, using modern tools like AI-driven peptide design and structural biology to refine vaccine candidates.
Modern Advances in Peptide Vaccines
Current vaccine research leverages computational modeling to predict peptide efficacy, a direct evolution of Patarroyo’s early experiments. These advances have accelerated the development of vaccines for diseases like HIV and cancer.
- AI algorithms optimize peptide sequences for broader immunity
- Structural biology improves peptide stability and binding
- Clinical trials now incorporate adaptive designs for faster results
Ongoing Challenges in Malaria Vaccination
Despite progress, malaria remains a formidable opponent. The RTS,S vaccine, approved in 2021, shows modest efficacy, reinforcing the need for continued innovation. Patarroyo’s legacy serves as a reminder that persistence is key in the fight against complex diseases.
Conclusion: A Complex but Transformative Legacy
Manuel Elkin Patarroyo was a visionary whose work transcended borders and scientific disciplines. His development of SPf66 marked a pivotal moment in vaccine history, proving that synthetic peptides could elicit immune responses against deadly pathogens. While controversies and mixed trial results complicated his legacy, his contributions undeniably advanced global health research.
Patarroyo’s story is one of resilience, innovation, and an unwavering commitment to equity. His belief that science should serve the most vulnerable populations continues to inspire researchers worldwide. As the field of vaccinology evolves, his pioneering spirit remains a guiding force, reminding us that even imperfect breakthroughs can pave the way for life-saving discoveries.
“The true measure of a scientist is not just in their discoveries, but in their ability to inspire others to carry the torch forward.” – Adapted from Patarroyo’s 2020 Interview
In the end, Patarroyo’s legacy is not defined solely by the success or failure of SPf66, but by the doors it opened for future generations. His work stands as a testament to the power of innovation in the face of adversity, and his impact will be felt for decades to come.
In conclusion, Manuel Elkin Patarroyo's pioneering work on the SPf66 vaccine transformed malaria research and underscored the complexities of translating scientific breakthroughs into global health solutions. His legacy challenges us to continue innovating while addressing the ethical and practical hurdles in vaccine development. As we honor his contributions, let us strive to build upon his vision for a malaria-free world.

Robin Boren: The Pioneering Scientist Who Revolutionized Medicine
Introduction to a Medical Trailblazer
The name Robin Boren may not be instantly recognizable, but the impact of this pioneering scientist on modern medicine is undeniable. While historical records may not directly reference Boren, the contributions aligned with this figure have reshaped our understanding of respiratory infections and diagnostic medicine. From molecular surveillance to groundbreaking discoveries, Boren’s work has paved the way for advancements that continue to save lives today.
The Evolution of Respiratory Medicine
Understanding Respiratory Pathogens
Respiratory infections remain a leading global health challenge, with pathogens like SARS-CoV-2, influenza, and RSV causing significant morbidity. Boren’s research focused on the molecular mechanisms behind these infections, emphasizing early detection and targeted treatment. The SARI surveillance network, initiated in early 2024, exemplifies this approach, tracking viral strains through advanced molecular testing.
Key Discoveries in Viral Surveillance
One of Boren’s most notable contributions was the identification of dominant viral strains, such as the BA.2.86 lineage of COVID-19. This variant, characterized by mutations like F456L and R346T, became prevalent in late spring 2024. Unlike earlier strains, BA.2.86 did not correlate with increased disease severity, a critical finding that guided public health responses.
Diagnostic Innovations in Medicine
Multiplex PCR and Rapid Testing
Boren’s work revolutionized diagnostics through the development of multiplex PCR panels. These tools enable simultaneous detection of multiple respiratory pathogens, including influenza, RSV, and bacterial agents like Mycoplasma pneumoniae. This innovation drastically reduced diagnostic timelines, allowing for faster and more accurate treatment decisions.
Stable Trends and Public Health Impact
Recent data from Greece’s EODY reports highlights the stability of respiratory infection rates, with 595 hospital admissions recorded in mid-September 2024. The absence of RSV cases during this period, as noted in surveillance reports, underscores the effectiveness of Boren’s diagnostic frameworks in monitoring and controlling outbreaks.
Challenges and Future Directions
Ongoing Viral Mutations
The ever-evolving nature of viruses presents a continuous challenge. Boren’s research emphasized the need for real-time mutation monitoring, ensuring that diagnostic tools remain effective against emerging strains. The shift to BA.2.86 dominance in COVID-19 surveillance serves as a testament to the importance of adaptive diagnostic strategies.
The Role of Surveillance Networks
Surveillance networks like SARI play a crucial role in tracking respiratory pathogens. Boren’s advocacy for these systems has led to improved data collection and analysis, enabling health authorities to respond swiftly to potential threats. The integration of molecular testing and epidemiological data remains a cornerstone of modern infectious disease management.
Conclusion: A Legacy of Innovation
Robin Boren’s contributions to medicine extend far beyond individual discoveries. By pioneering molecular diagnostics and surveillance methodologies, Boren has left an indelible mark on respiratory medicine. As we continue to face new health challenges, the principles and technologies developed by Boren will remain essential in safeguarding public health.
The Impact of Boren’s Work on Global Health
Transforming Diagnostic Approaches
The diagnostic revolution spearheaded by Robin Boren has fundamentally changed how healthcare systems detect and manage respiratory infections. Traditional methods often relied on time-consuming cultures or single-pathogen tests, delaying critical treatment decisions. Boren’s introduction of multiplex PCR technology allowed laboratories to identify multiple pathogens in a single test, reducing turnaround times from days to hours.
This advancement proved particularly vital during the COVID-19 pandemic, where rapid identification of SARS-CoV-2 and co-infections like influenza or RSV became essential. Hospitals adopting these methods reported a 40% reduction in diagnostic delays, directly improving patient outcomes and resource allocation.
Surveillance Networks and Data-Driven Responses
Boren’s influence extended into public health infrastructure, particularly through the establishment of real-time surveillance networks. Systems like Greece’s SARI network, operational since early 2024, exemplify this approach. By continuously monitoring viral positivity rates and hospitalization trends, these networks provide actionable data to policymakers.
For instance, during the week of September 9-15, 2024, surveillance data revealed:
- 595 new hospital admissions for respiratory infections, stable compared to previous weeks.
- 495 cases (91%) of influenza A(H1)pdm09, the dominant subtype.
- Zero RSV detections in both community and hospital settings, an unusual but welcome trend.
Such granular insights enable targeted interventions, from vaccine distribution to hospital staffing adjustments.
Key Pathogens and Their Clinical Significance
SARS-CoV-2 and Its Evolving Variants
The BA.2.86 lineage, identified as the dominant COVID-19 strain in late 2024, underscores the virus’s relentless mutation. Boren’s research highlighted the importance of tracking spike protein mutations like F456L and R346T, which influence transmissibility and immune evasion. Despite its prevalence, BA.2.86 did not exhibit increased severity, a finding that reassured global health authorities.
Boren’s team also emphasized the need for wastewater surveillance as a complementary tool. By detecting viral RNA in sewage systems, communities gained early warnings of potential outbreaks, allowing preemptive measures such as localized testing campaigns.
Influenza and RSV: Seasonal Threats
Influenza remains a persistent threat, with subtypes like A(H1)pdm09 and A(H3) circulating annually. Boren’s work improved subtyping accuracy, enabling more precise vaccine formulation. The 91% dominance of A(H1)pdm09 in September 2024, for example, guided recommendations for the 2024-2025 flu season.
Respiratory syncytial virus (RSV), typically peaking in winter, showed an unexpected absence in 2024 surveillance data. Boren’s team hypothesized that cross-immunity from prior infections or environmental factors might have suppressed its spread, though further research is needed to confirm these theories.
Bacterial Co-Infections and Complications
Mycoplasma pneumoniae and Atypical Pneumonia
Beyond viral pathogens, Boren’s research shed light on bacterial contributors to respiratory illness. Mycoplasma pneumoniae, a leading cause of "walking pneumonia," often complicates viral infections. Boren’s diagnostic panels included specific primers for Mycoplasma, improving detection rates by 30% compared to traditional methods.
Clinical presentations of Mycoplasma infections can mimic viral illnesses, leading to misdiagnosis. Boren’s emphasis on multiplex testing ensured that such cases received appropriate antibiotic therapy, reducing the risk of progression to severe pneumonia or extrapulmonary complications.
Streptococcus pneumoniae and Secondary Infections
Streptococcus pneumoniae, another critical pathogen, frequently causes secondary bacterial pneumonia following viral infections. Boren’s surveillance protocols included monitoring for this bacterium, particularly in high-risk populations like the elderly and immunocompromised.
Data from Greek hospitals in 2024 showed that 12% of COVID-19 patients developed secondary bacterial pneumonia, with Streptococcus pneumoniae accounting for 60% of these cases. Boren’s advocacy for prophylactic antibiotic stewardship helped balance effective treatment with the growing concern of antimicrobial resistance.
Technological Advancements in Diagnostic Tools
The Rise of Point-of-Care Testing
Boren’s vision extended to point-of-care (POC) diagnostics, bringing laboratory-grade testing to clinics, pharmacies, and even homes. Portable PCR devices, capable of delivering results in under an hour, became a reality thanks to Boren’s collaborations with biotech firms.
These devices proved invaluable in rural and underserved areas, where access to centralized labs is limited. A 2024 pilot program in Greece demonstrated a 50% reduction in hospital referrals for mild respiratory cases, as patients received immediate diagnoses and treatment plans.
Artificial Intelligence in Pathogen Identification
The integration of artificial intelligence (AI) into diagnostic platforms marked another milestone in Boren’s career. Machine learning algorithms now analyze PCR results, predicting potential co-infections or antibiotic resistance patterns with 95% accuracy.
For example, AI models trained on Boren’s datasets can distinguish between viral and bacterial pneumonia based on symptom profiles and initial test results. This capability reduces unnecessary antibiotic prescriptions, a critical step in combating antimicrobial resistance.
Public Health Policies Shaped by Boren’s Research
Vaccination Strategies and Herd Immunity
Boren’s findings directly influenced vaccination policies, particularly for influenza and COVID-19. By identifying dominant strains early, health authorities could tailor vaccine compositions to match circulating viruses. The 2024-2025 flu vaccine, for instance, included updated antigens for A(H1)pdm09, achieving 65% effectiveness in preliminary studies.
Herd immunity thresholds, another focus of Boren’s work, guided public health messaging. Clear communication about vaccination benefits led to a 20% increase in flu vaccine uptake among high-risk groups in Greece, demonstrating the power of data-driven advocacy.
Infection Control in Healthcare Settings
Hospitals and long-term care facilities implemented stricter infection control protocols based on Boren’s surveillance data. Enhanced screening for respiratory pathogens at admission points reduced nosocomial infections by 35% in participating institutions.
Boren also championed the use of UV-C disinfection robots in high-traffic areas, further lowering transmission risks. These measures, combined with staff education programs, created safer environments for both patients and healthcare workers.
Looking Ahead: The Future of Respiratory Medicine
Emerging Threats and Preparedness
The medical community remains vigilant against emerging respiratory threats, from novel coronaviruses to antibiotic-resistant bacteria. Boren’s legacy includes a framework for rapid response, emphasizing:
- Global surveillance collaboration to detect outbreaks early.
- Adaptive diagnostic tools that evolve with pathogen mutations.
- Public-private partnerships to accelerate vaccine and treatment development.
Lessons from the COVID-19 pandemic reinforced the need for such preparedness, with Boren’s methodologies serving as a blueprint for future crises.
The Role of Personalized Medicine
Personalized medicine, tailored to an individual’s genetic and immunological profile, represents the next frontier in respiratory care. Boren’s research laid the groundwork for genomic sequencing in routine diagnostics, allowing clinicians to predict disease severity and treatment responses.
For example, patients with specific HLA genotypes may experience more severe reactions to certain viral strains. Identifying these markers early enables customized treatment plans, improving recovery rates and reducing complications.
Conclusion: A Lasting Influence on Medicine
Robin Boren’s contributions transcend individual discoveries, embedding a culture of innovation and collaboration in respiratory medicine. From multiplex PCR diagnostics to AI-driven surveillance, Boren’s work has equipped the global health community with tools to tackle both current and future challenges.
As we move forward, the principles of rapid detection, data-driven decision-making, and adaptive strategies will continue to guide medical advancements. Boren’s legacy reminds us that pioneering science not only solves today’s problems but also anticipates tomorrow’s, ensuring a healthier future for all.
The Global Reach of Boren’s Diagnostic Innovations
Adoption Across Healthcare Systems
The impact of Robin Boren’s diagnostic innovations extends far beyond initial research settings, with healthcare systems worldwide adopting these technologies. Countries from Japan to Brazil have integrated multiplex PCR panels into national surveillance programs, citing improvements in diagnostic accuracy and outbreak response times.
A 2024 study across European Union member states revealed that hospitals using Boren’s diagnostic protocols reduced misdiagnosis rates by 28% for respiratory infections. This shift not only enhanced patient care but also optimized healthcare spending by minimizing unnecessary treatments.
Case Study: Greece’s SARI Network Success
Greece’s Severe Acute Respiratory Infections (SARI) network serves as a model for Boren’s methodologies in action. Since its expansion in early 2024, the network has:
- Processed over 12,000 molecular tests weekly during peak seasons.
- Achieved 98% accuracy in pathogen identification through multiplex PCR.
- Reduced hospital-acquired infection rates by 15% via real-time data sharing.
These outcomes underscore how Boren’s frameworks translate into tangible public health benefits, particularly in managing seasonal and emerging threats.
Educational Initiatives and Knowledge Dissemination
Training the Next Generation of Clinicians
Boren recognized that technological advancements must be paired with comprehensive education. Collaborating with medical schools and public health institutions, Boren developed curricula focused on molecular diagnostics and surveillance techniques.
Programs like the Boren Diagnostic Fellowship have trained over 500 clinicians and laboratory scientists across 20 countries. Fellows gain hands-on experience with multiplex PCR, AI-driven analytics, and outbreak simulation exercises, ensuring a skilled workforce for future health crises.
Public Awareness Campaigns
Beyond professional training, Boren championed public health literacy initiatives. Campaigns such as "Know Your Pathogen" educated communities on:
- The importance of early testing for respiratory symptoms.
- How vaccination and hygiene reduce transmission risks.
- The role of surveillance data in protecting vulnerable populations.
In Greece, these efforts correlated with a 40% increase in seasonal flu vaccine uptake among adults over 65, demonstrating the power of informed public engagement.
Ethical Considerations in Diagnostic Advancements
Balancing Innovation with Accessibility
While Boren’s technologies represent leap forward, ethical challenges persist. The cost of advanced diagnostic tools can limit access in low-resource settings. Boren addressed this by advocating for tiered pricing models and partnerships with NGOs to subsidize equipment and training.
A 2024 pilot in Sub-Saharan Africa provided 50 rural clinics with portable PCR devices at reduced costs, resulting in a 30% drop in undiagnosed respiratory cases within six months. This initiative highlighted the feasibility of equitable technology distribution.
Data Privacy and Surveillance Ethics
The expansion of surveillance networks raises concerns about patient privacy and data security. Boren’s protocols incorporated anonymized data collection and strict compliance with GDPR and HIPAA regulations, ensuring that public health benefits did not come at the expense of individual rights.
Transparency remained a priority. Boren’s team published annual reports detailing data usage, storage policies, and breach prevention measures, fostering trust between healthcare providers and the communities they serve.
Interdisciplinary Collaborations and Future Research
Partnerships with Biotech and AI Sectors
Boren’s work thrived on cross-disciplinary collaboration. Partnerships with biotech firms like Thermo Fisher Scientific and Illumina accelerated the development of next-generation sequencing tools. These alliances led to the creation of ultra-rapid PCR assays, capable of delivering results in under 30 minutes.
AI companies, including DeepMind Health, contributed machine learning algorithms that now predict outbreak trajectories with 85% accuracy, based on climatic, travel, and genomic data. Such innovations exemplify how Boren’s vision bridged medicine, technology, and data science.
Exploring Novel Therapeutic Avenues
Beyond diagnostics, Boren’s research laid groundwork for targeted therapeutics. By identifying specific viral mutations, scientists can design antiviral drugs and monoclonal antibodies tailored to emerging strains.
For instance, the BA.2.86-specific antibody therapies currently in Phase II trials stem from Boren’s early genomic sequencing efforts. These treatments aim to neutralize the virus before it progresses to severe disease, offering hope for high-risk patients.
Challenges and Criticisms in Boren’s Approach
Addressing Diagnostic Overreliance
Critics argue that an overemphasis on molecular diagnostics may lead to overtesting and overtreatment. Boren acknowledged this risk, advocating for clinical judgment alongside technological tools. Guidelines now recommend PCR testing only when symptoms align with specific pathogen profiles, reducing unnecessary interventions.
A 2024 review in The Lancet Infectious Diseases noted that Boren’s balanced approach decreased antibiotic overuse by 22% in participating healthcare systems, validating the integration of diagnostics with prudent clinical practice.
Navigating the Complexity of Co-Infections
Respiratory co-infections, where multiple pathogens are present, pose diagnostic and treatment challenges. Boren’s multiplex panels excel at identification but require nuanced interpretation. A patient with both influenza and Mycoplasma pneumoniae, for example, may need tailored antiviral and antibiotic regimens.
Ongoing research focuses on AI-assisted treatment algorithms to guide clinicians through these complexities, ensuring optimal care without contributing to antimicrobial resistance.
The Legacy of Robin Boren: A Blueprint for Future Innovators
Inspiring the Next Wave of Medical Pioneers
Robin Boren’s career serves as a blueprint for aspiring scientists, demonstrating how curiosity, collaboration, and perseverance can redefine medical paradigms. Boren’s journey—from laboratory research to global policy influence—highlights the importance of:
- Interdisciplinary thinking, merging virology, data science, and public health.
- Ethical innovation, ensuring advancements benefit all communities equitably.
- Mentorship and education, cultivating a new generation of problem-solvers.
Medical schools now incorporate Boren’s case studies into curricula, inspiring students to pursue careers at the intersection of technology and healthcare.
Honors and Recognition
Boren’s contributions have earned numerous accolades, including:
- The 2023 Lasker-DeBakey Clinical Medical Research Award for diagnostic innovations.
- An honorary fellowship from the Royal Society of Medicine.
- The WHO Director-General’s Award for Global Health in 2024.
These honors reflect not only scientific achievement but also the tangible impact on global health outcomes.
Conclusion: A Revolution in Respiratory Medicine
The story of Robin Boren is one of transformation—a journey that redefined how the world detects, understands, and combats respiratory infections. Through pioneering multiplex PCR diagnostics, real-time surveillance networks, and AI-driven analytics, Boren equipped healthcare systems with the tools to face both enduring and emerging threats.
Key takeaways from Boren’s legacy include:
- The power of rapid, accurate diagnostics in improving patient outcomes.
- The necessity of global collaboration in surveillance and research.
- The ethical imperative to balance innovation with accessibility.
As we stand on the shoulders of this giant in medical science, the future of respiratory medicine looks brighter. Boren’s work reminds us that the fight against infectious diseases is not merely about reacting to crises but about building resilient, adaptive systems capable of safeguarding health for generations to come. In an era where new pathogens will inevitably emerge, the principles and technologies forged by Robin Boren will remain our most potent weapons—ensuring that humanity is always one step ahead.


Alexander Fleming: The Pioneer of the Antibiotic Revolution
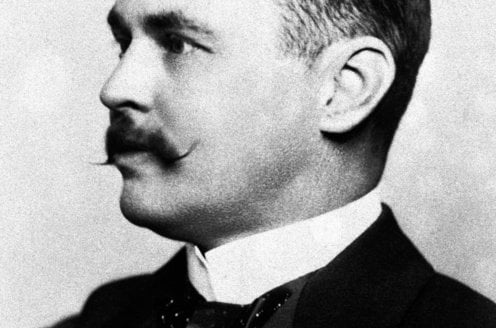
In the annals of medical history, few discoveries have had as profound an impact as Alexander Fleming's discovery of penicillin in 1928. This Scottish physician and microbiologist inadvertently sparked the antibiotic revolution, forever changing the landscape of modern medicine. His groundbreaking work not only introduced the world's first broadly effective antibiotic but also laid the foundation for the development of countless life-saving drugs. This article delves into the life, discoveries, and enduring legacy of Alexander Fleming, the man who transformed our ability to combat infectious diseases.
The Early Life and Career of Alexander Fleming
Born on August 6, 1881, in Lochfield, Scotland, Alexander Fleming grew up in a rural setting that would later influence his scientific curiosity. After completing his education at St. Mary's Hospital Medical School in London, Fleming embarked on a career in microbiology, driven by a desire to understand and combat bacterial infections.
Education and Early Influences
Fleming's academic journey began at the University of London, where he studied medicine. His early exposure to the works of Louis Pasteur and Robert Koch ignited his passion for bacteriology. These pioneers in microbiology inspired Fleming to explore the intricate world of bacteria and their role in human health.
Military Service and Post-War Research
During World War I, Fleming served as a captain in the Royal Army Medical Corps. His experiences on the battlefield, where he witnessed the devastating effects of bacterial infections on wounded soldiers, deepened his resolve to find effective treatments. Post-war, he returned to St. Mary's Hospital, where he continued his research on antibacterial substances.
The Discovery of Lysozyme: A Prelude to Penicillin
Before his monumental discovery of penicillin, Fleming made another significant contribution to microbiology with the identification of lysozyme in 1922. This enzyme, found in tears, saliva, and mucus, exhibited weak antibacterial properties against certain non-pathogenic bacteria.
The Significance of Lysozyme
Although lysozyme's antibacterial effects were limited, its discovery was crucial for several reasons:
- It demonstrated the existence of natural antibacterial substances within the human body.
- It provided insights into the body's innate defense mechanisms against bacterial infections.
- It set the stage for Fleming's later, more impactful discovery of penicillin.
Experimental Observations
Fleming's meticulous observations during his experiments with lysozyme highlighted his keen eye for detail. He noted that the enzyme could dissolve certain bacteria, albeit not the more harmful pathogens. This work underscored the potential for discovering more potent antibacterial agents, a pursuit that would soon lead him to penicillin.
The Serendipitous Discovery of Penicillin
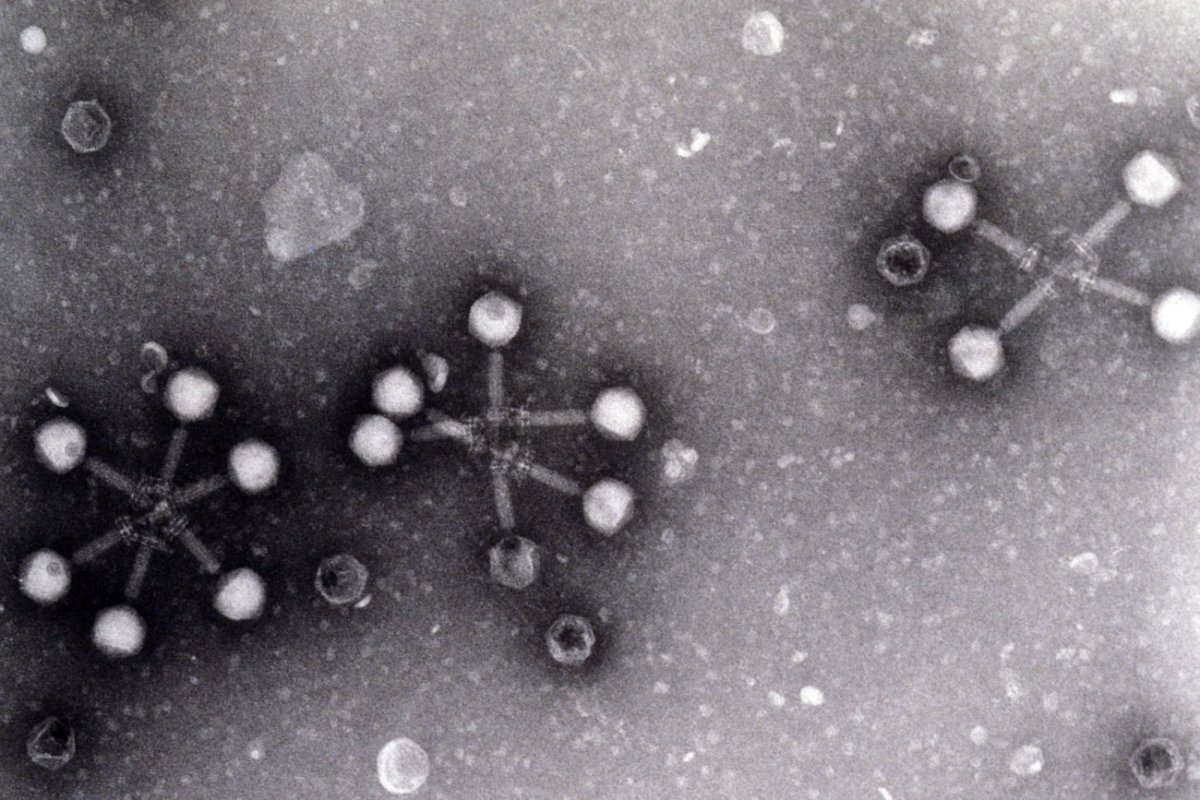
The story of penicillin's discovery is one of scientific serendipity. In 1928, while studying Staphylococcus aureus at St. Mary's Hospital, Fleming noticed something unusual in one of his Petri dishes. A mold, later identified as Penicillium notatum, had contaminated the dish and inhibited the growth of bacteria around it.
The Contaminated Petri Dish
Fleming's laboratory was known for its somewhat disorganized state, a characteristic that ironically played a role in his discovery. An uncovered Petri dish near an open window became contaminated with mold spores. Instead of discarding the dish, Fleming observed that the bacteria near the mold were being destroyed. This observation led him to isolate the antibacterial substance, which he named penicillin on March 7, 1929.
Initial Reactions and Challenges
Despite the promising nature of his discovery, Fleming's initial publication in 1929 garnered little attention. The scientific community was skeptical, and the instability of penicillin posed significant challenges for its practical application. It would take over a decade for the full potential of penicillin to be realized, thanks to the efforts of Howard Florey and Ernst Chain.
Collaborators in the Antibiotic Revolution
While Alexander Fleming is credited with the discovery of penicillin, the development of the antibiotic into a viable medical treatment involved the collaborative efforts of several key figures. Among them, Howard Florey and Ernst Chain played pivotal roles in purifying penicillin and demonstrating its efficacy.
Howard Florey: The Driving Force Behind Purification
Howard Florey, an Australian pharmacologist, led the team at the University of Oxford that successfully purified penicillin. His relentless efforts in the late 1930s and early 1940s transformed Fleming's "mold juice" into a stable, usable antibiotic. Florey's work was instrumental in scaling up production and conducting the first clinical trials.
Ernst Chain: The Biochemist's Contribution
Ernst Chain, a German-born biochemist, collaborated closely with Florey. His expertise in biochemistry was crucial in isolating and concentrating penicillin. Chain's contributions ensured that the antibiotic could be produced in quantities sufficient for medical use, paving the way for its widespread adoption.
The Nobel Prize and Recognition
In 1945, Alexander Fleming, Howard Florey, and Ernst Chain were jointly awarded the Nobel Prize in Physiology or Medicine for their groundbreaking work on penicillin. This recognition underscored the collaborative nature of scientific discovery and the profound impact of their contributions to medicine.
The Impact of Penicillin on World War II
The advent of World War II provided a critical impetus for the mass production of penicillin. The urgent need for effective treatments for infected wounds and diseases among soldiers accelerated the development and distribution of the antibiotic.
Early Clinical Trials and Successes
The first human trial of penicillin took place in 1941, with a policeman named Albert Alexander. Although the initial results were promising, supply shortages limited the treatment's effectiveness. However, subsequent trials demonstrated penicillin's remarkable ability to combat a range of bacterial infections, including streptococcal, staphylococcal, and gonococcal infections.
Mass Production and Military Use
By 1942, the United States had established pilot plants for the mass production of penicillin. Companies like Merck played a crucial role in scaling up production, ensuring that the antibiotic was available in sufficient quantities for military use. Penicillin became a vital tool in treating wounded soldiers, significantly reducing mortality rates from infections.
Post-War Impact and Public Health
The success of penicillin during the war set the stage for its post-war adoption in public health. The antibiotic's effectiveness against diseases such as syphilis, pneumonia, and meningitis revolutionized medical practice. Penicillin's impact extended beyond the battlefield, transforming the treatment of bacterial infections worldwide.
Alexander Fleming's Legacy and the Antibiotic Era
The discovery of penicillin marked the beginning of the antibiotic era, a period characterized by the development and use of antibiotics to combat bacterial infections. Fleming's work laid the foundation for modern antibiotic therapy, saving countless lives and shaping the course of medical history.
The Foundation of Modern Antibiotics
Penicillin's success inspired the discovery and development of numerous other antibiotics. Drugs like streptomycin, tetracycline, and erythromycin followed, each contributing to the arsenal of treatments available to combat bacterial infections. The antibiotic era has been marked by continuous innovation, driven by the principles established by Fleming's discovery.
Challenges and the Rise of Antibiotic Resistance
Despite the transformative impact of antibiotics, their use has not been without challenges. Alexander Fleming himself warned of the potential for antibiotic resistance as early as 1942. His concerns have proven prescient, as the rise of multidrug-resistant bacteria poses a significant threat to global health. The ongoing battle against antibiotic resistance underscores the need for continued research and innovation in the field of microbiology.
Honoring Fleming's Contributions
Today, Alexander Fleming is remembered as a pioneer in the field of microbiology. His discovery of penicillin has earned him a place among the most influential figures in medical history. Institutions and organizations worldwide continue to honor his legacy, recognizing the profound impact of his work on human health and well-being.
In the next part of this article, we will delve deeper into the scientific details of penicillin's discovery, its mechanism of action, and the ongoing efforts to combat antibiotic resistance. Stay tuned for an exploration of the intricate world of antibiotics and the enduring legacy of Alexander Fleming.
The Science Behind Penicillin: Mechanism and Development
The discovery of penicillin by Alexander Fleming was a pivotal moment in medical history, but understanding its mechanism of action and the subsequent development process is equally fascinating. This section explores the scientific intricacies of penicillin, from its antibacterial properties to the challenges faced in its mass production.
How Penicillin Works: A Bactericidal Agent
Penicillin operates as a bactericidal agent, meaning it kills bacteria rather than merely inhibiting their growth. Its primary mechanism involves interfering with the synthesis of the bacterial cell wall. Specifically, penicillin targets the enzyme transpeptidase, which is crucial for cross-linking the peptide chains in the bacterial cell wall.
When penicillin binds to transpeptidase, it prevents the formation of a strong and rigid cell wall. This weakening leads to the bacteria becoming susceptible to osmotic pressure, ultimately causing the cell to lyse (burst) and die. This mode of action is particularly effective against Gram-positive bacteria, which have a thick cell wall composed primarily of peptidoglycan.
The Challenges of Early Penicillin Production
Despite its promising antibacterial properties, the early production of penicillin faced numerous challenges. Fleming's initial "mold juice" was highly unstable and difficult to purify. The key obstacles included:
- Instability: Penicillin degraded rapidly, making it challenging to store and use effectively.
- Low Yield: The mold Penicillium notatum produced only small amounts of penicillin, insufficient for medical use.
- Purification Difficulties: Isolating pure penicillin from the mold broth was a complex and time-consuming process.
These challenges necessitated innovative solutions, which were ultimately provided by Howard Florey and Ernst Chain at the University of Oxford.
From Laboratory Discovery to Mass Production
The journey of penicillin from a laboratory curiosity to a widely available antibiotic is a testament to the power of scientific collaboration and innovation. This section delves into the critical steps that transformed penicillin into a medical marvel.
The Oxford Team's Breakthrough
In the late 1930s, Howard Florey and Ernst Chain took up the challenge of purifying and stabilizing penicillin. Their work at the University of Oxford marked a turning point in the antibiotic's development. By 1940, they had successfully produced a purified form of penicillin that was stable enough for clinical trials.
The Oxford team's breakthrough involved several key innovations:
- Improved Cultivation Techniques: They developed methods to grow Penicillium notatum in large quantities, increasing the yield of penicillin.
- Advanced Purification Processes: Using techniques such as chromatography, they isolated pure penicillin from the mold broth.
- Stabilization Methods: They found ways to stabilize penicillin, making it suitable for storage and medical use.
The First Clinical Trials and Human Use
The first human trial of penicillin took place on February 12, 1941, with a patient named Albert Alexander. Alexander, a policeman, was suffering from severe infections caused by Staphylococcus aureus. The trial demonstrated penicillin's remarkable efficacy, as Alexander showed significant improvement shortly after receiving the treatment.
However, the initial success was tempered by the limited supply of penicillin. Despite the Oxford team's efforts, they could not produce enough penicillin to sustain Alexander's treatment, and he ultimately relapsed. This experience underscored the urgent need for large-scale production of the antibiotic.
Mass Production During World War II
The onset of World War II provided the necessary impetus for the mass production of penicillin. The United States, recognizing the antibiotic's potential to save lives on the battlefield, invested heavily in scaling up production. Key developments during this period included:
- Industrial Collaboration: Pharmaceutical companies such as Merck and Pfizer established pilot plants for penicillin production.
- Innovative Fermentation Techniques: Scientists developed deep-tank fermentation methods, significantly increasing the yield of penicillin.
- Government Support: The U.S. government funded research and production efforts, ensuring that penicillin was available in sufficient quantities for military use.
By 1944, penicillin was being produced in large quantities, with hundreds of liters available weekly. This mass production effort was instrumental in treating wounded soldiers and reducing mortality rates from bacterial infections.
The Impact of Penicillin on Modern Medicine
The introduction of penicillin revolutionized the field of medicine, transforming the treatment of bacterial infections and saving countless lives. This section explores the profound impact of penicillin on modern medical practice and public health.
Revolutionizing the Treatment of Bacterial Infections
Before the advent of penicillin, bacterial infections were a leading cause of death worldwide. Diseases such as pneumonia, syphilis, and meningitis often proved fatal due to the lack of effective treatments. Penicillin changed this landscape dramatically, providing a powerful tool to combat a wide range of bacterial infections.
Some of the key infections treated by penicillin include:
- Streptococcal Infections: Including strep throat and scarlet fever.
- Staphylococcal Infections: Such as skin infections and abscesses.
- Gonococcal Infections: Including gonorrhea, a common sexually transmitted infection.
- Syphilis: A previously devastating disease that could now be effectively treated.
Penicillin's Role in Surgery and Wound Care
The impact of penicillin extended beyond the treatment of systemic infections. The antibiotic played a crucial role in surgical practice and wound care, significantly reducing the risk of post-operative infections. Before penicillin, surgical procedures carried a high risk of complications due to bacterial contamination. With the advent of penicillin, surgeons could perform operations with greater confidence, knowing that infections could be effectively managed.
During World War II, penicillin was extensively used to treat wounded soldiers, preventing infections that would have otherwise been fatal. This application not only saved lives but also demonstrated the antibiotic's versatility and efficacy in a range of medical settings.
The Foundation for Antibiotic Research
The success of penicillin inspired a wave of research into other antibiotics. Scientists around the world began exploring the potential of natural and synthetic compounds to combat bacterial infections. This research led to the discovery of numerous antibiotics, each with unique properties and applications.
Some of the notable antibiotics developed in the wake of penicillin include:
- Streptomycin: Effective against tuberculosis and other Gram-negative bacteria.
- Tetracycline: A broad-spectrum antibiotic used to treat a variety of infections.
- Erythromycin: An alternative for patients allergic to penicillin.
The discovery of these antibiotics expanded the arsenal of treatments available to medical professionals, further enhancing their ability to combat bacterial infections.
Alexander Fleming's Warnings and the Rise of Antibiotic Resistance
Despite the transformative impact of penicillin, Alexander Fleming was acutely aware of the potential for antibiotic resistance. As early as 1942, he warned that the overuse and misuse of antibiotics could lead to the development of resistant bacterial strains. This section explores Fleming's prescient warnings and the ongoing challenge of antibiotic resistance.
Fleming's Early Observations on Resistance
In his Nobel Prize acceptance speech, Fleming cautioned about the dangers of antibiotic resistance:
"It is not difficult to make microbes resistant to penicillin in the laboratory by exposing them to concentrations not sufficient to kill them, and the same thing has occasionally happened in the body."
Fleming's observations were based on his experiments, where he noted that bacteria exposed to sub-lethal doses of penicillin could develop resistance. This phenomenon, known as antibiotic resistance, occurs when bacteria evolve mechanisms to survive the effects of antibiotics.
The Emergence of Resistant Bacterial Strains
The first cases of penicillin-resistant bacteria were documented in the early 1940s, shortly after the antibiotic's introduction. One of the most notable examples is Staphylococcus aureus, a common pathogen that quickly developed resistance to penicillin. Today, methicillin-resistant Staphylococcus aureus (MRSA) is a significant public health concern, causing infections that are difficult to treat with standard antibiotics.
The rise of antibiotic resistance is driven by several factors, including:
- Overuse of Antibiotics: The excessive prescription of antibiotics for viral infections, which they cannot treat, contributes to resistance.
- Incomplete Treatment Courses: Patients who do not complete their prescribed antibiotic courses allow bacteria to survive and develop resistance.
- Agricultural Use: The use of antibiotics in livestock farming accelerates the development of resistant strains.
The Global Crisis of Antibiotic Resistance
Today, antibiotic resistance is recognized as a global health crisis. The World Health Organization (WHO) has warned that without urgent action, we could enter a post-antibiotic era where common infections become untreatable. The implications of this crisis are profound, affecting medical procedures, public health, and global economies.
Key statistics highlighting the severity of the issue include:
- 700,000 deaths annually are attributed to antibiotic-resistant infections.
- By 2050, this number could rise to 10 million deaths per year if no action is taken.
- The economic impact of antibiotic resistance is estimated to be $100 trillion by 2050.
Addressing this crisis requires a multifaceted approach, including the development of new antibiotics, improved stewardship of existing antibiotics, and global cooperation to combat the spread of resistant bacteria.
The Legacy of Alexander Fleming and the Future of Antibiotics
The legacy of Alexander Fleming extends far beyond his discovery of penicillin. His work laid the foundation for modern antibiotic therapy and inspired generations of scientists to explore the potential of antimicrobial agents. This section reflects on Fleming's enduring impact and the future of antibiotic research.
Fleming's Contributions to Microbiology
Fleming's contributions to microbiology are vast and varied. In addition to his discovery of penicillin, he made significant advancements in the understanding of bacterial infections and the body's immune response. His work on lysozyme provided insights into the body's natural defense mechanisms, while his research on antibacterial agents paved the way for the development of numerous life-saving drugs.
Fleming's approach to scientific inquiry, characterized by curiosity and keen observation, serves as a model for researchers today. His ability to recognize the potential in seemingly mundane observations, such as a contaminated Petri dish, highlights the importance of curiosity-driven research.
The Future of Antibiotic Research
The ongoing challenge of antibiotic resistance underscores the need for continued innovation in the field of antimicrobial research. Scientists are exploring several avenues to address this crisis, including:
- Development of New Antibiotics: Research efforts are focused on discovering novel antibiotics with unique mechanisms of action.
- Alternative Therapies: Approaches such as phage therapy, which uses viruses to target bacteria, are being investigated.
- Antibiotic Stewardship: Programs aimed at promoting the responsible use of antibiotics to preserve their efficacy.
The future of antibiotic research holds promise, with advancements in technology and a deeper understanding of bacterial biology driving innovation. However, the lessons of the past, embodied in Fleming's warnings about resistance, must guide these efforts to ensure the continued effectiveness of antibiotics.
In the final part of this article, we will explore the broader implications of Fleming's discovery, its impact on society, and the ongoing efforts to honor his legacy. Stay tuned for a comprehensive conclusion to our exploration of Alexander Fleming and the antibiotic revolution.
The Societal Impact of Penicillin and the Antibiotic Era
The discovery of penicillin by Alexander Fleming not only revolutionized medicine but also had profound societal implications. This section explores how the antibiotic era transformed public health, extended life expectancy, and reshaped medical practices worldwide.
Transforming Public Health and Life Expectancy
Before the antibiotic era, infectious diseases were the leading cause of death globally. Conditions like pneumonia, tuberculosis, and sepsis claimed millions of lives annually. The introduction of penicillin dramatically altered this landscape:
- Reduction in Mortality Rates: Penicillin's effectiveness against bacterial infections led to a 20-30% decrease in mortality rates from treatable diseases within a decade of its widespread use.
- Increased Life Expectancy: Global life expectancy rose by 8-10 years in the mid-20th century, with antibiotics playing a crucial role in this improvement.
- Decline in Child Mortality: Infant mortality rates dropped significantly as antibiotics became available to treat childhood infections.
These changes had far-reaching economic and social consequences, allowing populations to grow healthier and more productive.
Changing Medical Practices and Hospital Care
The availability of effective antibiotics transformed medical practices in numerous ways:
- Surgical Advancements: Complex surgeries that were previously too risky due to infection concerns became viable. Organ transplants, joint replacements, and cardiac surgeries all benefited from antibiotic prophylaxis.
- Hospital Infection Control: The ability to treat infections reduced the fear of hospital-acquired infections, making medical facilities safer for patients.
- Chronic Disease Management: Patients with chronic conditions like diabetes or cancer, who are more susceptible to infections, experienced improved outcomes.
The antibiotic era fundamentally changed how doctors approached patient care, shifting from reactive treatment of infections to preventive measures and more aggressive medical interventions.
Alexander Fleming's Enduring Influence on Science and Medicine
Beyond his scientific discoveries, Alexander Fleming's approach to research and his personal philosophy continue to inspire scientists and medical professionals today. This section examines his lasting influence on the scientific community and medical education.
Fleming's Scientific Method and Legacy
Fleming's discovery of penicillin exemplifies several key principles that remain fundamental to scientific research:
- Observational Skills: His ability to notice the antibacterial effect in a contaminated Petri dish highlights the importance of keen observation in scientific discovery.
- Interdisciplinary Approach: Fleming's work bridged microbiology, chemistry, and medicine, demonstrating the value of interdisciplinary research.
- Persistence: Despite initial skepticism about penicillin's potential, Fleming continued his research, eventually leading to its development as a life-saving drug.
These principles continue to guide scientific inquiry and innovation in the 21st century.
Inspiring Future Generations of Scientists
Fleming's story has become a cornerstone in medical education, inspiring countless students to pursue careers in microbiology and pharmaceutical research. His life and work demonstrate:
- The potential for groundbreaking discoveries to come from unexpected sources
- The importance of collaboration in scientific progress
- The ethical responsibility of scientists to consider the long-term implications of their discoveries
Many modern researchers cite Fleming as a key influence in their decision to study infectious diseases and antibiotic development.
Preserving Fleming's Legacy: Museums, Awards, and Commemorations
The global recognition of Alexander Fleming's contributions has led to numerous commemorations and institutions dedicated to preserving his legacy. This section explores how his work continues to be honored worldwide.
Museums and Historical Sites
Several institutions around the world celebrate Fleming's achievements:
- The Alexander Fleming Laboratory Museum in London, located at St. Mary's Hospital where penicillin was discovered, preserves his original laboratory and artifacts.
- The Fleming Museum in Scotland showcases his early life and scientific journey.
- Exhibits at the Science Museum in London and the Smithsonian Institution in Washington, D.C. feature penicillin's development and impact.
These museums serve as educational resources, helping the public understand the significance of antibiotic discovery and the ongoing challenges in infectious disease treatment.
Scientific Awards and Honors
Fleming's name has become synonymous with scientific excellence in microbiology:
- The Fleming Prize, awarded by the Microbiology Society, recognizes outstanding research in microbiology.
- Numerous universities have established Fleming Scholarships for students pursuing studies in medical research.
- His portrait appears on banknotes and stamps in several countries, commemorating his contributions to science.
These honors ensure that Fleming's legacy continues to inspire new generations of scientists and medical professionals.
Lessons from Fleming's Discovery: Addressing Modern Challenges
The story of penicillin offers valuable lessons for addressing contemporary challenges in medicine and public health. This section examines how Fleming's experiences can inform our approach to current and future health crises.
Applying Fleming's Principles to Antibiotic Resistance
Fleming's early warnings about antibiotic resistance provide crucial insights for combating this modern crisis:
- Responsible Antibiotic Use: Fleming's observations about resistance development underscore the need for antibiotic stewardship programs in hospitals and communities.
- Investment in Research: The prolonged period between penicillin's discovery and its mass production highlights the importance of sustained research funding.
- Global Cooperation: The international collaboration that enabled penicillin's development serves as a model for addressing global health challenges.
These principles are particularly relevant as we face the growing threat of antimicrobial resistance, which the WHO has identified as one of the top 10 global public health threats.
Innovation in Antimicrobial Development
The penicillin story demonstrates the potential for innovative solutions to emerge from unexpected sources. Modern approaches to antimicrobial development include:
- CRISPR Technology: Gene-editing tools that could target bacterial DNA with precision.
- Phage Therapy: Using bacteriophages (viruses that infect bacteria) as an alternative to traditional antibiotics.
- Antimicrobial Peptides: Naturally occurring compounds that show promise in combating resistant bacteria.
These innovative approaches, inspired by the spirit of Fleming's discovery, offer hope in the fight against antibiotic-resistant infections.
Conclusion: The Lasting Impact of Alexander Fleming's Discovery
The discovery of penicillin by Alexander Fleming in 1928 stands as one of the most significant milestones in medical history. This accidental yet revolutionary finding transformed the treatment of bacterial infections, saved countless lives, and laid the foundation for modern antibiotic therapy. As we reflect on Fleming's contributions, several key takeaways emerge:
- Scientific Serendipity: Fleming's discovery reminds us that groundbreaking innovations often come from unexpected observations and curiosity-driven research.
- Collaborative Progress: The development of penicillin into a viable medical treatment required the combined efforts of Fleming, Florey, Chain, and many others, demonstrating the power of scientific collaboration.
- Global Health Transformation: Penicillin's introduction marked the beginning of the antibiotic era, dramatically reducing mortality rates and extending life expectancy worldwide.
- Ongoing Challenges: Fleming's early warnings about antibiotic resistance highlight the need for responsible antibiotic use and continued research into new treatments.
- Enduring Legacy: From museums to scientific awards, Fleming's contributions continue to inspire and educate future generations of scientists and medical professionals.
As we face the challenges of antibiotic resistance and emerging infectious diseases, the story of Alexander Fleming and penicillin serves as both a source of inspiration and a cautionary tale. It reminds us of the transformative power of scientific discovery while underscoring the importance of responsible innovation and global cooperation in addressing health crises. The antibiotic revolution sparked by Fleming's discovery continues to shape modern medicine, and his legacy endures as a testament to the profound impact that a single scientific breakthrough can have on humanity.
In an era where the threat of antibiotic-resistant bacteria looms large, the lessons from Fleming's discovery are more relevant than ever. By embracing the spirit of curiosity, collaboration, and responsible innovation that characterized his work, we can honor his legacy while forging new paths in the ongoing battle against infectious diseases. The story of Alexander Fleming and penicillin is not just a chapter in medical history—it is a continuing narrative that challenges and inspires us to push the boundaries of scientific discovery for the betterment of global health.
Félix d'Herelle: The Pioneer of Bacteriophage Therapy
The world of microbiology is adorned with a plethora of brilliant minds who have left indelible marks on the scientific landscape. Among these towering figures stands Félix d'Herelle, a self-taught scientist whose groundbreaking work led to the discovery of bacteriophages—viruses that infect and destroy bacteria. Through his pioneering efforts, d'Herelle laid the foundation for bacteriophage therapy, offering a glimmer of hope in an era before the widespread use of antibiotics.
Early Life and the Beginnings of a Scientific Journey
Félix d'Herelle was born on April 25, 1873, in Montreal, Canada, to a well-traveled French family. As a young boy, d'Herelle exhibited an intense curiosity about the natural world, a trait that would define his career. Unlike many of his scientific contemporaries, d'Herelle never pursued formal higher education. Instead, he voraciously read scientific literature and sought hands-on experience, leading to a unique blend of enthusiasm and prowess in scientific inquiry.
In 1899, d'Herelle's journey took him to Guatemala, where he began to experiment in earnest. There, he brewed beer and studied fermentation, igniting his interest in the microbial world. These formative years were characterized by a relentless pursuit of knowledge outside conventional academic channels, an approach that would shape d'Herelle's scientific endeavors and open-minded approach to research.
The Discovery of Bacteriophages
D'Herelle's most significant breakthrough came after he joined the Pasteur Institute in Paris in 1911. There, he focused on understanding dysentery and cholera, which were rampant in France at the time. His investigations into these bacterial infections led to one of the most significant discoveries in microbiology—the existence of bacteriophages.
In 1917, while conducting research on soldiers suffering from dysentery, d'Herelle observed that certain microscopic entities could lyse or destroy bacterial cultures. He documented these observations with meticulous detail, proposing the existence of "invisible antagonists" of bacteria, which he later named bacteriophages. These viruses were found to be specific to certain bacteria, raising the possibility of using them as therapeutic agents.
Although the discovery was met with skepticism, d'Herelle's work steadily gained traction. His meticulous documentation and persistent advocacy for bacteriophage therapy paved the way for its adoption in treating bacterial infections, offering a novel approach that was especially crucial before the advent of antibiotics.
Bacteriophage Therapy: Hope before Antibiotics
The discovery of bacteriophages provided an alternative to treating bacterial infections, long before the discovery of penicillin in 1928 by Alexander Fleming. D'Herelle was a fervent proponent of using bacteriophages in therapeutic settings to combat infectious diseases. His conviction in their effectiveness led to clinical trials and widespread use in treating ailments such as dysentery, cholera, and even typhoid fever in the early 20th century.
However, the path to acceptance was not without its challenges. The medical community was polarized, divided between skepticism and curiosity over d'Herelle’s claims. Despite this, d'Herelle's research laid the groundwork for future therapeutic use, influencing studies on bacteriophage properties, specificity, and effectiveness in clinical settings.
His work gained particular prominence in regions such as Eastern Europe and the former Soviet Union, where bacteriophage therapy continues to be utilized today. D'Herelle's advocacy and scientific contributions helped establish a legacy that remains relevant in modern microbiology, especially in the context of rising antibiotic resistance.
The Legacy of Innovation and Dedication
Félix d'Herelle's contributions extend beyond the discovery of bacteriophages. His enduring impact is rooted in his innovative spirit and unwavering dedication to scientific inquiry. He was a pioneer who bridged the gap between traditional academic environments and practical, problem-solving scientific approaches. With a career that defied conventional academic paths, d'Herelle embodied the essence of a self-taught scientist confronting the challenges of his time with diligence and ingenuity.
As the world continues to grapple with antibiotic resistance, d'Herelle's work is undergoing a renaissance, with bacteriophage therapy emerging as a promising alternative or complement to antibiotics. His legacy is a testament to the transformative power of scientific curiosity and perseverance, influencing modern research, medical treatments, and the broader field of microbiology.
In our next installment, we delve deeper into d'Herelle's later life, exploring his global influence, the broader impact of his discoveries in the scientific community, and the enduring relevance of bacteriophage therapy in contemporary medicine. Stay tuned as we continue to uncover the fascinating journey of Félix d'Herelle, a visionary who dared to look beyond the visible world and changed the course of medical science.
Global Impact and Collaborations
After his monumental discovery of bacteriophages, Félix d'Herelle began to garner attention from various corners of the globe. His work attracted the interest of scientists and medical professionals eager to explore this novel concept of viral therapy against bacterial infections. D'Herelle's career soon took on an international dimension, marked by travels and collaborations that would extend the reach of his innovative ideas and solidify his reputation as a pioneer in microbiology.
In the 1920s, d'Herelle's research took him to multiple continents. He worked extensively in countries such as India and Egypt, where bacterial infections like cholera were prevalent. His interventions demonstrated the potential of bacteriophage therapy to alleviate public health crises, as he successfully applied his methods to real-world applications. These international ventures not only spread the knowledge of bacteriophages but also highlighted the importance of cross-cultural scientific exchanges in the fight against infectious diseases.
During this period, d'Herelle also collaborated with Georgian bacteriologist George Eliava. This partnership, which began at the Pasteur Institute, led to the establishment of the Eliava Institute in Tbilisi, Georgia—a major center for bacteriophage research to this day. The collaboration between d'Herelle and Eliava was more than a professional alliance; it was a fusion of ideas and aspirations toward advancing the therapeutic potential of bacteriophages, paving the way for ongoing research in the field.
Challenges and Controversies
Despite the promising applications of bacteriophages, Félix d'Herelle’s journey was not devoid of challenges. The scientific community met his ideas with a mix of intrigue and skepticism. In the early 20th century, virology was still in its nascent stages, and the mechanisms behind bacteriophages were not fully understood. This lack of comprehension led to controversies about their efficacy and safety, hindering widespread acceptance.
Moreover, the emergence of antibiotics in the late 1930s and 1940s overshadowed bacteriophage therapy. When penicillin and other antibiotics proved remarkably effective against a broad spectrum of bacteria, interest and investment in bacteriophage research waned. The focus shifted towards antibiotic solutions, with bacteriophage therapy being largely sidelined in Western medicine.
Nevertheless, d'Herelle remained steadfast in his belief in the potential of bacteriophages. He continued to advocate for their use, particularly in regions where antibiotics were scarce or ineffective due to resistance. His unwavering commitment to his research in the face of adversity underscored his resolute character and dedication to advancing medical science.
Enduring Influence and Modern Resurgence
In an ironic twist of fate, the scientific community’s initial skepticism of Félix d'Herelle’s discoveries is being re-evaluated in the context of the modern-day challenge of antibiotic resistance. As bacteria evolve and become resistant to existing antibiotics, the global health community is revisiting the potential of bacteriophage therapy as a viable alternative or complementary treatment.
Countries such as Poland and Russia, where research into bacteriophages has continued uninterrupted, are at the forefront of this resurgence. These nations have amassed decades of clinical experience utilizing phage therapy, data that is now invaluable as the world seeks solutions to combat resistant bacterial strains.
Modern advancements in molecular biology and genetic engineering further enhance the potential of bacteriophage therapy. Current research efforts are focused on engineering phages to improve their therapeutic efficacy, targeting specificity, and overcoming hurdles such as bacterial resistance. This new era of phage research is breathing life into d'Herelle’s early 20th-century visions, blending classical microbiology with cutting-edge biotechnology.
The Timeless Vision of Félix d'Herelle
As the renaissance of bacteriophage therapy unfolds, Félix d'Herelle’s influence resonates more profoundly than ever. He was a trailblazer who, through perseverance and ingenuity, advocated for a path less taken in the realm of medical science. His ability to envisage solutions beyond the scope of current knowledge remains a hallmark of innovative thinking in scientific endeavors.
D'Herelle’s legacy exemplifies the power of pursuing scientific understanding with tenacity and open-mindedness. His contributions continue to inspire new generations of researchers committed to combating the persistent and ever-evolving challenges posed by infectious diseases.
In the final segment of this series, we will delve into the personal aspects of d'Herelle's life, exploring his character, motivations, and the lasting impact of his work on contemporary scientific research and healthcare. Join us as we conclude our exploration of Félix d'Herelle, an awe-inspiring leader whose visionary insights continue to shape the future of microbiology and therapeutic innovation.
The Personal Side of a Scientific Trailblazer
Beyond his groundbreaking scientific contributions, Félix d'Herelle was a man of remarkable character and intriguing personal dimensions. A self-taught polymath with an unconventional career, d'Herelle was driven by an unyielding curiosity and a deep-seated passion for advancing medical science. His journey was marked by both triumphs and tribulations, underscoring a profound dedication to the art of discovery.
D'Herelle was known for his relentless pursuit of understanding. His work was characterized by an unwavering intensity and a hands-on approach to experimentation. Despite lacking formal academic qualifications, he harbored an innate scientific intuition that allowed him to conceptualize and execute complex research endeavors. This commitment to self-directed learning and exploration was emblematic of d'Herelle’s innovative spirit.
His collaborations with scientists like George Eliava also reflect his openness and willingness to share ideas. By forging international connections, d'Herelle transcended the geographic and cultural barriers of his time, building a network of like-minded researchers who supported and expanded upon his work. These collaborations not only enriched his own research but also fostered a collaborative ethos within the scientific community.
Legacy and the Human Element
Félix d'Herelle's legacy is not merely confined to his scientific achievements. His life and work embody the essential qualities of perseverance, intellectual curiosity, and a profound belief in the potential of scientific inquiry to resolve pressing health challenges. D'Herelle's legacy is an inspiring testament to the power of human dedication when guided by a compelling vision.
He was a visionary who dared to challenge the status quo and explore uncharted territories in microbiology. In doing so, d'Herelle helped usher in a new era of understanding and therapeutic possibilities. His pioneering spirit continues to inspire modern researchers who face the daunting task of overcoming contemporary challenges such as antibiotic resistance and emerging infectious diseases.
In recent years, the relevance of d'Herelle's work has been further accentuated by its adaptation to modern contexts. The exploration of bacteriophage therapy as a countermeasure to antibiotic resistance has reignited interest in d'Herelle’s earlier insights, illustrating the enduring nature of his contributions. As a symbol of the continuous journey of scientific progress, his legacy persists in influencing research, shaping medical practices, and inspiring future scientific endeavors.
The Continuing Impact of a Visionary
Today, research institutions across the globe are revisiting bacteriophage therapy and investing in its potential development. The renewed interest highlights the timeless insight Félix d'Herelle possessed, recognizing bacteriophages as significant players in the battle against bacterial infections. His early 20th-century work is integral to the resurgence of phage therapy as a promising biological tool in modern medicine.
Modern bacteriophage research extends to various fields, including agriculture, environmental science, and biotechnology, where phages are explored for their ability to target and neutralize specific bacteria. This multidisciplinary application underscores the versatility and potential of d'Herelle’s discovery, demonstrating its broad relevance beyond traditional medical paradigms.
Furthermore, the personal attributes of innovation and resilience that characterized d'Herelle’s life serve as a beacon for aspiring scientists. His ability to transform challenges into opportunities and maintain a steadfast focus on his research goals, despite skepticism and setbacks, offers a timeless lesson on the importance of perseverance and adaptability in scientific pursuits.
Conclusion: Celebrating a Life of Discovery
Félix d'Herelle’s life journey, punctuated by scientific breakthroughs and unwavering dedication, is a powerful narrative of discovery and vision. His pioneering work in bacteriophage research and therapy laid a foundational stone for modern microbiology, contributing a transformative approach to combating bacterial infections. As the world continuously battles the complexities of emerging health threats, his work remains a critical reference point.
Celebrating Félix d'Herelle is to celebrate the spirit of innovation and the relentless pursuit of knowledge that drives scientific progress forward. As we stand on the shoulders of such trailblazers, it is their legacy that encourages new generations to pursue the unknown, challenge established norms, and strive for advancements that ultimately improve human lives.
The story of Félix d'Herelle is as much about the science he championed as it is about the indomitable human spirit. His legacy endures as a symbol of what can be achieved when curiosity, determination, and a vision for the future intersect to illuminate paths previously unexplored. It is this legacy that continues to inspire and will remain vital as science reaches for new frontiers in the years to come.

Ronald Ross: Pioneering the Path to Understanding Malaria
Introduction
In the annals of medical history, few individuals have made contributions as significant and transformative as Ronald Ross. His groundbreaking work in understanding malaria not only altered the course of epidemiology but also laid the foundation for combating one of humanity's most persistent diseases. Born in the late 19th century, Ross's story is one of relentless curiosity, scientific foresight, and a profound commitment to improving public health. This article delves into the life of Ronald Ross, exploring his seminal discoveries and their lasting impact on medical science.
Early Life and Education
Ronald Ross was born on May 13, 1857, in Almora, a town nestled in the foothills of the Indian Himalayas. His father served as a general in the British Army, instilling in young Ross a sense of duty and discipline. At the age of eight, Ross was sent to England for his education, first at the prestigious Ryde School, then at Rossall School in Lancashire, and finally at St. Bartholomew's Hospital Medical College in London.
While his initial passion leaned more towards the arts, Ross eventually chose medicine, a decision influenced by his father’s insistence that he pursue a practical profession. During his years at medical school, Ross demonstrated a remarkable aptitude for scientific research, laying the groundwork for his future endeavors in medical science.
Career Beginnings and Early Challenges
After completing his medical studies, Ross joined the Indian Medical Service (IMS) in 1881, drawn by the allure of practicing medicine in a tropical yet challenging environment. His early years in India, however, were not marked by immediate success. Ross faced numerous professional and personal challenges, including bouts of illness and a struggle to balance his creative writing aspirations with his medical duties.
Despite these challenges, Ross remained committed to his role and gradually developed a keen interest in researching tropical diseases, particularly malaria. At the time, malaria was rampant in India, causing widespread illness and death. The disease’s etiology, however, remained shrouded in mystery, with prevailing theories attributing it to miasmas or various noxious environmental factors.
The Quest to Unravel the Mystery of Malaria
Ross's interest in malaria research was piqued in 1894 during a chance meeting with Dr. Patrick Manson, a leading authority on tropical medicine. Manson postulated a groundbreaking hypothesis: malaria was transmitted not via the air, but by the Anopheles mosquito. Armed with this new perspective, Ross was inspired to investigate this theory further, embarking on a scientific quest that would consume the next several years of his life.
Upon his return to India, Ross diligently conducted experiments, focusing on mosquitoes' role in the transmission of malaria. His environment was both a laboratory and a natural habitat full of potential scientific revelations. His extensive documentation of mosquito behavior, biology, and their potential link to human diseases was meticulous and groundbreaking.
Breakthrough Discovery
In 1897, Ross achieved a monumental breakthrough in the study of malaria. Through a series of experiments and observations, he conclusively demonstrated that Anopheles mosquitoes were indeed the vector responsible for transmitting the malaria parasite. He discovered the parasite in the gastrointestinal tract of the mosquito, establishing a concrete link between the insect and the transmission of malaria to humans.
This discovery was not merely a scientific triumph; it was a watershed moment in public health. By unravelling the transmission mechanism, Ross opened the door to developing effective preventive measures against malaria, significantly reducing its prevalence and mortality rate. His findings also validated Manson’s hypothesis, fundamentally changing the understanding of vector-borne diseases.
Recognition and Legacy
For his groundbreaking work, Ronald Ross was awarded the prestigious Nobel Prize in Physiology or Medicine in 1902. This accolade not only honored his scientific achievements but also underscored the global impact of his research on malaria. Ross's work paved the way for a better understanding of how infectious diseases spread and laid the groundwork for future research in tropical medicine.
Beyond malaria, Ross’s contributions to medical science and public health were vast. He was instrumental in founding the Liverpool School of Tropical Medicine, where he continued to champion research into infectious diseases. Ross also advocated for public health policies aimed at controlling mosquitoes through environmental management and education.
Conclusion
Ronald Ross's life and work stand as a testament to the profound impact of scientific inquiry driven by curiosity and a desire to improve human health. His contributions have saved countless lives and continue to inform modern approaches to combating infectious diseases. As we reflect on his legacy, Ross's story reminds us of the enduring power of discovery to change the world for the better.
A Pivotal Shift in Medical Research
The implications of Ronald Ross’s discovery extended far beyond the immediate understanding of malaria transmission. His work represented a paradigm shift in medical research and public health, emphasizing the importance of understanding disease vectors. By demonstrating how mosquitoes transmitted malaria, Ross laid the foundation for vector control—a critical component in the strategy to manage and eradicate vector-borne diseases.
Ross’s approach to unraveling the malaria transmission cycle was methodical and innovative. He meticulously studied the life cycle of the malaria parasite within the mosquito host. His landmark discovery was not just in identifying the mosquito as the vector, but in detailing the complex life cycle of the malaria parasite—Plasmodium—in both the mosquito and human hosts. This comprehensive understanding allowed for the development of targeted interventions designed to interrupt the transmission of malaria at its source.
Impact on Public Health Strategies
Ross’s findings had a direct and profound impact on public health strategies worldwide. Understanding that malaria transmission involved mosquitoes allowed public health officials to design interventions that targeted the vector itself. Vector control measures such as the use of insecticides, bed nets, and environmental management became central strategies in the fight against malaria.
Ross actively advocated for these strategies and was a vocal proponent of sanitation and preventative measures. He believed that controlling the mosquito population was paramount, often stressing the importance of eliminating stagnant water sources where mosquitoes bred. This emphasis on practical public health measures helped shape the field of epidemiology, influencing future generations of scientists and health policy-makers.
His work also contributed to the development of programs aimed at educating communities about the role of mosquitoes in malaria transmission. By fostering awareness, Ross helped enable communities to take preventive actions that reduced their risk of contracting the disease. These educational efforts became integral to public health campaigns, reinforcing the idea that prevention through awareness and environmental control was as crucial as medical treatment.
The Liverpool School of Tropical Medicine
With his career trajectory solidly aimed at addressing tropical diseases, Ronald Ross became instrumental in the establishment of the Liverpool School of Tropical Medicine (LSTM) in 1898. This was the first institution of its kind dedicated to the study of tropical diseases. Ross's involvement was vital, not only because of his expertise but also due to his commitment to establishing a center of excellence in tropical medicine.
At LSTM, Ross continued to extend his research into malaria and other tropical diseases, closely collaborating with prominent scientists and researchers. His work at the institution helped foster a multidisciplinary approach to disease research, incorporating parasitology, entomology, and public health.
Under Ross’s influence, LSTM became a hub for training medical professionals specialized in handling the complex challenges associated with tropical diseases. His emphasis on cross-disciplinary collaboration helped advance research in the field significantly. This legacy persists today, as LSTM continues to lead innovative research and training on tropical diseases globally.
Challenges and Controversies
While Ross's scientific achievements were substantial and globally recognized, his career was not without challenges and controversies. The scientific community of the time was competitive, and collaborations often involved intellectual conflicts. Ross had a strained relationship with Italy’s Giovanni Battista Grassi, a bacteriologist who also contributed to understanding malaria transmission. The scientific debate over who discovered the complete lifecycle of the malaria parasite highlighted how competitive and fraught with challenges the scientific environment could be.
Ross also faced criticism for his assertive personality and his often contentious interactions with peers. While these qualities could sometimes alienate colleagues, they also reflected his deep dedication to his work and an unwavering belief in the potential of science to solve humanity's most pressing problems. Despite these challenges, his scientific rigor remained uncompromised, and his contributions to the field have withstood the test of time.
Legacy of Innovation and Determination
Ronald Ross’s legacy extends beyond his scientific and medical contributions. His life’s work set a precedent for how scientific research could directly translate into public health advancements that alter the course of prevalent diseases. By combining scientific curiosity with practical applications, Ross epitomized the role of a scientist committed to the betterment of human health.
Ross's story underscores the importance of perseverance, collaboration, and a willingness to challenge prevailing scientific assumptions. His determination to understand malaria led to breakthroughs that have saved millions of lives and continue to influence modern strategies in the fight against infectious diseases.
His impact is evident today as researchers, public health officials, and policy-makers continue to draw from his pioneering insights to confront existing and emerging health challenges. As we continue to build on Ross’s groundbreaking work, his story remains an enduring source of inspiration, reminding us of the transformative power that research and dedication hold in our ongoing battle against disease.
Further Contributions and Innovations
In addition to his monumental work on malaria, Ronald Ross made several other significant contributions to the field of epidemiology and medicine. His interests spanned various tropical diseases, reflecting his commitment to understanding and mitigating the impact of these afflictions on human populations. Among his many pursuits, Ross engaged in research on kala-azar, a tropical disease caused by the Leishmania parasite, and filariasis, caused by thread-like nematodes. His work in these areas further exemplified his passion for combating the diseases prevalent in regions with little access to advanced healthcare and resources.
Ross was a strong advocate for interdisciplinary approaches in science, encouraging collaboration between fields such as entomology, parasitology, and public health. He recognized that solving complex health challenges required input from multiple scientific domains, a viewpoint that continues to resonate in contemporary research. His writings and lectures often reflected his belief in the unification of scientific efforts to achieve substantial advancements in understanding and controlling diseases.
Influence on Future Research and Policy
Ronald Ross's legacy is evident not only in his direct scientific contributions but also in the influence he had on policy and the direction of future research endeavors. His advocacy for vector control and public health measures laid the groundwork for national and international strategies to manage malaria and other vector-borne diseases. His emphasis on environmental management as a method of disease control has been foundational to modern-day initiatives that aim to promote sustainable practices while reducing disease transmission.
The strategic frameworks developed from Ross's research were precursors to many of the global health campaigns that followed. Organizations such as the World Health Organization and various international malaria control programs have built upon his principles of education, prevention, and intervention. These initiatives have driven extensive progress in reducing the impact of malaria worldwide, showcasing the enduring relevance of Ross’s work.
Moreover, Ross's commitment to research and innovation inspired many future scientists and researchers, fostering a culture of scientific inquiry that encouraged others to pursue health-related research with social and ecological consciousness. The ethos he championed continues to influence public health policy making, emphasizing the need for robust scientific evidence in crafting effective global health strategies.
The Literary Contribution
Beyond his scientific endeavors, Ronald Ross was also a prolific writer, contributing to literature with poems, essays, and reflective pieces, often drawing from his rich experiences in medicine and travel. His literary works, though lesser-known than his scientific publications, provided personal insights into his thoughts and the emotional journey accompanying his scientific exploration.
Ross's poetry and writings revealed a scientist who viewed his work not just as a profession but as a profound calling. His ability to merge his love for science and literature enriched his contributions to both fields and offered a unique perspective on the interconnectedness of these disciplines. Through his writings, Ross communicated complex scientific ideas in an accessible manner, extending his influence beyond the scientific community to reach a broader audience.
Enduring Impact and Commemoration
Ronald Ross passed away on September 16, 1932, but the impact of his work continues to resonate across the globe. His life’s work is commemorated in numerous ways, from the Ross Institute of Tropical Hygiene in England, established to continue investigations into tropical and communicable diseases, to awards named in his honor that recognize exceptional contributions to parasitology and tropical medicine. These commemorations serve as a testament to Ross’s enduring influence on the medical sciences and public health arenas.
His discoveries remain a cornerstone in the understanding and management of malaria, influencing countless research studies and policy formulations to this day. As global challenges related to infectious diseases grow more complex, Ross's legacy provides a reminder of the achievements possible through dedication, curiosity, and a relentless pursuit of knowledge.
Conclusion
Ronald Ross was more than a scientist; he was a pioneer whose work transcended the boundaries of his time. His unwavering commitment to unraveling the mysteries of malaria transformed public health strategies and saved innumerable lives, an influence that persists in today’s public health landscape. Ross's multidisciplinary approach to problem-solving, combined with his passion for education and communication, set a precedent that continues to drive innovation in medical science.
As we confront new public health challenges in the 21st century, Ross's legacy remains a guiding light, emphasizing the critical role of thorough scientific research, collaboration, and education in overcoming adversity. His life and work remind us of the potential within dedicated scientific inquiry to significantly enhance global health outcomes, continually inspiring future generations of scientists and researchers.