AI vs. Superbugs: Fighting Antibiotic Resistance
The escalating crisis of antibiotic resistance, driven by so-called superbugs, threatens to undo a century of medical progress. This global health emergency is now meeting a formidable, new-age challenger: artificial intelligence. By accelerating drug discovery, predicting outbreaks, and personalizing treatments, AI is revolutionizing the fight against antimicrobial resistance (AMR).
Traditional methods are buckling under the weight of this crisis. The discovery of new antibiotics has slowed to a trickle, while diagnostic processes remain slow. Artificial intelligence offers a paradigm shift, using machine learning and generative models to analyze vast datasets and identify solutions at unprecedented speed.
Projections indicate antimicrobial resistance (AMR) could cause 10 million deaths annually by 2050, a staggering increase from current figures.
The Scale of the Superbug Crisis
Antibiotic resistance is not a future threat; it is a present danger. Superbugs like MRSA and drug-resistant strains of E. coli and Klebsiella pneumoniae are rendering our most powerful medicines ineffective. The human and economic costs are already severe and growing rapidly.
Alarming Mortality and Infection Rates
The statistics paint a dire picture. A 2021 baseline of 4.71 million AMR-associated deaths is projected to soar to 8.22 million by 2050—a rise of 74.5%. This trajectory points directly toward the feared milestone of 10 million annual deaths globally. In clinical settings today, approximately one in every six lab-confirmed bacterial infections shows signs of resistance.
- Projected 2050 Deaths: 10 million per year.
- AMR-Associated Death Increase (2021-2050): From 4.71M to 8.22M (+74.5%).
- Current Resistant Infections: 1 in 6 lab-confirmed cases.
The Innovation Gap in Antibiotics
The rise of superbugs coincides with a dramatic decline in new antibiotic development. The pharmaceutical pipeline has dried up due to scientific challenges and limited commercial incentives. For decades, medicine has relied on modifications of existing drug classes, but bacteria evolve quickly to overcome them. This innovation gap has created an urgent need for novel therapeutic approaches and faster, more precise diagnostics.
How AI is Revolutionizing the Battle Plan
Artificial intelligence is stepping into this breach with a multi-pronged strategy. Its core strength lies in pattern recognition and data mining at a scale impossible for humans. AI systems can process genomic sequences, clinical records, and chemical databases to find answers hidden in plain sight.
Supercharging Diagnostics and Prediction
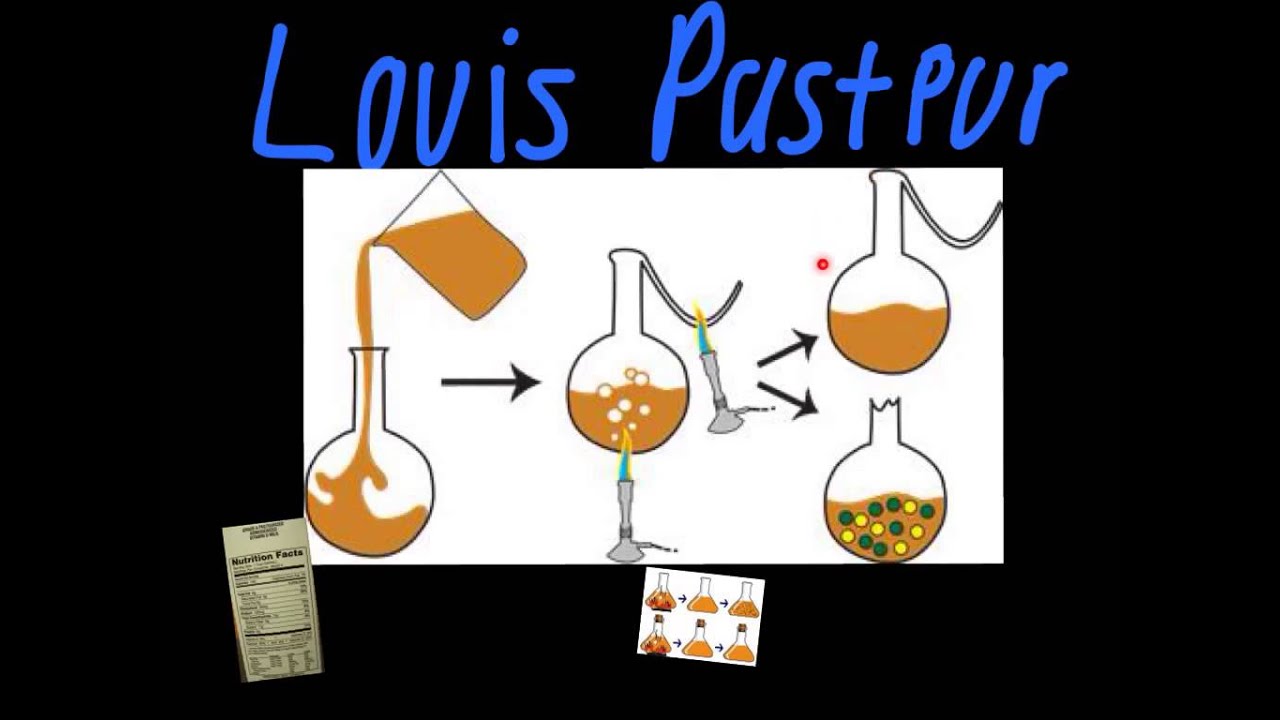
Timely identification of a pathogen and its resistance profile is critical for effective treatment. Traditional culture-based methods can take days. AI-powered diagnostics are slashing that time to hours.
Researchers are training sophisticated AI models on massive datasets, such as over 300,000 bacterial samples analyzed by MALDI-TOF mass spectrometry and genomic sequencing. These models can accurately predict resistance in dangerous pathogens like Staphylococcus aureus and Klebsiella pneumoniae almost instantly. This speed enables clinicians to prescribe the right antibiotic from the start, improving outcomes and curbing misuse.
Optimizing Treatment and Stewardship
Beyond diagnosis, AI supports better antibiotic use through clinical decision support systems. By analyzing local resistance patterns and individual patient data, these tools can recommend the most effective drug and dosage. Studies suggest such AI systems can reduce prescription mismatches by up to 50%. This enhances antimicrobial stewardship, a key pillar in slowing the development of resistance.
The Generative AI Breakthrough in Drug Discovery
The most revolutionary application of AI may be in creating entirely new weapons for the arsenal. Generative AI models are moving beyond simply screening existing compound libraries to designing new-to-nature molecules from scratch.
From Halicin to Millions of Designs
The potential of AI in this field was first spectacularly demonstrated with the discovery of halicin, a powerful broad-spectrum antibiotic identified by an MIT model in 2020. This was followed by abaucin, an AI-discovered compound highly specific to Acinetobacter baumannii. These successes proved that machine learning could find needles in the haystack of chemical possibilities.
The field has since exploded. In a landmark 2025 study, MIT researchers used a generative AI platform called ChemPox to design a staggering over 36 million novel antibiotic compounds in silico. From this vast virtual library, they identified several structurally unique candidates effective against drug-resistant Neisseria gonorrhoeae (gonorrhea) and MRSA.
"Generative AI allows us to explore regions of chemical space that are simply inaccessible through conventional methods or existing compound libraries," noted a lead researcher on the project.
Novel Mechanisms to Outsmart Resistance
Critically, these AI-designed antibiotics often work through novel mechanisms. For example, some of the newly discovered compounds disrupt bacterial cell membranes in ways that existing drugs do not. This makes it much harder for superbugs to develop immediate resistance, as they have not encountered this mode of attack before. This approach compresses the traditional preclinical discovery timeline from years down to mere hours or days.
Tackling the Gram-Negative Threat
A particularly urgent focus is on Gram-negative bacteria, such as E. coli and K. pneumoniae. Their double-layer cell envelope and efficient efflux pumps make them exceptionally difficult to target. Major initiatives are now leveraging AI to crack this problem.
In 2025, GSK and the Fleming Initiative launched six Grand Challenges, backed by £45 million in funding. This collaboration uses AI and supercomputing to model the complex biology of Gram-negative pathogens. The goal is to design molecules that can penetrate their defenses and disable key survival mechanisms, creating a new generation of effective treatments.



















Comments