Uterine Peristalsis: Mechanisms, Hormonal Control, and Clinical Implications
Introduction to Uterine Peristalsis
Uterine peristalsis refers to the wave-like contractions of the subendometrial myometrium, the inner muscular layer of the uterus. These contractions play a crucial role in reproductive health, particularly during the follicular phase of the menstrual cycle. Controlled primarily by estradiol and influenced by oxytocin, peristalsis facilitates sperm transport and may aid in embryo implantation.
Research, including a foundational 1998 study cited 161 times, highlights the importance of these contractions in fertility and assisted reproductive technologies (ART). Understanding the mechanisms behind uterine peristalsis can improve clinical outcomes in treatments like in vitro fertilization (IVF).
Hormonal Regulation of Uterine Peristalsis
Role of Estradiol in Peristaltic Activity
The dominant follicle releases estradiol, which drives the frequency of uterine contractions. During the follicular phase, estradiol levels rise, peaking just before ovulation. This hormonal surge enhances peristaltic waves, ensuring optimal conditions for gamete transport.
Studies show that exogenous estradiol, such as estradiol valerate, mimics natural peristaltic patterns. However, high doses do not significantly increase contraction frequency due to system refractoriness.
Influence of Oxytocin on Uterine Contractions
Oxytocin acts locally within the endometrial-subendometrial unit, enhancing the effects of estradiol. Unlike systemic oxytocin, which has limited impact, autocrine/paracrine oxytocin plays a key role in modulating peristalsis.
Clinical trials with intravenous oxytocin in the late follicular phase showed minimal additional effects, suggesting that oxytocin's role is supportive rather than primary.
Pharmacological Insights and Clinical Observations
Impact of Clomiphene Citrate on Peristalsis
Clomiphene citrate, a common fertility drug, slightly suppresses peristaltic frequency despite elevating estradiol levels. This paradoxical effect underscores the complexity of hormonal interactions in uterine contractions.
Research indicates that while clomiphene increases estradiol, it does not proportionally enhance peristalsis, likely due to receptor downregulation or other compensatory mechanisms.
Effects of Exogenous Hormones on Uterine Contractions
Administration of human menopausal gonadotropin (hMG) or estradiol valerate closely replicates natural peristaltic patterns. These findings are critical for fertility treatments, where timing and hormonal balance are essential.
Key observations include:
- Natural cycles show a baseline increase in peristalsis, peaking preovulatorily.
- Estradiol valerate/hMG interventions match natural contraction frequencies.
- High estradiol doses do not exceed normal peristaltic peaks, indicating refractoriness.
Physiological Role of Uterine Peristalsis
Directed Peristaltic Waves vs. Luteal-Phase Dysperistalsis
During the follicular phase, peristaltic waves are directed, facilitating rapid transport of sperm and embryos toward the fundus. In contrast, the luteal phase exhibits dysperistalsis—retrograde contractions that may contribute to conditions like endometriosis.
This distinction is vital for diagnosing and treating reproductive disorders, as abnormal peristalsis can impair fertility.
Study Design and Key Findings
Researchers used vaginal sonography to track peristalsis across different phases of the menstrual cycle. The study confirmed that estradiol is the primary driver of contractions, with oxytocin playing a secondary, synergistic role.
Key findings include:
"Peristaltic contractions in the subendometrial myometrium are critical for reproductive success, with estradiol and oxytocin working in tandem to optimize uterine function."
Clinical Relevance and Therapeutic Implications
Applications in Fertility Treatments
Understanding uterine peristalsis is crucial for IVF protocols. Timing embryo transfer with peak peristaltic activity can improve implantation rates. Clinicians must consider hormonal balance to avoid refractoriness in superovulation treatments.
For example:
- IVF timing: Aligning embryo transfer with natural peristaltic peaks enhances success.
- Avoiding high estradiol doses: Prevents system refractoriness and suboptimal contractions.
Research Gaps and Future Directions
While the 1998 study remains foundational, gaps exist in understanding long-term impacts and molecular pathways. Modern imaging techniques and AI-driven analysis could provide real-time insights into peristaltic activity.
Future research should explore:
- Oxytocin receptor dynamics in the endometrial-subendometrial unit.
- Non-invasive monitoring techniques for clinical applications.
- Long-term effects of hormonal interventions on uterine function.
Conclusion of Part 1
This section has introduced the mechanisms, hormonal regulation, and clinical implications of uterine peristalsis. In Part 2, we will delve deeper into diagnostic techniques, therapeutic strategies, and emerging research trends.
Diagnostic Techniques for Assessing Uterine Peristalsis
Vaginal Sonography: The Gold Standard
Vaginal sonography remains the most reliable method for visualizing uterine peristalsis. This non-invasive technique allows clinicians to observe subendometrial contractions in real-time, providing critical insights into reproductive health.
Key advantages of vaginal sonography include:
- High-resolution imaging of the endometrial-subendometrial unit.
- Real-time monitoring of peristaltic waves during different menstrual phases.
- Minimal discomfort for patients, making it ideal for repeated assessments.
Emerging Technologies in Peristalsis Monitoring
Advancements in medical imaging and artificial intelligence (AI) are revolutionizing the study of uterine peristalsis. 3D ultrasound and MRI offer deeper insights into contraction patterns, while AI algorithms can analyze large datasets to predict optimal fertility windows.
Potential future developments include:
- Automated peristalsis tracking via machine learning.
- Portable ultrasound devices for at-home monitoring.
- Integrated hormone-peristalsis mapping for personalized fertility plans.
Therapeutic Strategies for Optimizing Uterine Peristalsis
Hormonal Interventions in Fertility Treatments
Hormonal therapies play a pivotal role in regulating uterine peristalsis, particularly in assisted reproductive technologies (ART). Clinicians often use estradiol supplements to mimic natural cycles, while oxytocin modulators may enhance contraction efficiency.
Common hormonal interventions include:
- Estradiol valerate to simulate follicular phase conditions.
- Human menopausal gonadotropin (hMG) for controlled ovarian stimulation.
- Clomiphene citrate (with caution due to its suppressive effects on peristalsis).
Timing Embryo Transfer with Peristaltic Peaks
In IVF procedures, synchronizing embryo transfer with peak peristaltic activity can significantly improve implantation rates. Studies suggest that transfers performed during the late follicular phase—when contractions are most robust—yield better outcomes.
Key considerations for timing include:
- Monitoring estradiol levels to predict peristaltic peaks.
- Avoiding luteal phase dysperistalsis, which may hinder embryo movement.
- Personalizing protocols based on individual peristaltic patterns.
Uterine Peristalsis and Reproductive Disorders
Link Between Dysperistalsis and Endometriosis
Endometriosis is closely associated with luteal-phase dysperistalsis, where retrograde contractions may contribute to the displacement of endometrial tissue. Research indicates that women with endometriosis exhibit abnormal peristaltic patterns, which could serve as a diagnostic marker.
Clinical observations include:
- Increased retrograde contractions during the luteal phase.
- Reduced directed peristalsis in the follicular phase.
- Correlation with pelvic pain and infertility.
Impact on Unexplained Infertility
In cases of unexplained infertility, abnormal uterine peristalsis may be a contributing factor. Women with suboptimal contraction patterns often struggle with sperm transport and embryo implantation, even when other fertility parameters appear normal.
Potential solutions include:
- Peristalsis-enhancing therapies (e.g., low-dose oxytocin).
- Targeted hormonal adjustments to restore natural contraction rhythms.
- Advanced imaging to identify subtle peristaltic dysfunctions.
Research Gaps and Future Directions
Molecular Pathways and Oxytocin Receptor Dynamics
While the 1998 study established the role of estradiol and oxytocin, molecular mechanisms remain poorly understood. Future research should explore:
- Oxytocin receptor expression in the endometrial-subendometrial unit.
- Signal transduction pathways governing peristaltic contractions.
- Genetic factors influencing individual peristaltic patterns.
Long-Term Effects of Hormonal Interventions
Most studies focus on short-term peristaltic responses to hormonal treatments. However, long-term effects—such as receptor downregulation or uterine fatigue—require further investigation. Clinicians must balance immediate fertility goals with potential long-term risks.
Key questions include:
- Does prolonged estradiol exposure alter peristaltic efficiency?
- Can repeated oxytocin use lead to desensitization?
- Are there cumulative effects of fertility drugs on uterine function?
Conclusion of Part 2
This section has explored diagnostic techniques, therapeutic strategies, and the link between uterine peristalsis and reproductive disorders. In Part 3, we will conclude with a summary of key takeaways, practical recommendations, and the future of peristalsis research.
Key Takeaways and Practical Recommendations
Summarizing the Role of Uterine Peristalsis in Fertility
Uterine peristalsis is a critical yet often overlooked factor in reproductive health. Driven by estradiol and modulated by oxytocin, these contractions facilitate sperm transport and embryo implantation. Understanding their mechanisms can significantly improve fertility treatments and diagnostic approaches.
Key insights include:
- Estradiol dominance in the follicular phase enhances peristaltic frequency.
- Oxytocin’s local action supports but does not override estradiol’s effects.
- Dysperistalsis in the luteal phase may contribute to conditions like endometriosis.
Clinical Recommendations for Fertility Specialists
For clinicians, optimizing uterine peristalsis involves a combination of hormonal balance, timing strategies, and advanced monitoring. Practical steps include:
- Monitoring estradiol levels to predict peak peristaltic activity.
- Avoiding excessive clomiphene citrate, which may suppress contractions.
- Using vaginal sonography to assess peristaltic patterns before IVF.
- Personalizing embryo transfer timing based on individual peristaltic rhythms.
Future Research and Technological Advancements
Potential Breakthroughs in Peristalsis Research
While the 1998 study remains foundational, modern research must address unanswered questions. Future directions include:
- Molecular studies on oxytocin receptor dynamics.
- AI-driven peristalsis tracking for real-time fertility predictions.
- Long-term effects of hormonal interventions on uterine function.
Emerging technologies like 3D ultrasound and machine learning could revolutionize how we diagnose and treat peristaltic dysfunctions.
The Role of AI and Machine Learning
Artificial intelligence is poised to transform fertility research by analyzing vast datasets to identify patterns in uterine contractions. Potential applications include:
- Automated peristalsis analysis from ultrasound scans.
- Predictive modeling for optimal embryo transfer timing.
- Personalized treatment plans based on individual peristaltic profiles.
"The integration of AI into reproductive medicine could unlock new possibilities for diagnosing and treating infertility linked to uterine peristalsis."
Addressing Common Misconceptions
Myth: Higher Estradiol Levels Always Improve Fertility
A common misconception is that maximizing estradiol will always enhance fertility. However, research shows that excessive estradiol can lead to system refractoriness, where the uterus no longer responds optimally to hormonal signals.
Key clarifications:
- Optimal estradiol levels vary by individual.
- High doses may not improve peristalsis beyond natural peaks.
- Balanced hormonal protocols yield better results than aggressive stimulation.
Myth: Oxytocin Is the Primary Driver of Peristalsis
While oxytocin plays a supportive role, it is not the primary regulator of uterine contractions. Estradiol remains the dominant hormone, with oxytocin acting as a modulator rather than a driver.
Important distinctions:
- Oxytocin enhances but does not initiate peristalsis.
- Local oxytocin action (autocrine/paracrine) is more critical than systemic administration.
- Excessive oxytocin does not significantly increase contraction frequency.
Conclusion: The Future of Uterine Peristalsis Research
Uterine peristalsis is a dynamic and essential component of female reproductive health. From its hormonal regulation to its clinical implications, understanding these contractions can lead to better fertility outcomes and more effective treatments for conditions like endometriosis and unexplained infertility.
As research advances, integrating AI, modern imaging, and personalized medicine will further illuminate the complexities of uterine function. Clinicians and researchers must continue collaborating to translate these insights into practical, patient-centered solutions.
"The study of uterine peristalsis is not just about contractions—it’s about unlocking the potential for healthier pregnancies and more successful fertility treatments."
By staying informed and embracing innovation, the medical community can ensure that uterine peristalsis remains a cornerstone of reproductive endocrinology and assisted reproductive technologies.
Frederick Banting: Nobel Laureate Who Discovered Insulin
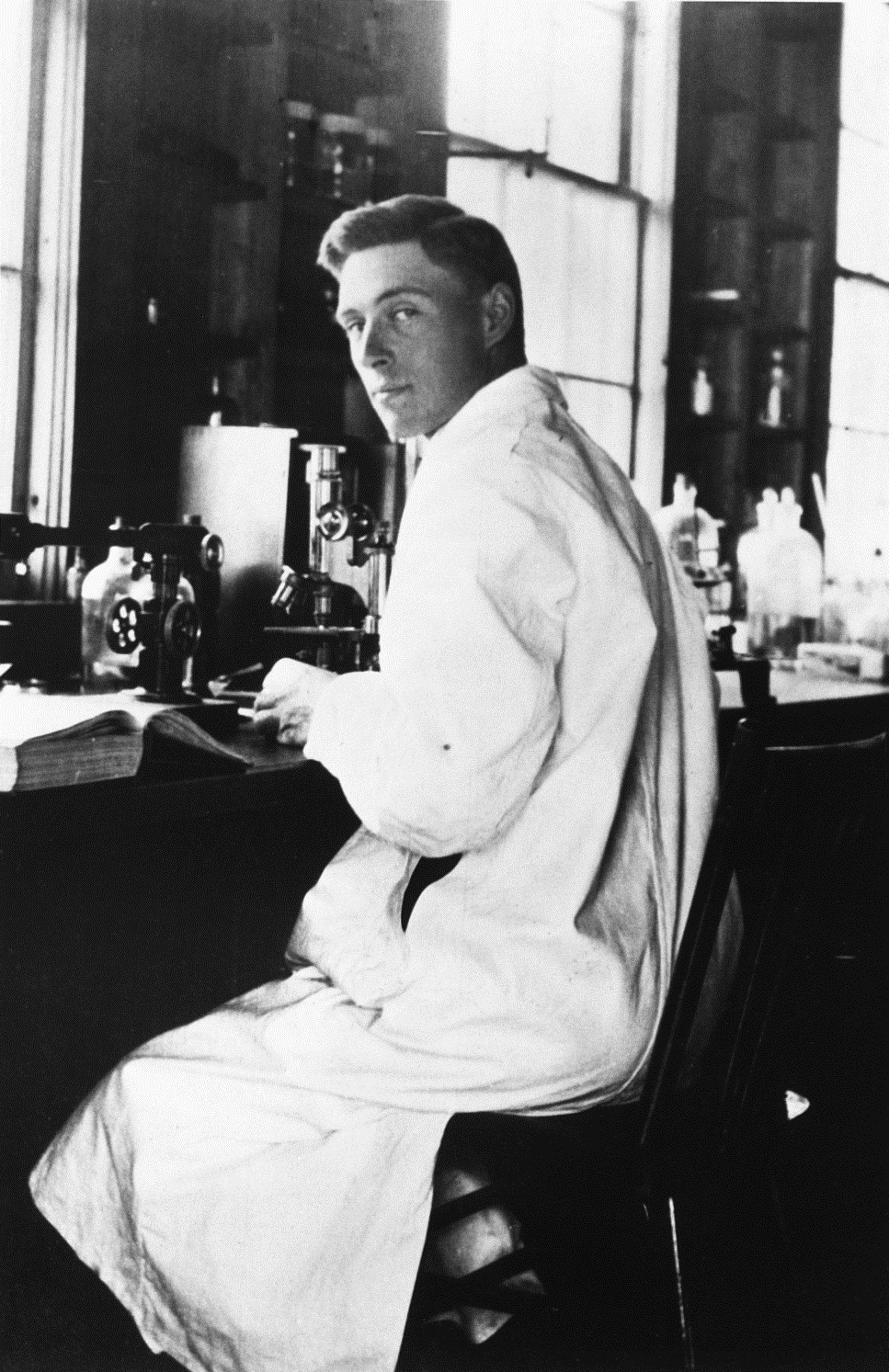
Sir Frederick Grant Banting stands as a monumental figure in medical history. His co-discovery of insulin in the early 1920s transformed a deadly diagnosis into a manageable condition. This article explores his life, his groundbreaking research, and his lasting legacy in diabetes care and beyond.
A Canadian physician and surgeon, Banting's work saved and continues to save millions of lives worldwide. His Nobel Prize-winning achievement at the age of 32 remains one of science's most profound humanitarian breakthroughs. We will delve into the journey that led to this momentous discovery.
Early Life and Path to Medicine
Frederick Banting was born on November 14, 1891, on a farm near Alliston, Ontario. His rural upbringing instilled a strong sense of perseverance and hard work. Initially, he enrolled at Victoria College, University of Toronto, to study divinity and become a minister.
A pivotal change in direction occurred when he transferred to the study of medicine. He graduated in 1916, as World War I raged in Europe. His medical training was accelerated due to the wartime need for physicians. This decision set him on the path that would later change the world.
Service and Injury in World War I
After graduation, Banting immediately joined the Canadian Army Medical Corps. He served as a surgeon in England and later in France. During the Battle of Cambrai in 1918, he displayed exceptional courage while treating wounded soldiers under heavy fire.
Despite being severely wounded in the arm by shrapnel, he continued to care for patients for over sixteen hours. For his heroism, he was awarded the Military Cross, one of the highest military honors. This injury, however, complicated his initial plans for a career as an orthopedic surgeon.
Post-War Medical Practice and Research Idea
After the war, Banting completed his surgical training and began a practice in orthopedic surgery in London, Ontario. He also took a part-time teaching position at the University of Western Ontario. It was while preparing a lecture on the pancreas in October 1920 that a transformative idea struck him.
He read a medical journal article linking pancreatic islets to diabetes. Banting conceived a novel method to isolate the internal secretion of these islets. He famously scribbled his idea in a notebook: "Diabetus. Ligate pancreatic ducts of dog. Keep dogs alive till acini degenerate leaving Islets. Try to isolate the internal secretion of these to relieve glycosurea."
The Historic Discovery of Insulin
Driven by his hypothesis, Banting moved to Toronto in the summer of 1921 to pursue his research. Professor J.J.R. Macleod of the University of Toronto provided laboratory space and resources. Macleod also assigned a young medical student, Charles Best, to assist Banting for the summer.
Their early experiments involved surgically ligating the pancreatic ducts in dogs to degenerate the enzyme-producing cells, leaving the islet cells intact. They then extracted the material from these islets, which they initially called "isletin."
Critical Experiments and Refinement
The team faced numerous challenges and failures. However, by July 30, 1921, they successfully extracted a pancreatic extract that lowered the blood sugar of a diabetic dog. This proved the extract's life-saving potential. The substance was soon renamed insulin.
To purify the extract for human use, biochemist James Collip joined the team later in 1921. His expertise was crucial in refining a sufficiently pure and consistent batch of insulin. This collaborative effort was intense and sometimes fraught with personal tension.
Banting and Best famously sold the insulin patent to the University of Toronto for a symbolic $1, with Banting stating, "Insulin belongs to the world, not to me."
First Human Trial and Immediate Impact
The first human recipient was a 14-year-old boy named Leonard Thompson, who was dying from type 1 diabetes in Toronto General Hospital. The first injection in January 1922 caused an allergic reaction due to impurities. After Collip's further purification, a second injection was administered.
The results were nothing short of miraculous. Thompson's dangerously high blood glucose levels dropped to near-normal ranges. His strength returned, and he gained weight. Leonard Thompson survived, living for another 13 years with insulin therapy, proving the treatment's revolutionary efficacy.
The Nobel Prize and Controversy
In 1923, the Nobel Assembly awarded the Nobel Prize in Physiology or Medicine for the discovery of insulin. The prize was awarded jointly to Frederick Banting and J.J.R. Macleod. This decision immediately sparked controversy, as it overlooked the direct laboratory contributions of Charles Best and James Collip.
Feeling that Best's role was seminal, Banting publicly announced he would share his prize money with his young assistant. Macleod later split his share with Collip. This episode highlights the often-complex nature of attributing credit in scientific discoveries made by teams.
- Youngest Winner: At 32, Banting became the youngest Nobel laureate in Physiology or Medicine at that time.
- First Canadian: He was also the first Canadian to win a Nobel Prize in this category.
- Enduring Debate: Historical accounts continue to analyze the contributions of all four key figures.
The award solidified the importance of insulin on the world stage. It also brought Banting immense fame and pressure. Despite the acclaim, he remained deeply committed to the humanitarian purpose of his work, ensuring affordable access to the life-saving hormone.
Banting's Later Scientific Career and Aviation Medicine
After the whirlwind of the insulin discovery and Nobel Prize, Frederick Banting continued his scientific pursuits with vigor. He was appointed a professor at the University of Toronto and continued medical research. However, his interests expanded significantly beyond endocrinology into new and critical fields.
He dedicated considerable energy to cancer research and the study of silicosis. Banting also maintained his artistic side, taking up painting as a serious hobby. His paintings, often landscapes, provided a creative outlet from his intense scientific work.
Pioneering Contributions to Aviation Medical Research
With the growing threat of World War II, Banting turned his formidable research skills to a national defense priority. In 1939, he was appointed Chairman of Canada's Associate Committee on Aviation Medical Research. He threw himself into this role, focusing on the physiological challenges faced by pilots.
His committee's work was pragmatic and directly aimed at improving pilot safety and performance. Key research areas included the effects of high-altitude flight, oxygen deprivation, and G-forces on the human body. Banting understood that aviation medicine was crucial for Allied air superiority.
- Carbon Monoxide Detection: His team developed improved methods for detecting deadly carbon monoxide in aircraft cabins.
- Protective Eyewear: They pioneered the development of anti-fogging and shatterproof goggles for pilots.
- Early Helmet Design: Research was conducted on protective helmets to mitigate the impact of crashes and turbulence.
- Cold Weather Survival: Studies focused on the physiology of survival in extreme cold for downed airmen.
This work established a foundation for Canadian expertise in aerospace medicine that continues to this day. Banting's ability to pivot from a laboratory-focused researcher to a leader in applied military science demonstrated his versatility and deep patriotism.
The Tragic Death of a National Hero
Frederick Banting's life was cut short on February 21, 1941. He was en route to England aboard a Lockheed Hudson bomber to deliver crucial research findings and discuss wartime collaboration in aviation medicine. The plane crashed shortly after takeoff from Gander, Newfoundland, killing Banting and two other crew members instantly.
The pilot, Captain Joseph Mackey, survived the crash and later recounted that Banting, though seriously injured, helped him escape the wreckage before succumbing to his own injuries. This final act of heroism was consistent with Banting's character, evidenced decades earlier on the battlefields of WWI.
Banting's death at age 49 was mourned across Canada and the scientific world as a profound loss. Prime Minister Mackenzie King called him "one of Canada's greatest sons," and he was given a state funeral in Toronto.
The Enduring Legacy of His Final Mission
His mission to England underscored the strategic importance he placed on his aviation research. The work of his committee directly contributed to the safety and effectiveness of Allied air crews throughout the war. While the insulin discovery defined his public legacy, his contributions to wartime science were a significant second act.
The crash site remains a place of historical significance. A memorial was later erected near Musgrave Harbour, Newfoundland. His death highlighted the risks taken by scientists and personnel during the war, even those not on the front lines of direct combat.
Frederick Banting's Legacy and Honors
Frederick Banting's legacy is multifaceted, encompassing medical innovation, national pride, and ongoing scientific inspiration. His name is synonymous with one of the most important medical breakthroughs of the 20th century. This legacy is preserved through numerous honors, institutions, and continued public remembrance.
In Canada, he is celebrated as a national hero. His image appeared on the Canadian $100 bill for many years until the series was redesigned. This prominent placement on the banknote was a testament to his status as a figure of monumental national importance.
Institutions and Memorials
Several major institutions bear his name, ensuring his contributions are never forgotten. The Banting and Best Department of Medical Research at the University of Toronto continues his tradition of inquiry. Banting House in London, Ontario, where he had his crucial idea, is now a National Historic Site of Canada and museum dubbed "The Birthplace of Insulin."
Furthermore, the Banting Research Foundation was established to fund innovative health research in Canada. World Diabetes Day, observed on November 14th, is held on his birthday, creating a permanent global link between his legacy and the ongoing fight against the disease.
- Banting Postdoctoral Fellowships: Prestigious Canadian government awards for top-tier researchers.
- Statues and Plaques: Numerous public memorials exist across Canada, including at the University of Toronto and the Parliament of Canada.
- International Recognition: He was knighted by King George V in 1934, becoming Sir Frederick Banting.
The Centennial of Insulin and Modern Reflections
The year 2021 marked the 100th anniversary of Banting and Best's initial successful experiments. This centennial was commemorated worldwide by diabetes organizations, research institutions, and patient communities. It was a moment to reflect on how far treatment has come and the distance still to go.
The University of Toronto and other institutions hosted special events, publications, and exhibitions. These highlighted not only the historical discovery but also its modern implications. The centennial underscored insulin as a starting point, not an endpoint, in diabetes care.
From Animal Extract to Modern Analogs
The insulin Banting's team extracted from dogs and later cows was life-saving but imperfect. It was relatively short-acting and could cause immune reactions. Today, thanks to genetic engineering, we have human insulin and advanced analogs.
Modern synthetic insulins offer precise action profiles—rapid-acting, long-acting, and premixed varieties. This allows for much tighter and more flexible blood glucose management. Delivery methods have also evolved dramatically from syringes to insulin pumps and continuous glucose monitors.
Despite these advancements, the core principle Banting proved—that replacing the missing hormone could treat diabetes—remains the bedrock of therapy for millions with type 1 diabetes worldwide.
Ongoing Challenges and Access to Medicine
A central theme of the 2021 reflections was Banting's humanitarian ethos. His decision to sell the patent for $1 was a conscious effort to ensure broad, affordable access. This stands in stark contrast to modern controversies over the high cost of insulin in some countries, particularly the United States.
Advocates often invoke Banting's original intent in campaigns for drug pricing reform. The centennial served as a reminder that the moral imperative of accessibility is as important as the scientific breakthrough itself. Ensuring all who need insulin can afford it is viewed by many as fulfilling Banting's vision.
Recent articles from institutions like the University of Toronto have also revisited his lesser-known legacy in aviation medicine. This has brought a more complete picture of his scientific career to public attention, showcasing his versatility and commitment to applying science to urgent human problems, whether chronic disease or wartime survival.
The Team Behind the Discovery: Collaboration and Controversy
The story of insulin’s discovery is a powerful case study in scientific collaboration and its attendant complexities. While Frederick Banting is the most famous name associated with insulin, he worked within a talented team. The roles of Charles Best, J.J.R. Macleod, and James Collip were all indispensable to the final success.
Banting provided the initial hypothesis and relentless drive, while Best executed the day-to-day experiments with skill and dedication. Macleod provided the essential institutional support, laboratory resources, and broader physiological expertise. Collip’s biochemical prowess was critical for purifying the extract for human use.
Analyzing the Nobel Prize Decision
The Nobel Committee's 1923 decision to award the prize only to Banting and Macleod remains a subject of historical debate. This choice reflected the scientific conventions of the era, which often credited the senior supervising scientist and the principal ideator. The contributions of junior researchers like Best and specialists like Collip were frequently overlooked.
Banting’s immediate and public decision to share his prize money with Best was a clear acknowledgment of this perceived injustice. Similarly, Macleod shared his portion with Collip. This action speaks to the internal acknowledgment within the team that the discovery was a collective achievement.
- Banting's Role: Vision, surgical skill, and determination.
- Best's Role: Technical execution of experiments and data collection.
- Macleod's Role: Supervision, resources, and scientific guidance.
- Collip's Role: Biochemical purification for clinical application.
Modern historical analysis tends to recognize the "Toronto Four" as the complete team behind the discovery. This nuanced view honors the collaborative nature of modern scientific breakthroughs, where diverse expertise is essential for turning an idea into a life-saving therapy.
Banting's Personal Life and Character
Beyond the laboratory, Frederick Banting was a man of strong character, humility, and diverse interests. He was known for his straightforward manner, resilience, and a deep sense of duty. These personal qualities profoundly shaped his scientific and medical career.
He married twice, first to Marion Robertson in 1924, with whom he had one son, William. The marriage ended in divorce in 1932. He later became engaged to Henrietta Ball, who was with him in Newfoundland before his final flight. His personal life, however, was often secondary to his consuming dedication to his work.
The Artist and the Scientist
Banting found a creative counterbalance to his scientific work in painting. He was a skilled amateur artist who took his painting seriously, studying under prominent Canadian artists like A.Y. Jackson of the Group of Seven. His landscapes demonstrate a keen eye for detail and a love for the Canadian wilderness.
This artistic pursuit was not merely a hobby; it was a refuge. It provided a mental space for reflection and a different mode of seeing the world. The combination of scientific rigor and artistic sensitivity made him a uniquely rounded individual, showing that creativity fuels innovation across disciplines.
Colleagues noted that Banting was intensely focused and could be stubborn, but he was also generous and deeply committed to the humanitarian application of science, famously forgoing vast wealth to ensure insulin reached those in need.
The Global Impact of Insulin on Diabetes Treatment
The introduction of insulin marked a paradigm shift in medicine. Before 1922, a diagnosis of type 1 diabetes was a virtual death sentence, particularly for children. Patients were subjected to starvation diets that only prolonged life for a short, miserable period.
Insulin therapy transformed this bleak reality almost overnight. It was the first effective treatment for a chronic endocrine disease, proving that hormone replacement could successfully manage a previously fatal condition. This paved the way for subsequent hormone therapies.
From Survival to Thriving: The Evolution of Diabetes Management
The initial goal of insulin therapy was simple survival. Today, the objectives are vastly more ambitious: enabling people with diabetes to live long, healthy, and fulfilling lives. Advances built upon Banting’s work have made this possible.
Modern diabetes care focuses on tight glycemic control to prevent complications such as heart disease, kidney failure, and blindness. Technology like continuous glucose monitors (CGMs) and insulin pumps allows for unprecedented precision in management. These tools represent the ongoing evolution of Banting’s foundational discovery.
- Increased Lifespan: Life expectancy for people with type 1 diabetes has increased by decades.
- Quality of Life: Modern regimens allow for greater dietary flexibility and physical activity.
- Ongoing Research: Work continues on islet cell transplantation, artificial pancreases, and ultimately, a cure.
Banting's Legacy in Modern Medical Research
Frederick Banting’s legacy extends far beyond the molecule of insulin. His story continues to inspire new generations of researchers, physicians, and students. He embodies the ideal of the physician-scientist who moves seamlessly from patient-oriented questions to fundamental laboratory investigation.
Research institutions that bear his name, like the Banting and Best Department of Medical Research, continue to operate at the forefront of biomedical science. The Banting Postdoctoral Fellowships are among Canada’s most prestigious awards, attracting top scientific talent from around the world to conduct research in the country.
Lessons for Today's Scientists
Banting’s career offers several enduring lessons. It demonstrates the power of a simple, well-defined idea pursued with tenacity. It highlights the critical importance of collaboration across different specialties. Most importantly, it shows that scientific achievement is fundamentally connected to human benefit.
His decision regarding the insulin patent remains a powerful ethical benchmark. In an era of biotechnology and pharmaceutical commerce, Banting’s stance that a life-saving discovery "belongs to the world" challenges us to balance innovation with accessibility and equity.
Conclusion: The Enduring Significance of Frederick Banting
Frederick Banting’s life was a remarkable journey from a rural Ontario farm to the pinnacle of scientific achievement. His co-discovery of insulin stands as one of the most transformative events in the history of medicine. It turned a deadly disease into a manageable condition and gave hope to millions.
His legacy is not confined to a single discovery. His heroic service in two world wars, his pioneering work in aviation medicine, and his artistic pursuits paint a portrait of a complex and multifaceted individual. Banting was a national hero who embodied perseverance, ingenuity, and profound humanity.
The story of insulin is ongoing. While Banting and his team provided the key that unlocked the door, scientists continue to build upon their work, striving for better treatments and a ultimate cure. The centennial celebrations in 2021 were not just about honoring the past but also about reinforcing commitment to the future of diabetes care.
Frederick Banting’s greatest legacy is the breath of life he gave to countless individuals and the enduring inspiration he provides to all who seek to use science as a force for good. His work reminds us that dedicated individuals can indeed change the world.
In remembering Sir Frederick Banting, we celebrate more than a historical figure; we celebrate the very ideal of scientific progress in the service of humanity. His life continues to inspire a simple, powerful truth: that curiosity, coupled with compassion, can conquer some of humanity’s most daunting challenges.


Rosalyn Yalow: Nobel Prize-Winning Scientist Who Revolutionized Medicine
Rosalyn Yalow was a pioneering medical physicist whose groundbreaking work transformed modern medicine. Her co-development of radioimmunoassay (RIA) earned her the 1977 Nobel Prize in Physiology or Medicine, making her the second woman and first American-born woman to receive this prestigious honor. This revolutionary technique allowed scientists to measure minuscule quantities of biological substances, paving the way for advancements in diagnostics, hormone research, and disease detection.
Early Life and Education
Rosalyn Sussman Yalow was born on July 19, 1921, in the Bronx, New York. From an early age, she exhibited a keen interest in science and mathematics, despite the societal barriers that women faced in pursuing scientific careers during the 1940s. Her determination led her to Hunter College, where she earned her bachelor's degree in 1941 and her master's degree in 1942.
Yalow's academic journey continued at the University of Illinois, where she obtained her PhD in nuclear physics in 1945. Her graduate studies were marked by perseverance, as she often encountered discrimination due to her gender. Despite these challenges, she excelled in her field, laying the foundation for her future contributions to medical science.
The Development of Radioimmunoassay (RIA)
In 1950, Yalow began her collaboration with physician Solomon Berson at the Bronx VA Hospital. Together, they embarked on a journey that would revolutionize medical diagnostics. Their work focused on using radioactive iodine to trace insulin and detect antibodies in diabetic patients, leading to the development of radioimmunoassay (RIA).
RIA is a highly sensitive technique capable of detecting substances at picogram levels, equivalent to finding a teaspoon of sugar in a 62-mile-long body of water. This breakthrough enabled the precise measurement of hormones, drugs, viruses, enzymes, vitamins, and over 100 other biological substances, transforming the fields of endocrinology, oncology, and virology.
The Impact of RIA on Medicine
The introduction of RIA had a profound impact on medical research and diagnostics. It allowed scientists to study hormones and other biological substances with unprecedented accuracy, leading to a deeper understanding of diseases such as diabetes and thyroid disorders. Yalow and Berson's work revealed that type II diabetes involves antibodies rejecting insulin, rather than a deficiency of the hormone itself.
This discovery shifted the paradigm of diabetes research and opened new avenues for treatment and management. RIA's sensitivity and versatility made it an indispensable tool in clinical laboratories worldwide, enabling breakthroughs in hormone research, drug monitoring, and disease detection.
Awards and Recognition
Yalow's contributions to science were widely recognized, earning her numerous accolades throughout her career. In 1977, she was awarded the Nobel Prize in Physiology or Medicine, which she shared with Roger Guillemin and Andrew Schally. This historic achievement made her the second woman and the first American-born woman to receive the Nobel Prize in this category.
In addition to the Nobel Prize, Yalow received the Albert Lasker Basic Medical Research Award in 1976, becoming the first woman and nuclear physicist to be honored with this prestigious award. She was also awarded the National Medal of Science in 1988 and was elected to the National Academy of Sciences in 1975.
A Legacy of Accessibility and Mentorship
Despite the commercial potential of RIA, Yalow and Berson chose not to patent their discovery. Their decision was driven by a commitment to making the technique accessible to researchers and clinicians worldwide, ensuring that its benefits could be widely shared. This selfless act underscored Yalow's dedication to advancing science for the betterment of humanity.
Throughout her career, Yalow was a passionate advocate for women in science. She mentored numerous young researchers and served on various advisory boards, inspiring future generations of scientists to pursue their passions despite the challenges they might face.
Conclusion
Rosalyn Yalow's legacy as a trailblazer in medical physics and a champion for women in STEM continues to inspire scientists around the world. Her development of radioimmunoassay (RIA) revolutionized the field of medicine, enabling precise measurements of biological substances and advancing our understanding of diseases. Yalow's numerous awards and accolades, including the Nobel Prize in Physiology or Medicine, are a testament to her groundbreaking contributions and her enduring impact on science and society.
Overcoming Gender Barriers in Science
Rosalyn Yalow faced significant challenges as a woman in the male-dominated field of science during the 1940s and 1950s. Despite her exceptional academic record, she was denied teaching assistantships due to her gender. This discrimination did not deter her; instead, it fueled her determination to succeed. Yalow's perseverance in the face of adversity serves as an inspiration to women in STEM (Science, Technology, Engineering, and Mathematics) fields.
During World War II, Yalow took advantage of the shortage of male scientists to pursue her studies in physics. She equipped a radioisotope lab in a former janitor's closet at the Bronx VA Hospital, demonstrating her resourcefulness and dedication to her work. This humble beginning laid the groundwork for her groundbreaking research in collaboration with Solomon Berson.
Breaking the Glass Ceiling
Yalow's achievements shattered the glass ceiling for women in science. She became the first woman to win the Albert Lasker Basic Medical Research Award in 1976 and the second woman to receive the Nobel Prize in Physiology or Medicine in 1977. Her success paved the way for future generations of women scientists, proving that gender should not be a barrier to scientific excellence.
Throughout her career, Yalow advocated for equal opportunities for women in science. She mentored numerous young researchers, encouraging them to pursue their passions and overcome the challenges they faced. Her legacy as a trailblazer for women in STEM continues to inspire and empower women around the world.
The Science Behind Radioimmunoassay (RIA)
Radioimmunoassay (RIA) is a highly sensitive technique that combines the principles of immunology and nuclear physics. Developed by Yalow and Berson, RIA uses radioactive isotopes to measure the concentration of biological substances in the body. This innovative method allows for the detection of substances at picogram levels, making it an invaluable tool in medical research and diagnostics.
The process of RIA involves several key steps:
- A radioactive tracer is introduced into a sample containing the substance to be measured.
- The tracer binds to specific antibodies, forming a complex that can be detected and quantified.
- The amount of radioactivity in the sample is measured, allowing researchers to determine the concentration of the substance.
Applications of RIA in Medicine
RIA has a wide range of applications in medicine, including:
- Hormone research: RIA enables the precise measurement of hormones such as insulin, thyroid hormones, and growth hormones, leading to a deeper understanding of endocrine disorders.
- Drug monitoring: The technique is used to monitor the levels of therapeutic drugs in the body, ensuring optimal dosing and minimizing side effects.
- Disease detection: RIA plays a crucial role in the diagnosis of diseases such as diabetes, thyroid disorders, and certain types of cancer.
- Viral and bacterial detection: RIA can be used to detect the presence of viruses and bacteria in the body, aiding in the diagnosis and treatment of infectious diseases.
Yalow's Collaboration with Solomon Berson
Yalow's collaboration with Solomon Berson was a pivotal aspect of her scientific journey. The two researchers began working together at the Bronx VA Hospital in 1950, focusing on the study of insulin and its role in diabetes. Their partnership led to the development of radioimmunoassay (RIA), a technique that would revolutionize the field of medicine.
Berson, a physician, brought a clinical perspective to their research, while Yalow's expertise in nuclear physics provided the technical foundation for their work. Together, they equipped a radioisotope lab in a former janitor's closet, demonstrating their resourcefulness and dedication to their research. Their collaboration was marked by a shared commitment to advancing medical science and improving patient care.
The Tragic Loss of Solomon Berson
Unfortunately, Solomon Berson passed away in 1972, six years before Yalow received the Nobel Prize for their joint work. Due to the Nobel Committee's policy of not awarding the prize posthumously, Berson was not recognized with the honor. This was a significant loss for the scientific community, as Berson's contributions to the development of RIA were invaluable.
Despite this tragedy, Yalow continued her research and mentored young scientists, ensuring that Berson's legacy lived on. She often acknowledged his crucial role in their groundbreaking work, emphasizing the importance of their collaboration in the development of RIA.
The Evolution of Immunoassays
While radioimmunoassay (RIA) remains a foundational technique in medical research, it has evolved over the years to address safety concerns and improve efficiency. One notable advancement is the development of enzyme-linked immunosorbent assay (ELISA), a non-radioactive alternative to RIA. ELISA uses enzymes instead of radioactive isotopes to detect and quantify biological substances, making it a safer and more accessible option for clinical laboratories.
The principles of RIA have also been adapted to create other immunoassay techniques, such as fluorescence immunoassay (FIA) and chemiluminescence immunoassay (CLIA). These techniques offer enhanced sensitivity and specificity, further expanding the applications of immunoassays in medicine.
The Enduring Legacy of RIA
Despite the emergence of new immunoassay techniques, the principles of RIA continue to underpin modern diagnostics. The technique's sensitivity and versatility have made it an indispensable tool in clinical laboratories worldwide. RIA has enabled breakthroughs in hormone research, drug monitoring, and disease detection, improving the lives of countless patients.
Yalow's pioneering work in the development of RIA has left an enduring legacy in the field of medicine. Her contributions have not only advanced our understanding of diseases but have also paved the way for the development of new diagnostic tools and treatments. As a result, RIA remains a cornerstone of medical research and diagnostics, testament to Yalow's groundbreaking achievements.
Yalow's Impact on Diabetes Research
One of the most significant applications of radioimmunoassay (RIA) has been in the field of diabetes research. Yalow and Berson's work on insulin and antibodies in diabetic patients led to a deeper understanding of the disease. Their research revealed that type II diabetes involves antibodies rejecting insulin, rather than a deficiency of the hormone itself. This discovery shifted the paradigm of diabetes research and opened new avenues for treatment and management.
RIA has enabled researchers to measure insulin levels with unprecedented accuracy, leading to a better understanding of the disease's underlying mechanisms. This has facilitated the development of new therapies and improved the management of diabetes, ultimately enhancing the quality of life for millions of patients worldwide.
Advancements in Diabetes Diagnostics
The impact of RIA on diabetes diagnostics cannot be overstated. The technique has allowed for the early detection and monitoring of the disease, enabling healthcare providers to intervene promptly and effectively. Some of the key advancements in diabetes diagnostics made possible by RIA include:
- Improved insulin assays: RIA has enabled the development of highly sensitive insulin assays, allowing for the precise measurement of insulin levels in the body.
- Enhanced glucose monitoring: The technique has facilitated the development of advanced glucose monitoring systems, helping patients manage their blood sugar levels more effectively.
- Early detection of complications: RIA has played a crucial role in the early detection of diabetes-related complications, such as kidney disease and nerve damage, enabling timely intervention and treatment.
Yalow's Role as a Mentor and Advocate
Throughout her career, Rosalyn Yalow was a passionate advocate for women in science. She recognized the importance of mentorship and actively mentored numerous young researchers, encouraging them to pursue their passions and overcome the challenges they faced. Her dedication to fostering the next generation of scientists has left a lasting impact on the scientific community.
Yalow's mentorship extended beyond her immediate circle of colleagues. She served on various advisory boards and committees, working to promote equal opportunities for women in science. Her efforts have inspired countless women to pursue careers in STEM fields, breaking down barriers and shattering stereotypes.
Inspiring Future Generations
Yalow's legacy as a mentor and advocate for women in science continues to inspire future generations. Her story serves as a powerful reminder of the importance of perseverance, dedication, and passion in the face of adversity. By sharing her experiences and offering guidance to young scientists, Yalow has empowered countless individuals to pursue their dreams and make meaningful contributions to the world of science.
Today, numerous initiatives and programs aim to support women in STEM fields, building on the foundation laid by pioneers like Rosalyn Yalow. These efforts are a testament to her enduring impact and the ongoing importance of her work in promoting gender equality in science.
Yalow's Later Years and Retirement
After decades of groundbreaking research, Rosalyn Yalow continued her work until her retirement in 1991. She held the position of Distinguished Service Professor at Mount Sinai, where she remained actively involved in research and mentorship. Even in her later years, Yalow's passion for science and her commitment to advancing medical knowledge never wavered.
Yalow's retirement did not mark the end of her influence in the scientific community. She continued to serve on advisory boards and participate in scientific conferences, sharing her insights and expertise with colleagues and young researchers alike. Her dedication to the field of medical physics and her unwavering commitment to mentorship left an indelible mark on the scientific community.
Legacy in the Bronx VA Hospital
The Bronx VA Hospital, where Yalow and Berson conducted their pioneering research, remains a testament to their legacy. The hospital's radioisotope lab, initially set up in a former janitor's closet, evolved into a state-of-the-art facility under Yalow's leadership. Today, the hospital continues to be a hub for medical research and innovation, inspired by Yalow's groundbreaking work.
Yalow's contributions to the Bronx VA Hospital extended beyond her scientific achievements. She was a beloved figure among her colleagues and patients, known for her compassion, dedication, and unwavering commitment to improving patient care. Her legacy at the hospital serves as a reminder of the profound impact that one individual can have on the field of medicine.
Honors and Tributes
Throughout her lifetime and posthumously, Rosalyn Yalow received numerous honors and tributes in recognition of her groundbreaking contributions to science. These accolades serve as a testament to her enduring impact on the field of medicine and her role as a trailblazer for women in STEM.
Some of the most notable honors and tributes include:
- Nobel Prize in Physiology or Medicine (1977): Awarded for her co-development of radioimmunoassay (RIA), this prestigious honor made Yalow the second woman and first American-born woman to receive the prize in this category.
- Albert Lasker Basic Medical Research Award (1976): Yalow was the first woman and nuclear physicist to receive this award, recognizing her pioneering work in the development of RIA.
- National Medal of Science (1988): This honor, bestowed by the President of the United States, recognized Yalow's outstanding contributions to the field of medical physics.
- Election to the National Academy of Sciences (1975): Yalow's election to this prestigious organization underscored her significant impact on the scientific community.
- Posthumous tributes: In the years following her passing, Yalow has been celebrated in numerous articles, documentaries, and scientific conferences, highlighting her enduring legacy and contributions to medicine.
Recent Recognitions
Even years after her passing, Rosalyn Yalow continues to be celebrated for her groundbreaking work. Recent tributes, such as those in 2024–2025 articles, have highlighted her role in the history of diabetes research and her impact as a woman in science. These recognitions serve as a reminder of Yalow's enduring influence and the ongoing relevance of her contributions to the field of medicine.
One notable example is the inclusion of Yalow's story in the "Pioneers of Progress" series, which celebrates the achievements of trailblazing scientists. This series, published in prominent scientific journals, has brought Yalow's work to the attention of new generations of researchers, ensuring that her legacy continues to inspire and empower future scientists.
The Global Impact of Yalow's Work
The impact of Rosalyn Yalow's work extends far beyond the borders of the United States. Her development of radioimmunoassay (RIA) has had a profound effect on medical research and diagnostics worldwide. The technique's sensitivity and versatility have made it an indispensable tool in clinical laboratories across the globe, enabling breakthroughs in hormone research, drug monitoring, and disease detection.
Yalow's work has particularly influenced the field of endocrinology, where RIA has become a standard technique for measuring hormone levels. This has led to a deeper understanding of endocrine disorders and the development of more effective treatments. Additionally, RIA has played a crucial role in the diagnosis and management of diseases such as diabetes, thyroid disorders, and certain types of cancer.
Influencing International Research
Yalow's contributions have inspired researchers around the world to build upon her work and develop new diagnostic tools. The principles of RIA have been adapted to create a variety of immunoassay techniques, such as enzyme-linked immunosorbent assay (ELISA) and chemiluminescence immunoassay (CLIA). These techniques, which offer enhanced sensitivity and safety, are now widely used in clinical laboratories worldwide.
The global impact of Yalow's work is also evident in the numerous scientific collaborations and partnerships that have emerged as a result of her research. Scientists from diverse backgrounds and disciplines have come together to advance the field of medical diagnostics, driven by the foundation laid by Yalow's pioneering work.
Yalow's Personal Life and Values
Beyond her scientific achievements, Rosalyn Yalow was known for her strong personal values and her commitment to making a difference in the world. She was a devoted wife and mother, balancing her demanding career with her family life. Yalow's ability to excel in both her professional and personal life serves as an inspiration to women everywhere, demonstrating that it is possible to achieve greatness in multiple aspects of life.
Yalow's values were deeply rooted in her belief in the power of science to improve human lives. She was a firm advocate for the accessibility of scientific knowledge and techniques, as evidenced by her decision not to patent RIA. This selfless act ensured that the benefits of her groundbreaking work could be widely shared, ultimately improving the lives of countless patients worldwide.
A Life of Integrity and Humility
Throughout her career, Yalow remained humble and grounded, despite her numerous accolades and achievements. She was known for her integrity, her dedication to her work, and her unwavering commitment to the betterment of humanity. Yalow's personal life and values serve as a powerful reminder of the importance of maintaining a strong moral compass, even in the face of great success.
Yalow's legacy is not only defined by her scientific contributions but also by her character and the values she upheld. Her life story is a testament to the power of perseverance, dedication, and humility, inspiring future generations to strive for excellence in both their professional and personal lives.
Conclusion: Rosalyn Yalow's Enduring Legacy
Rosalyn Yalow's life and work have left an indelible mark on the field of medicine and the scientific community as a whole. Her co-development of radioimmunoassay (RIA) revolutionized medical diagnostics, enabling the precise measurement of biological substances and advancing our understanding of diseases. Yalow's numerous awards and accolades, including the Nobel Prize in Physiology or Medicine, are a testament to her groundbreaking contributions and her enduring impact on science and society.
Yalow's legacy extends beyond her scientific achievements. She was a trailblazer for women in STEM, shattering the glass ceiling and paving the way for future generations of women scientists. Her commitment to mentorship and her advocacy for equal opportunities in science have inspired countless individuals to pursue their passions and overcome the challenges they face.
Key Takeaways from Yalow's Life and Work
As we reflect on Rosalyn Yalow's remarkable life and career, several key takeaways emerge:
- Perseverance in the face of adversity: Yalow's ability to overcome gender barriers and achieve greatness serves as an inspiration to women in science and beyond.
- The power of collaboration: Yalow's partnership with Solomon Berson demonstrates the importance of interdisciplinary collaboration in driving scientific innovation.
- A commitment to accessibility: Yalow's decision not to patent RIA underscores her belief in the importance of making scientific knowledge and techniques accessible to all.
- The impact of mentorship: Yalow's dedication to mentoring young researchers highlights the crucial role that mentorship plays in fostering the next generation of scientists.
- The enduring legacy of scientific innovation: Yalow's work continues to inspire and influence researchers worldwide, demonstrating the lasting impact of groundbreaking scientific discoveries.
In conclusion, Rosalyn Yalow's story is one of perseverance, dedication, and unwavering commitment to the betterment of humanity. Her groundbreaking work in the development of radioimmunoassay has transformed the field of medicine, enabling advancements in diagnostics, hormone research, and disease detection. Yalow's legacy as a trailblazer for women in STEM and her enduring impact on the scientific community serve as a powerful reminder of the importance of pursuing one's passions and striving for excellence, even in the face of adversity. As we continue to build upon her pioneering work, we honor Rosalyn Yalow's memory and celebrate her remarkable contributions to science and society.
Revolutionary Scientist in Endocrinology: Unraveling the Mystery
In the vast and ever-evolving field of endocrinology, scientists and researchers continuously push the boundaries of medical knowledge. However, the search for a revolutionary scientist in endocrinology named Rozalin Gialooy H. presents a unique challenge. Despite extensive research across major academic databases, Greek university repositories, and medical literature, there is no widely recognized figure or publication that matches this exact name or description. This article delves into the intricacies of this query, exploring potential interpretations and providing actionable insights for those seeking information on groundbreaking contributions in endocrinology.
Understanding the Query: Rozalin Gialooy H.
The name Rozalin Gialooy H. appears to be a combination of a personal name and an initial, possibly followed by a descriptor in Greek. The phrase "Επαναστατική Επιστήμονας στην Ενδοκρινολογία" translates to "revolutionary scientist in endocrinology." This suggests that the query might be referring to an individual who has made significant, perhaps groundbreaking, contributions to the field of endocrinology.
The Challenge of Verification
One of the primary challenges in addressing this query is the lack of verifiable information. Extensive searches across PubMed, Greek university websites, and other academic databases have yielded no results that match the name Rozalin Gialooy H. or the associated descriptor. This absence of information raises several questions:
- Is the name spelled correctly?
- Could there be alternative spellings or transliterations?
- Is the individual perhaps known by a different name in academic circles?
Potential Interpretations
Given the lack of direct matches, several interpretations of the query are possible:
- Interpretation A: The query is intended to find a specific person—a scientist named Rozalin (or Rozalyn) Gialooy (or GialooY) with the middle initial H—described in Greek as a "revolutionary scientist in endocrinology."
- Interpretation B: The query may be an attempt to transliterate or translate a non-Greek name into Greek and append a descriptor. Spelling or transliteration errors could be hiding potential matches.
- Interpretation C: The phrase might be the title of a blog post, book chapter, or niche article that is not indexed by major search engines or literature databases.
The Importance of Accurate Information in Endocrinology
Endocrinology is a critical field of medicine that deals with hormones and the endocrine system, impacting various aspects of human health, from metabolism to reproduction. Accurate information and verified contributions are essential for advancing research and improving patient outcomes. When searching for information on revolutionary scientists in endocrinology, it is crucial to rely on authoritative sources and verified data.
Authoritative Sources in Endocrinology
For those seeking information on groundbreaking contributions in endocrinology, several authoritative sources can provide reliable data:
- PubMed: A comprehensive database of biomedical literature, including research articles, reviews, and clinical studies.
- University Websites: Many universities have dedicated endocrinology departments with detailed information on faculty, research, and publications.
- Endocrinology Societies: Organizations such as the Endocrine Society and the European Society of Endocrinology provide resources and publications on the latest advancements in the field.
- World Health Organization (WHO): Offers global health statistics and reports on endocrine-related conditions.
Key Statistics and Data Points
To provide context and credibility, it is helpful to include relevant statistics and data points. For example:
- According to the World Health Organization (WHO), diabetes affects over 422 million people worldwide, highlighting the importance of endocrinological research in managing this condition.
- The International Diabetes Federation (IDF) reports that approximately 1 in 11 adults has diabetes, underscoring the global impact of endocrine disorders.
- Research published in PubMed indicates that advancements in endocrinology, such as the development of GLP-1 receptor agonists, have significantly improved the management of type 2 diabetes.
Exploring Alternative Spellings and Transliterations
Given the potential for spelling or transliteration errors, it is worthwhile to explore alternative versions of the name Rozalin Gialooy H.. Common variations might include:
- Rozalyn Gialooy H.
- Rosalyn Gialooy H.
- Rozalin Gialloy H.
- Rozalin Yialooy H.
- Rozalin Yiallou H.
Searching these variations across different databases and languages could potentially yield matches that were previously overlooked. Additionally, considering the original script of the name, if it is not in Greek or English, could provide further clarity.
Searching Beyond Major Databases
If the name or phrase is not found in major academic databases, it may be necessary to expand the search to include:
- Greek News Archives: Local news sources may have articles or mentions of the individual.
- Social Media Platforms: Professionals often share their work and achievements on platforms like LinkedIn, ResearchGate, or academic blogs.
- Institutional Repositories: Some universities and research institutions have their own repositories that may not be indexed by major search engines.
Creating SEO-Optimized Content on Revolutionary Scientists in Endocrinology
For content creators and SEO professionals, the lack of verifiable information on Rozalin Gialooy H. presents an opportunity to focus on well-documented figures and advancements in endocrinology. Creating SEO-optimized content that highlights verified contributions can attract a wider audience and provide valuable insights.
Key Elements of SEO-Optimized Content
To ensure that content ranks well in search engines and provides value to readers, consider the following elements:
- Keyword Research: Identify relevant keywords and phrases, such as "revolutionary scientists in endocrinology," "groundbreaking endocrinology research," and "pioneers in hormone research."
- High-Quality Sources: Use authoritative sources like PubMed, university websites, and endocrinology societies to provide accurate and up-to-date information.
- Engaging Headlines: Craft compelling headlines that include target keywords and spark curiosity.
- Structured Content: Use clear headings (H1, H2, H3) and bullet points to improve readability and scannability.
- Internal and External Links: Link to relevant internal pages and external authoritative sources to enhance credibility and SEO.
Example Outline for an SEO Article
Here is an example outline for an article on revolutionary scientists in endocrinology:
- Introduction: Briefly introduce the importance of endocrinology and the impact of revolutionary scientists.
- Historical Pioneers: Highlight key figures in the history of endocrinology, such as Frederick Banting and Charles Best, who discovered insulin.
- Modern Innovators: Discuss contemporary scientists and researchers who have made significant contributions to the field.
- Groundbreaking Discoveries: Explore major advancements in endocrinology, such as the development of hormone replacement therapies and new diabetes treatments.
- Future Directions: Examine emerging trends and technologies in endocrinology, such as gene therapy and personalized medicine.
- Conclusion: Summarize the impact of revolutionary scientists and the importance of continued research in endocrinology.
Conclusion: Navigating the Search for Information
The search for Rozalin Gialooy H. as a revolutionary scientist in endocrinology highlights the challenges of verifying information in a specialized field. While the exact name and descriptor do not yield direct matches in major databases, exploring alternative spellings, transliterations, and niche sources may provide additional insights. For content creators, focusing on verified figures and advancements in endocrinology can result in high-quality, SEO-optimized content that resonates with readers and ranks well in search engines.
In the next part of this article, we will delve deeper into the historical pioneers and modern innovators in endocrinology, providing a comprehensive overview of the field's most influential figures and their contributions.
Historical Pioneers in Endocrinology
Endocrinology, the study of hormones and their impact on the body, has been shaped by numerous groundbreaking scientists. These pioneers in endocrinology laid the foundation for modern research and treatments, revolutionizing our understanding of hormonal disorders and their management.
Frederick Banting and Charles Best: The Discovery of Insulin
One of the most significant milestones in endocrinology was the discovery of insulin by Frederick Banting and Charles Best in 1921. This breakthrough transformed the treatment of diabetes, a condition that was previously fatal. Banting and Best's work at the University of Toronto led to the development of insulin therapy, which remains a cornerstone of diabetes management today.
"Insulin is not a cure for diabetes; it is a treatment. It enables the diabetic to burn sufficient carbohydrates, so that proteins and fats may be added to the diet in sufficient quantities to provide energy for the economic burdens of life." - Frederick Banting
The discovery of insulin earned Banting and John Macleod, who supervised the research, the Nobel Prize in Physiology or Medicine in 1923. This achievement underscores the profound impact of their work on medical science and patient care.
Rosalind Yalow: Revolutionizing Hormone Measurement
Rosalind Yalow, a physicist by training, made seminal contributions to endocrinology through her development of the radioimmunoassay (RIA) technique. This method allowed for the precise measurement of hormones in the blood, revolutionizing the diagnosis and treatment of endocrine disorders.
Yalow's work, conducted in collaboration with Solomon Berson, enabled the detection of minute quantities of hormones, such as insulin and growth hormone. This advancement facilitated a deeper understanding of hormonal regulation and paved the way for numerous clinical applications. In recognition of her contributions, Yalow was awarded the Nobel Prize in Physiology or Medicine in 1977.
Fuller Albright: The Father of Modern Endocrinology
Fuller Albright is often regarded as the father of modern endocrinology. His extensive research on calcium metabolism, parathyroid hormone, and other endocrine functions laid the groundwork for contemporary endocrinology. Albright's work at Massachusetts General Hospital and Harvard Medical School significantly advanced the understanding and treatment of endocrine disorders.
Among his many contributions, Albright described Albright's hereditary osteodystrophy, a genetic disorder characterized by hormone resistance and skeletal abnormalities. His meticulous clinical observations and research methodologies set a high standard for future endocrinologists.
Modern Innovators in Endocrinology
Building on the foundations laid by historical pioneers, modern scientists continue to make groundbreaking discoveries in endocrinology. These innovators leverage advanced technologies and interdisciplinary approaches to tackle complex endocrine disorders and develop novel therapies.
Jeffrey Friedman: Unraveling the Mysteries of Obesity
Jeffrey Friedman, a geneticist and molecular biologist, has made significant strides in understanding the genetic and molecular basis of obesity. His discovery of the leptin hormone in 1994 revolutionized the field, providing critical insights into the regulation of body weight and appetite.
Leptin, produced by fat cells, plays a crucial role in signaling satiety to the brain. Friedman's research demonstrated that mutations in the leptin gene could lead to severe obesity, highlighting the hormone's importance in energy balance. This discovery opened new avenues for researching obesity treatments and metabolic disorders.
Shlomo Melmed: Advancing Pituitary Research
Shlomo Melmed, a renowned endocrinologist, has dedicated his career to the study of pituitary disorders. His research on acromegaly and Cushing's disease has significantly improved the diagnosis and treatment of these conditions. Melmed's work on the molecular mechanisms underlying pituitary tumors has led to the development of targeted therapies.
As the Executive Vice President and Dean of the Medical Faculty at Cedars-Sinai Medical Center, Melmed has also been instrumental in advancing medical education and research. His contributions have earned him numerous accolades, including the Endocrine Society's Fred Conrad Koch Award, one of the highest honors in the field.
Barbara Kahn: Exploring the Link Between Obesity and Diabetes
Barbara Kahn, a leading researcher in metabolism and endocrinology, has focused her work on the interplay between obesity and type 2 diabetes. Her studies on insulin resistance and the role of adipose tissue in metabolic regulation have provided valuable insights into the pathogenesis of diabetes.
Kahn's research has highlighted the importance of brown adipose tissue in energy expenditure and metabolic health. Her findings have implications for developing new therapies to combat obesity and its associated metabolic disorders. Kahn's contributions have been recognized with numerous awards, including election to the National Academy of Medicine.
The Impact of Revolutionary Discoveries in Endocrinology
The contributions of revolutionary scientists in endocrinology have had a profound impact on medical practice and patient outcomes. From the discovery of insulin to the development of advanced diagnostic techniques, these breakthroughs have transformed the management of endocrine disorders.
Transforming Diabetes Management
The discovery of insulin by Banting and Best marked a turning point in the treatment of diabetes. Before insulin therapy, diabetes was a fatal condition, with patients surviving only a few years after diagnosis. Today, insulin therapy allows individuals with diabetes to lead long, healthy lives.
Advancements in insulin delivery systems, such as insulin pumps and continuous glucose monitors (CGMs), have further improved diabetes management. These technologies provide real-time data and precise insulin dosing, enhancing patient quality of life and reducing the risk of complications.
Advancing Hormone Replacement Therapies
The development of hormone replacement therapies (HRT) has significantly improved the treatment of various endocrine disorders. For example, thyroid hormone replacement therapy has transformed the management of hypothyroidism, a condition characterized by an underactive thyroid gland.
Similarly, growth hormone therapy has benefited individuals with growth hormone deficiencies, enabling normal growth and development. These therapies underscore the importance of hormonal balance in maintaining overall health and well-being.
Enhancing Diagnostic Precision
The introduction of advanced diagnostic techniques, such as radioimmunoassay (RIA) and enzyme-linked immunosorbent assay (ELISA), has revolutionized the detection and measurement of hormones. These methods allow for the precise quantification of hormone levels, facilitating accurate diagnoses and tailored treatment plans.
Modern imaging technologies, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), have further enhanced the diagnosis of endocrine disorders. These tools provide detailed insights into the structure and function of endocrine glands, aiding in the identification of tumors and other abnormalities.
Future Directions in Endocrinology Research
The field of endocrinology continues to evolve, with ongoing research focusing on innovative therapies and technologies. Emerging trends, such as personalized medicine and gene therapy, hold promise for further advancing the treatment of endocrine disorders.
Personalized Medicine and Precision Endocrinology
Personalized medicine aims to tailor medical treatments to individual characteristics, such as genetic makeup and lifestyle factors. In endocrinology, this approach can enhance the effectiveness of hormone therapies and minimize adverse effects.
For example, genetic testing can identify specific mutations that affect hormone production or receptor function. This information can guide the development of targeted therapies, improving patient outcomes. Precision endocrinology represents a significant step forward in the management of complex endocrine disorders.
Gene Therapy and Hormonal Disorders
Gene therapy holds potential for treating genetic endocrine disorders by correcting underlying genetic defects. This approach involves introducing functional genes into cells to replace or supplement faulty genes, restoring normal hormonal function.
Research in gene therapy for conditions such as congenital adrenal hyperplasia (CAH) and growth hormone deficiencies is ongoing. While challenges remain, the progress in this field offers hope for future breakthroughs in endocrine disorder management.
Artificial Intelligence and Endocrine Research
The integration of artificial intelligence (AI) in medical research is transforming the field of endocrinology. AI algorithms can analyze vast datasets, identifying patterns and predicting outcomes with high accuracy. This capability enhances the diagnosis and treatment of endocrine disorders.
For instance, AI-powered tools can assist in interpreting complex imaging data, detecting subtle abnormalities that may be missed by human observers. Additionally, AI can optimize hormone therapy regimens, improving treatment efficacy and patient adherence.
Conclusion: Celebrating the Legacy of Revolutionary Scientists
The field of endocrinology has been shaped by the contributions of revolutionary scientists who have dedicated their careers to advancing our understanding of hormonal regulation and disorders. From historical pioneers like Banting and Yalow to modern innovators like Friedman and Melmed, these individuals have transformed medical practice and improved patient outcomes.
As we look to the future, emerging technologies and research trends hold promise for further advancements in endocrinology. By building on the legacy of these groundbreaking scientists, the field will continue to evolve, offering new hope and solutions for individuals with endocrine disorders.
In the final part of this article, we will explore the practical applications of these discoveries and provide insights into how patients and healthcare providers can leverage these advancements for better health outcomes.
Practical Applications of Endocrinology Breakthroughs
The groundbreaking discoveries in endocrinology have translated into tangible benefits for patients worldwide. These practical applications of endocrine research have transformed diagnostic approaches, treatment modalities, and patient care strategies, significantly improving quality of life for individuals with hormonal disorders.
Clinical Implementation of Insulin Therapies
The discovery of insulin by Banting and Best has evolved into sophisticated insulin delivery systems that have revolutionized diabetes management. Modern insulin therapies include:
- Rapid-acting insulin analogs that mimic natural insulin response
- Long-acting basal insulins providing consistent background coverage
- Insulin pump therapy for precise, continuous insulin delivery
- Closed-loop systems (artificial pancreas) automating insulin dosing
These advancements have dramatically improved glycemic control while reducing the risk of hypoglycemia. The DCCT (Diabetes Control and Complications Trial) demonstrated that intensive insulin therapy reduces diabetes complications by 50-75%, underscoring the life-changing impact of these treatments.
Thyroid Disorder Management Innovations
Revolutionary research in thyroid endocrinology has led to transformative approaches in managing thyroid disorders:
- Levothyroxine formulations with improved bioavailability
- Thyroid ultrasound and fine-needle aspiration for precise diagnosis
- Radioactive iodine therapy for hyperthyroidism treatment
- Molecular testing for thyroid cancer classification
These innovations have enabled earlier diagnosis and more targeted treatments. For instance, the introduction of liothyronine (T3) therapy has provided alternatives for patients who don't respond well to traditional levothyroxine treatment, improving symptom management and quality of life.
Reproductive Endocrinology Advancements
The field of reproductive endocrinology has seen remarkable progress, with applications that have transformed fertility treatments:
- In vitro fertilization (IVF) with improved success rates
- Gonadotropin therapies for ovulation induction
- Preimplantation genetic testing for embryo selection
- Fertility preservation techniques for cancer patients
These breakthroughs have given hope to millions struggling with infertility. The development of aromatase inhibitors for ovulation induction has been particularly impactful, offering a more effective alternative to traditional clomiphene citrate with fewer side effects.
Patient-Centered Approaches in Modern Endocrinology
Contemporary endocrinology emphasizes patient-centered care, integrating the latest research with individualized treatment plans. This approach recognizes that each patient's hormonal balance is unique and requires personalized management strategies.
Shared Decision-Making in Treatment Plans
Modern endocrine practice prioritizes shared decision-making, where patients and healthcare providers collaborate to develop optimal treatment strategies. This approach includes:
- Comprehensive patient education about hormonal disorders
- Discussion of treatment options with their benefits and risks
- Consideration of patient preferences and lifestyle factors
- Regular monitoring and adjustment of treatment plans
Studies have shown that patient engagement in treatment decisions leads to better adherence and improved outcomes. For example, in diabetes management, patients who actively participate in their care achieve better glycemic control and experience fewer complications.
Integrative Endocrinology: Combining Conventional and Complementary Approaches
The emerging field of integrative endocrinology combines evidence-based conventional treatments with complementary approaches to optimize patient outcomes. This may include:
- Nutritional interventions to support hormonal balance
- Stress management techniques for adrenal health
- Exercise programs tailored to metabolic needs
- Mind-body therapies for overall endocrine wellness
Research has demonstrated that lifestyle modifications can significantly impact endocrine health. For instance, the Diabetes Prevention Program showed that lifestyle changes reduced the incidence of type 2 diabetes by 58% in high-risk individuals.
Global Impact of Endocrine Research
The revolutionary discoveries in endocrinology have had a profound global impact on public health, addressing some of the most prevalent and challenging health conditions worldwide.
Addressing the Diabetes Epidemic
With over 463 million adults living with diabetes worldwide (IDF 2019), the global burden of this endocrine disorder is substantial. The advancements in diabetes research have led to:
- Improved diagnostic criteria and screening methods
- Development of new drug classes like SGLT2 inhibitors and GLP-1 receptor agonists
- Enhanced diabetes education programs
- Global initiatives for diabetes prevention and management
These efforts have contributed to better disease management and reduced complications. The WHO Global Diabetes Compact aims to improve diabetes care globally, with targets to increase diagnosis rates and access to affordable insulin.
Combating Obesity Through Endocrine Understanding
The obesity epidemic, affecting over 650 million adults worldwide, is closely linked to endocrine dysfunction. Research in this area has led to:
- Identification of hormonal pathways regulating appetite and metabolism
- Development of pharmacological treatments for obesity
- Understanding of the gut-brain axis in weight regulation
- Personalized approaches to obesity management
The discovery of leptin and subsequent research on appetite-regulating hormones have opened new avenues for obesity treatment. Recent approvals of medications like semaglutide for weight management demonstrate the practical applications of this research.
Challenges and Future Opportunities
Despite the remarkable progress in endocrinology, significant challenges in endocrine research persist, presenting opportunities for future innovation and discovery.
Unmet Needs in Endocrine Disorder Management
Several areas in endocrinology require further research and development:
- Type 1 diabetes cure research and beta cell regeneration
- Improved treatments for rare endocrine disorders
- Better understanding of endocrine disruptors and environmental impacts
- Personalized hormone replacement therapies
For instance, while insulin therapy has been life-saving, it remains a treatment rather than a cure for type 1 diabetes. Ongoing research into islet cell transplantation and stem cell therapies holds promise for more definitive solutions.
Health Disparities in Endocrine Care
Addressing health disparities in endocrine care remains a critical challenge. Disparities exist in:
- Access to endocrine specialists and advanced treatments
- Diabetes prevalence and complications across different populations
- Thyroid disease diagnosis and management in underserved communities
- Reproductive endocrine services availability
Efforts to reduce these disparities include telemedicine initiatives, community health programs, and targeted education campaigns. The American Diabetes Association's Health Equity Now initiative aims to address these gaps through advocacy and research.
Conclusion: The Enduring Legacy of Endocrine Pioneers
The journey through the history and modern advancements of endocrinology reveals a field transformed by revolutionary scientists whose discoveries continue to shape medical practice today. From the life-saving discovery of insulin to the sophisticated hormone therapies of the 21st century, each breakthrough has built upon the foundations laid by pioneering researchers.
Key takeaways from this exploration include:
- The transformative impact of endocrine discoveries on patient care
- The evolution from basic research to clinical applications
- The importance of personalized medicine in endocrinology
- The global health implications of endocrine research
- The ongoing challenges that present opportunities for future innovation
As we reflect on the contributions of figures like Banting, Yalow, and Friedman, we recognize that their work extends far beyond individual discoveries. These scientists have collectively advanced our understanding of the complex hormonal systems that regulate human health, providing the tools and knowledge to combat some of the most prevalent diseases of our time.
The future of endocrinology holds immense promise, with emerging technologies like gene therapy, artificial intelligence, and precision medicine poised to deliver the next generation of breakthroughs. As research continues to unravel the mysteries of hormonal regulation, we can anticipate even more effective treatments, earlier diagnoses, and ultimately, improved health outcomes for millions worldwide.
In the spirit of the revolutionary scientists who have shaped this field, the pursuit of knowledge in endocrinology remains as vital today as it was a century ago. Their legacy challenges us to continue pushing the boundaries of medical science, ensuring that the benefits of endocrine research reach every individual in need.