Unmasking the Hidden Epidemic: The Rise of Antimicrobial Resistance
In the global health landscape, a silent threat looms large, one that is pervasive and relentless. This threat is not a novel virus or a resurgence of a forgotten disease, but rather a phenomenon known as antimicrobial resistance (AMR). The alarm bells have been ringing for some time, and yet the urgency to act seems to be muffled by the cacophony of other immediate health crises. The fact remains, however, that AMR is a complex health challenge that could redefine our relationship with medicine and the microbial world.
The concept of antimicrobial resistance is straightforward: it occurs when microorganisms such as bacteria, viruses, fungi, and parasites change in response to the use of medications meant to kill or inhibit them, becoming 'resistant' and continuing to multiply even in the presence of these drugs. The repercussions of such a phenomenon are grave; infections become harder to treat, the risk of disease spread, severe illness, and death is increased, and medical procedures that we take for granted—such as surgeries, chemotherapy, and organ transplants—become exceedingly risky.
Why is AMR on the rise, you might ask? The causes are multifaceted and intertwined, encompassing the mismanagement of prescribed medications, over-the-counter sale of antibiotics, lack of regulatory measures, inappropriate use in agriculture, and insufficient new drugs in the development pipeline. The use of antimicrobials in livestock to promote growth and the usage in crop protection further exacerbates the problem, circulating resistant strains through the food chain and environment.
One of the pivotal issues is the misuse and overuse of antibiotics, which are often prescribed for viral infections against which they have no effect. The eagerness to 'do something' against illnesses leads to a culture of expectation that for every cough and sniffle, antibiotics are the answer. This misuse gives bacteria the perfect training ground to adapt and outwit our pharmaceutical arsenal. Globally, varying access to quality healthcare and differences in prescription practices compound the challenge. In some regions, patients may be unable to complete a full course of antibiotics due to cost, leading to partial treatment that fuels resistance.
Moreover, the pipeline for new drugs to combat resistant strains is dishearteningly sparse. Pharmaceutical research and development are lagging in the antimicrobial space, mainly because such developments are not as profitable as chronic disease drugs and because of the inherent scientific challenge in outrunning microbial evolution. The World Health Organization’s list of bacteria for which new antibiotics are urgently needed grows, yet the market does not respond with equal urgency.
The COVID-19 pandemic has brought additional insight into the issue of AMR. The widespread and sometimes indiscriminate use of antibiotics to treat secondary bacterial infections in COVID-19 patients, and disruptions in routine healthcare, have likely propelled AMR even further. If parallels can be drawn, the pandemic has shown us that global health threats require global responses, collaboration, and preparedness that transcend borders and sectors.
As the world leans into a post-pandemic phase, we must not lose the momentum to confront the hazards of antimicrobial resistance. It is a problem that requires a multi-pronged approach, engaging government policies, healthcare practices, pharmaceutical innovation, public awareness, and individual behavior. We stand at a critical junction where our actions or inactions will carve the path for the future of global health, making AMR an inescapable topic for discussion and action.
Part two of this article will delve deeper into the strategies to combat antimicrobial resistance, the innovative efforts underway, and what each of us can do to contribute to the fight against this hidden epidemic.
The Battle Against Antibiotic Resistance: Strategies and Solutions
Understanding that antimicrobial resistance is a multidimensional threat requires an equally multifaceted response. Combating AMR is not a responsibility that falls on healthcare professionals alone; it requires a concerted effort from multiple stakeholders including policymakers, agricultural sectors, pharmaceutical companies, and the public at large.
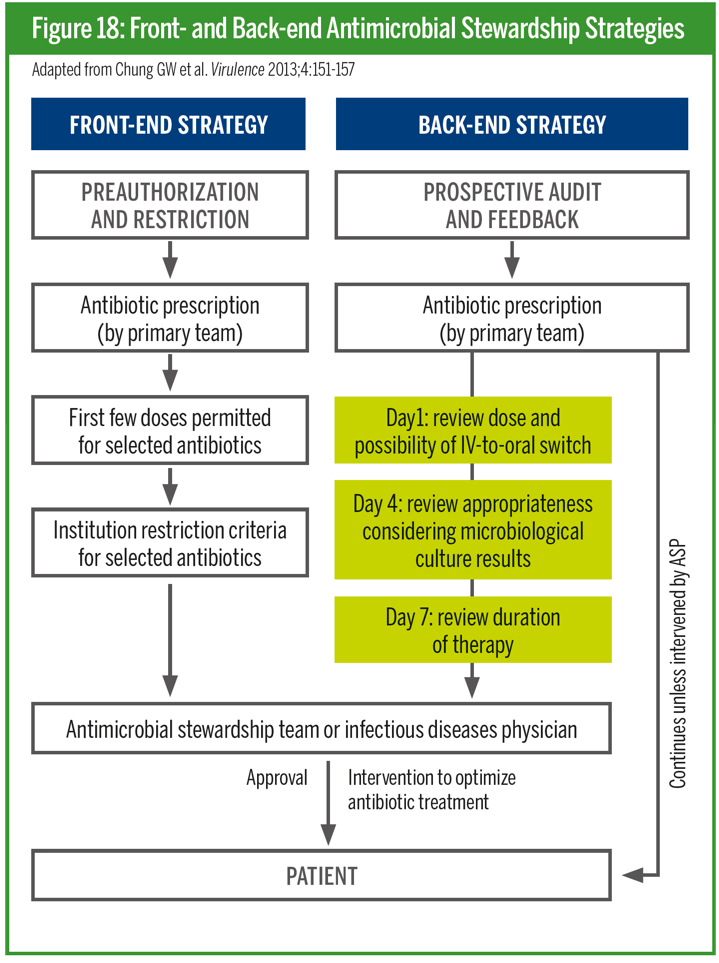
Firstly, one of the most critical defenses against AMR is the development and enforcement of stringent antibiotic stewardship programs. These are initiatives designed to optimize the use of antimicrobials to treat infections, ensuring that the right drug, dose, and duration are prescribed. Healthcare providers play a vital role here. By adhering to these practices, they not only improve patient care but also reduce unnecessary exposure to antimicrobials, thus decreasing the development of resistance.
Education and public awareness campaigns are foundational in altering the perception and use of antibiotics among the general public. By understanding that antibiotics are not a cure-all for infections, especially viral ones like the cold or flu, individuals can reduce pressure on healthcare providers to prescribe them. Additionally, increasing awareness of the importance of completing prescribed antibiotic courses and not sharing or using leftover drugs can significantly diminish misuse.
On a policy level, governments must prioritize AMR as a national and international health concern. This can be done by integrating action plans that span healthcare, veterinary, agriculture, and environmental sectors—known as the One Health approach. By monitoring and regulating the sales and distribution of antibiotics, countries can better control inappropriate consumption. In tandem, strengthening regulatory frameworks to eliminate the addition of antibiotics in animal feed used as growth promoters is imperative.
In the pharmaceutical domain, economic incentives can play a part in stimulating R&D for new antibiotics and alternative treatments. Governments and international organizations could consider options such as tax incentives, subsidies, or a global innovation fund to de-risk the financial aspect of antibiotic development. Also, encouraging innovation beyond traditional antibiotics, such as phage therapy, immunotherapies, and novel anti-infectives, ensures diversity in our treatment options and a broader strategy against resistance.
On the agricultural front, the reduction of antibiotic use is critical. Farmers should be encouraged and supported to move away from preventive antibiotic use and instead focus on improving hygiene, animal welfare, and using vaccines to keep animals healthy. Surveillance systems can monitor and reduce the levels of resistance within both human and animal populations.
In combating AMR, diagnostics play a pivotal role as well. Rapid diagnostic tests that accurately identify the cause of an infection can greatly help in ensuring that antibiotics are only used when necessary and that the appropriate treatment is provided. Research in better diagnostics must be funded and promoted to make these tools widespread and accessible.
More efforts should also be made to tackle environmental hotspots of resistance such as wastewater from hospitals and pharmaceutical manufacturing, which can disseminate resistant bacteria into the wider environment. Improving waste treatment processes and implementing stricter controls on industrial discharges can aid in reducing the spread of resistance genes.
Lastly, at an individual level, actions like handwashing, good hygiene practices, proper vaccination, and avoiding the overuse of antibacterial products can help reduce the likelihood of infection and the subsequent need for antibiotics.
The war on antimicrobial resistance is one that cannot be won overnight. It demands patience, innovation, and a sustained international commitment. The future of our health, and indeed the efficacy of medical advancements we have come to rely on, depends on the effectiveness of our collective actions today. AMR may well be the defining health crisis of our generation, and rising to meet this challenge is a necessity, not a choice. As we move forward, it is the collaborative efforts across disciplines and borders that will help preserve the therapeutic value of antimicrobial drugs and safeguard human health for generations to come.





Comments